Reconstruction of the proximal brachial triceps using a homologous tensor fascia lata graft can significantly enhance both esthetic and functional outcomes in patients with extensive muscle loss.
Dr. Eduardo Borges Ferreira Jr, Santa Casa de Misericórdia de São Paulo, Santa Casa de Misericórdia de São Paulo, Department of Orthopedics and Traumatology, “Fernandinho Simonsen” Pavilion, Rua Dr. Cesário Mota Júnior, 112 - Vila Buarque, São Paulo, Brazil. E-mail: eduardobfj2@gmail.com
Introduction: Injuries to the brachial triceps (BT) tendon are rare, accounting for about 1% of all tendon injuries. The complexity of these injuries, especially in their proximal portion, and the scarcity of data in the literature make each case essential to expand knowledge. This report demonstrates an effective treatment method for extensive muscle loss around the shoulder using a homologous graft, offering new perspectives for similar cases.
Case Report: A 65-year-old female patient presented with a history of desmoid tumor treated surgically through an extensive surgical resection of the proximal portion of the BT muscle, followed by a third-degree burn in the left scapular region. The patient exhibited sequelae, manifesting complaints related to esthetics and reduced active extension of the elbow. Hypotrophy of the deltoid muscle was also observed, associated with paresthesia in the corresponding C5 dermatome. The patient underwent surgical treatment for reconstruction of the proximal portion of the BT muscle using a homologous graft from the tensor fascia lata muscle, which resulted in esthetic and functional improvements without additional neurological deficits.
Conclusion: The case report demonstrates that reconstruction of the proximal portion of the BT muscle with a homologous graft is a promising approach for treating this type of injury, bringing significant improvements in muscle function and esthetics. Furthermore, a multidisciplinary approach, postoperative surveillance, and the continuous pursuit of technical advancements are essential to optimize results and minimize complications, broadening therapeutic options in complex cases.
Keywords: Muscle reconstruction, graft, brachial triceps.
Injuries to the brachial triceps (BT) muscle tendon are rare events, accounting for approximately 1% of all tendon injuries and are poorly documented in the literature [1,2]. Often, these injuries result from a fall with an extended wrist, vigorous eccentric contraction of the triceps, direct trauma to the elbow, or lifting against resistance [3,4]. They pose significant problems that, if untreated, can cause profound disability, especially among athletes [5]. The lack of data on these injuries complicates the development of effective therapeutic strategies, particularly for the proximal portion of the BT. Predominantly, studies focus on the distal portion of the BT as it is more common, exploring diagnostic and therapeutic options [1,6]. The identification of tears in the triceps tendon often presents as a diagnostic challenge, especially in the early stages due to swelling and pain [7,8]. The study by van Riet et al. highlighted that magnetic resonance imaging is effective in demonstrating tendon integrity or the site of the tear [7]. Furthermore, Tagliafico et al. (2011) demonstrated that ultrasound can be used in assessing injuries to the distal triceps tendon, being capable of differentiating complete from partial triceps tears [9]. However, prior experience with the ultrasound technique is required for greater diagnostic efficacy [9]. Recent studies have investigated the efficacy of different therapeutic approaches for injuries to the distal triceps tendon [7,10]. Alnaji et al. analyzed the outcomes and complications associated with various surgical techniques used in the primary repair of tears in the BT muscle tendon [10]. The study reported that the distribution of complications was 29.2% for the direct repair technique, 15.2% for the transosseous technique, and 7.7% for the suture anchor technique [10]. However, due to heterogeneity in tear patterns, surgical procedures, and outcome measures, it was not possible to determine the superiority of a specific technique over others [10]. Regarding the distal BT, Van Riet et al. explored various surgical approaches to treat tears of the distal triceps tendon [7]. In 22 patients, 23 procedures were performed, in which techniques varied between direct repair, used in fourteen cases, and reconstruction, applied in nine cases, using autologous tendon grafts from the Achilles, plantar, semitendinosus, latissimus dorsi, anconeus, and palmaris longus in six cases [7]. In each case of reconstruction, the transferred tendon was interlaced with the distal stump of the triceps and sutured with transosseous stitches [7]. In the present case report, the same technique was used, however, employing a homologous fascia lata graft instead of an autologous one, and occurring in different portions of the BT muscle. This case report aims to demonstrate an alternative for cases of significant muscle loss around the shoulder, aiming for functional and esthetic improvements.
