Fungal infection can present as a tumor lesion without any predisposing factor
Dr. Rajlaxmi Reddy, Department of Orthopaedics, Sree Balaji Medical College and Hospital, Chrompet - 600044, Chennai, Tamil Nadu, India. E-mail: saiprasadeng@gmail.com
Introduction: Fibrous dysplasia is a rare, benign bone disorder characterized by fibro-osseous replacement of normal bone.
Case Report: We report the case of a 22-year-old female who presented with chronic left arm pain and a history of pathological fracture of the left humerus. Radiological imaging revealed an ill-defined intramedullary mixed sclerotic and lytic lesion suggestive of fibrous dysplasia. The patient underwent bone curettage and grafting, and the sample was sent for histopathological examination. Surprisingly, the histology showed fungal spores, with no evidence of neoplasia. The patient had no known immunocompromised state or predisposing factors.
Conclusion: This case emphasizes the importance of considering rare infectious causes such as fungal osteomyelitis in the differential diagnosis of tumor-like bone lesions, even in immunocompetent individuals. Early tissue diagnosis is critical to avoid mismanagement and to initiate appropriate antifungal treatment.
Keywords: Fibrous dysplasia, pathological fracture, fungal growth, humerus, intramedullary, bone curettage, grafting.
Fibrous dysplasia is a typically non-malignant bone lesion which is characterized by intramedullary fibro-osseous proliferation secondary to altered osteogenesis, i.e., failure to form mature lamellar bone and arrest as woven bone. It occurs either in monostotic or polyostotic form [1,2]. Adult presentation often occurs incidentally during imaging for an unrelated indication. Fibro-osseous replacement of bone can lead to pathologic fracture, especially in weight-bearing bones or the upper extremities in athletes. Malignant transformation is rare [3,4]. Fibrous dysplasia is characterized by tumor-like proliferation of fibro-osseous tissue and can look like anything, but most commonly presents as a long lesion in a long bone. It is often purely lytic and takes on a ground-glass look as the matrix calcifies. In many cases, there is bone expansion and bone deformity. If periosteal reaction or pain is present, exclude fibrous dysplasia, unless there is a fracture [5]. A fungal infection of bone is more common in immunocompromised patients, commonly in older patients. Patients usually do not present with typical features of bone infection and are often diagnosed late. Clinical suspicion of fungal infection is mandatory to avoid complications in later stages [6]. Although fungal osteomyelitis is typically seen in immunocompromised individuals, its occurrence in healthy young adults is exceedingly rare and often mimics other bone pathologies such as fibrous dysplasia. In this report, we present a rare and unusual case of a healthy young female initially diagnosed radiologically as fibrous dysplasia, which was later confirmed histopathologically to be a fungal bone infection. This case is reported to highlight the diagnostic challenges and the importance of considering fungal infections in the differential diagnosis of tumor-like bone lesions, even in immunocompetent individuals.
Case Report [12]
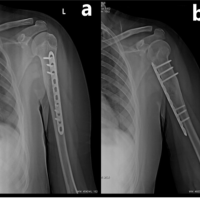
A 22-year-old female patient presented with complaints of pain in her left arm on and off for the past 2 years, which had been aggravated over the last 1 month. Pain is an insidious, progressive, non-radiating, dull aching type, aggravated on physical activity, relieved on rest. Patient had an alleged history of trauma 6 years back (skid and fall at her residence) sustaining injury to left arm and diagnosed to have a humerus fracture and lytic lesion. For which she was treated conservatively at an outside hospital. After 2 months of the fracture, the patient sustained again fracture over the same site and opted for conservative treatment. After 2 months of refracture aspiration (~50 mL) under CARM Guidance at SBMCH was done. On examination, no scar, sinus, or obvious swelling was noted. No soft tissue/bony tenderness seen. Range of motion (shoulder and elbow) was full and free without distal neurovascular deficit (DNVD). Blood investigations were carried out and found to be normal. X-ray (Fig. 1) showed mixed ill-defined lytic expansile lesions with a narrow zone of transition over the proximal 2/3rd of the left humerus. After the surgical procedure, the curettage bone was sent for histopathology (Fig. 2) and reported as fungal infection.
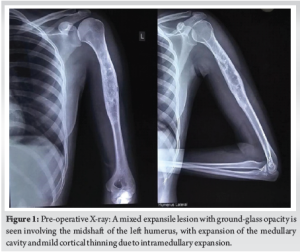
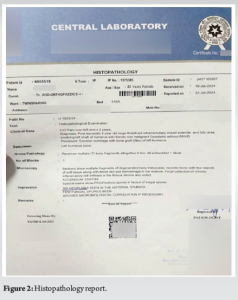
This case was reported due to its rarity and diagnostic complexity. While fibrous dysplasia is a known benign lesion with distinct radiological features, this case demonstrates that fungal infections can closely mimic such lesions both clinically and radiographically. The unexpected histopathological finding of fungal spores in an immunocompetent patient underscores the importance of maintaining a broad differential diagnosis when evaluating bone lesions. The incidence of fungal infection of bones and joints is usually low and rare. Invasive fungal infections are more likely to be associated with a rising population of immunosuppressed patients [7], and are also seen in patients with several comorbid conditions. Patients under steroid treatment are likely to be immunosuppressed and are prone to acquiring infections. Species such as Candida and Aspergillus are the most common causative organisms [8]. Candida, being an endemic dimorphic fungus, is accountable for an enormous number of cases globally. Fungal infections are commonly transmitted through the hematogenous route. Transmission from contiguous infection, or by direct inoculation following trauma or surgery, is also noted. Clinically, adults present with mild features, often without fever or a rise in inflammatory markers. Children may have features of vertebral osteomyelitis, which differ from adult presentations [9]. Due to the dormant nature of symptoms in adults, diagnosis is often delayed. Diagnosis is based on tissue culture, tissue histology, and clinical correlations. In this case, the X-ray findings (Fig. 1, 2) mimicked fibrous dysplasia, showing a mixed expansile lesion with ground-glass opacity. The patient was clinically and radiologically (Fig. 3-5) diagnosed to have fibrous dysplasia. However, histological examination revealed a fungal infection. Therefore, to avoid misdiagnosis, tissue culture and histology are necessary in similar presentations. Once diagnosed, appropriate antifungal medication and often surgical debridement are required.