Female patient, 65 years old, right-handed, an administrator, with a history of desmoid tumor in the left axillary region, underwent surgical treatment for tumor resection and chemotherapy in 2015. In 2016, she followed up with the plastic surgery team due to a 3rd° burn in the left scapular region, resulting from a domestic accident that year, caused by loss of sensation in the area following the previous surgical resection of the tumor. In 2018, after follow-ups and resolution of the skin condition from the burn, the patient complained during the physical examination of mild pain in the left shoulder and arm, with decreased active elbow extension, associated with bulging on the distal posterior face of the arm due to previous surgical intervention. The evaluation revealed deltoid muscle hypotrophy and functional loss of the latissimus dorsi muscle, associated with hypoesthesia at the level of the C5 dermatome, as well as an increase in volume in the distal and medial regions of the arm due to muscle retraction (Fig. 1). Despite these complications, she maintained good lateral rotation and shoulder elevation, due to an intact rotator cuff.

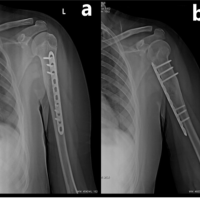
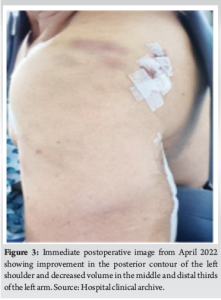
Still in 2018, the patient began stimulation with the EMSCULPT device (BTL Industries Inc., Boston, MA), which generates electromagnetic fields, aiming to improve muscle atrophy. However, she maintained the condition of progressive deltoid muscle hypotrophy and an increase in volume in the distal and medial region of the arm due to muscle retraction. In January 2021, the patient sought the Orthopedics and Traumatology of the Shoulder and Elbow team at the German Hospital Oswaldo Cruz, due to persistent symptoms. Radiographic images revealed a lowering of the humeral head, due to deltoid muscle hypotrophy (Fig. 2a). Magnetic resonance imaging of the arm showed a distal retraction of approximately eight centimeters of the lateral head of the triceps associated with deltoid muscle atrophy (Fig. 2b). In March 2022, a surgery for reconstruction of the proximal portion of the triceps with a homologous fascia lata graft was performed. Immediately postoperatively, improvement in the posterior contour of the left shoulder and a decrease in volume in the middle third of the left arm were noted, indicating a positive initial response to the intervention (Fig. 3). Two weeks after the procedure, local hyperemia and formation of a collection next to the distal incision were observed, and ultrasound sonography-guided puncture was performed, with subsequent improvement.
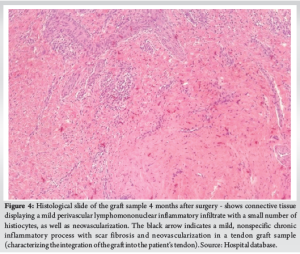
Four months after the surgery, the patient presented with a granuloma at the distal incision of the operative wound and underwent resection of it and removal of a sample of the tendon graft related to the granuloma, which was sent for anatomopathological evaluation. The connective tissue in the graft sample exhibited mild perivascular lymphomononuclear inflammatory infiltrate with a small number of histiocytes, in addition to neovascularization. This discrete nonspecific chronic inflammatory process with scar fibrosis and neovascularization characterized the integration of the graft into the patient’s tendon (Fig. 4).
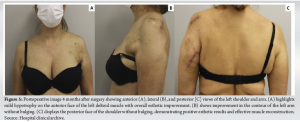
After these procedures, an improvement in esthetics was observed, absence of bulging on the posterior face of the left shoulder, better contour of the left arm, and slight visible hypotrophy on the anterior face of the left deltoid muscle (Fig. 5). The patient also showed clinical and functional improvement, with recovery of active elbow extension and was cleared to begin muscle strengthening.
Surgical procedure
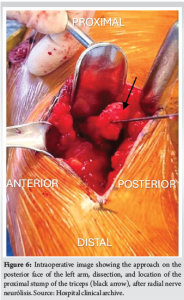
The patient was positioned in right lateral decubitus, and access was made on the posterior face of the left arm (Fig. 6), with dissection by layers and hemostasis. Neurólisis of the radial nerve, which was adhered to the BT. Dissection and release of the BT heads. Regarding the homologous fascia lata graft (Fig. 7), suturing was performed on the remaining triceps stump with polyester stitches size five (Fig. 8).