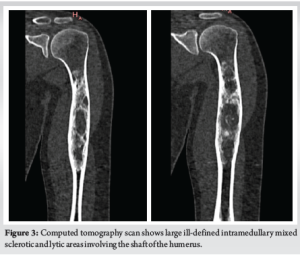
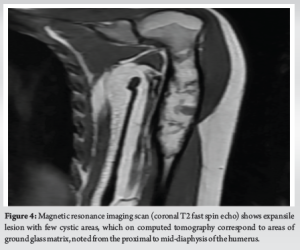

Fibrous dysplasia is characterized by the replacement of mature bone marrow with an immature abnormal matrix by fibro-osseous growth. Due to somatic mutation, it affects woven bone and leads to failure of turning into lamellar bone [10]. This condition often has no symptoms and is an incidental finding, usually presenting as a pathological fracture. Radiographically, a clearly circumscribed lesion with a narrow zone of transition can be appreciated. Computed tomography and magnetic resonance imaging (Fig. 3-6) are also found to be useful. Fibrous dysplasia is mostly treated symptomatically – such as managing pathological fractures or with simple palliative care [11,12]. Curettage, bone grafting, and fixation techniques are also used for the correction of deformities. Medically, bisphosphonates may be supplemented with other supportive treatments.
In our case report, a 22-year-old female patient diagnosed with post-traumatic, 6-year-old large ill-defined intramedullary mixed sclerotic and lytic area involving the left shaft of the humerus with non-malignant fibrous dysplasia without DNVD. For this, bone curettage and grafting were done under general anaesthesia. Curated sample sent to histopathological examination (HPE). HPE reports (Fig. 2) showed few fungal spores and no neoplasia. We concluded that even fungal infection can present as a tumor lesion and is often misdiagnosed and treated accordingly. Hence, fungal infection should be ruled out even in a healthy individual, even though it is more common in immunocompromised individuals to avoid complications.
Fungal infection can present as a tumor lesion and is often misdiagnosed and treated accordingly. Hence, fungal infection should be ruled out even in a healthy individual, even though it is more common in immunocompromised individuals to avoid complications.
References
- 1.DiCaprio MR, Enneking WF. Fibrous dysplasia. Pathophysiology, evaluation, and treatment. J Bone Joint Surg Am 2005;87:1848-64. [Google Scholar | PubMed]
- 2.Chika AT, Philomena IM. Fibrous dysplasia of the humerus: An uncommon cause of pathological fracture in a 56-year-old. Niger J Surg Res 2016;17:17-9. [Google Scholar | PubMed]
- 3.Stanton RP, Ippolito E, Springfield D, Lindaman L, Wientroub S, Leet A. The surgical management of fibrous dysplasia of bone. Orphanet J Rare Dis 2012;7 Suppl 1:S1. [Google Scholar | PubMed]
- 4.Parekh SG, Donthineni-Rao R, Ricchetti E, Lackman RD. Fibrous dysplasia. J Am Acad Orthop Surg 2004;12:305-13. [Google Scholar | PubMed]
- 5.Campanacci M, Laus M. Osteofibrous dysplasia of the tibia and fibula. J Bone Joint Surg Am 1981;63:367-75. [Google Scholar | PubMed]
- 6.Hahn SB, Kim SH, Cho NH, Choi CJ, Kim BS, Kang HJ. Treatment of osteofibrous dysplasia and associated lesions. Yonsei Med J 2007;48:502-10. [Google Scholar | PubMed]
- 7.Solooki S, Keikha Y, Vosoughi AR. Can ethanol be used as an adjuvant to extended curettage in order to reduce the recurrence rate of aneurysmal bone cyst? Rev Bras Ortop 2017;52:349-53. [Google Scholar | PubMed]
- 8.Cha SM, Shin HD, Kim KC, Park IY. Extensive curettage using a high-speed burr versus dehydrated alcohol instillation for the treatment of enchondroma of the hand. J Hand Surg Eur Vol 2015;40:384-91. [Google Scholar | PubMed]
- 9.Ozer B, Kalaci A, Duran N, Dogramaci Y, Yanat AN. Cutaneous infection caused by Aspergillus terreus. J Med Microbiol 2009;58:968-70. [Google Scholar | PubMed]
- 10.Myoken Y, Sugata T, Fujita Y, Kyo T, Fujihara M, Kohara T, et al. Molecular epidemiology of invasive stomatitis due to Aspergillus flavus in patients with acute leukemia. J Oral Pathol Med 2003;32:215-8. [Google Scholar | PubMed]
- 11.Hedayati MT, Pasqualotto AC, Warn PA, Bowyer P, Denning DW. Aspergillus flavus: Human pathogen, allergen and mycotoxin producer. Microbiology (Reading) 2007;153:1677-92. [Google Scholar | PubMed]
- 12.Mahabier KC, Vogels LM, Punt BJ, Roukema GR, Patka P, Van Lieshout EM. Humeral shaft fractures: Retrospective results of non-operative and operative treatment of 186 patients. Injury 2013;44:427-30. [Google Scholar | PubMed]