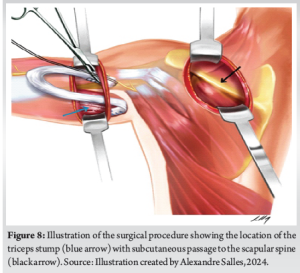
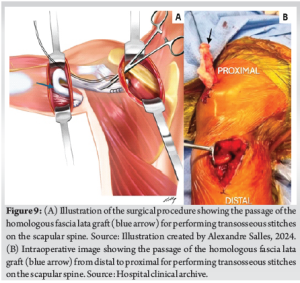
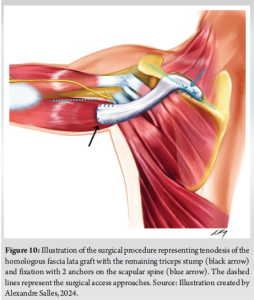
For the subcutaneous passage of the graft, another incision was made over the spine of the scapula, dissection by layers, and isolation of the spine. A tunnel was created from the spine of the scapula towards the triceps. Transfer of the graft (Fig. 9a and b) and suturing on the spine of the scapula with two anchors (Fig. 10). The remainder of the graft was taken back to the triceps and sutured over it (Fig. 10). Significant improvement in the deformity of the arm was observed. The patient remained immobilized with a simple sling for 4 weeks.
The case report presented reveals a series of clinical and therapeutic challenges, highlighting the complexity of management in cases with extensive muscular and tendinous injuries around the shoulder, as well as the importance of a multidisciplinary approach and the search for therapeutic alternatives. One of the most notable aspects of this case is the complexity and rarity of injuries to the BT tendon, especially in its proximal portion, which is poorly documented in the literature and, consequently, presents difficulties in treatment [1,2]. Recent studies have discussed the various surgical approaches to BT repair; however, due to heterogeneity in tear patterns, surgical procedures, and outcome measures, it has not been possible to determine the superiority of one specific technique over others [7,10]. In the case report presented, the patient exhibited significant retraction of the proximal portion of the BT, associated with the absence of the deltoid muscle, which negatively impacted her muscular function and esthetics. This condition is rare and requires specific and personalized approaches. The method used in this case, tenoplasty with a homologous tensor fascia lata muscle graft, stands out as a viable alternative for treating the described injury. The use of homologous grafts offers advantages, such as the absence of additional morbidity associated with obtaining autologous grafts. Furthermore, the surgical technique described demonstrates a precise and careful approach, with the graft being anchored, aiming for stable and lasting reconstruction. The integration of the graft was confirmed by histological evaluation, highlighting the integration of the transplanted tissue into the local muscular environment, which reinforces the effectiveness of this method. However, it is important to emphasize that the success of the procedure was not immediate, as the patient experienced postoperative complications, such as local hyperemia and the formation of a collection and granuloma at the distal incision. These complications highlight the challenges and the need for careful and vigilant postoperative follow-up. Nevertheless, there were no final clinical repercussions from these complications. The resolution of complications and the observed clinical and functional improvement 4 months after the surgical procedure highlight the efficacy of the intervention performed. The active extension of the elbow and the esthetic improvement achieved demonstrate the positive impact of the treatment on the patient’s quality of life. However, given the complexity of the case and the complications faced, it is essential to highlight the need for more studies and scientific work to improve muscle reconstruction techniques in similar cases. The investigation of new therapeutic approaches, as well as the analysis of risk factors and prognosis, are fundamental to improving outcomes and the safety of patients undergoing complex surgical procedures like this. In summary, this case report highlights not only the challenges faced in treating rare and complex muscle injuries but also the importance of a multidisciplinary approach, postoperative vigilance, and the continuous search for therapeutic alternatives and technical improvement.
This case report demonstrates the effectiveness of using a homologous tensor fascia lata graft for reconstructing complex muscle and tendon injuries around the shoulder, which reduces the morbidity associated with autologous graft harvesting. This innovative approach not only confirms the viability of homologous grafts in muscle reconstruction but also enriches our understanding of tissue integration techniques. The successful application in this rare condition holds significant implications for orthopedic surgery and potentially other medical fields involved in tissue recovery and repair.
This case report emphasizes the importance of alternative surgical approaches in managing complex injuries, particularly the use of homologous grafts for muscle and tendon reconstruction. Highlighting a method that reduces patient morbidity while ensuring effective recovery, this report offers valuable insights for orthopedic surgeons and other medical professionals dealing with similar challenges. The demonstrated success and multidisciplinary management approach make this case a critical read for those looking to improve surgical techniques and patient outcomes in muscle and tendon reconstructive surgeries.
References
- 1.Casadei K, Kiel J, Freidl M. Triceps tendon injuries. Curr Sports Med Rep 2020;19:367-72. [Google Scholar | PubMed]
- 2.Nawijn F, Emmink BL, Keizer J, Bosman WM. Complete triceps tendon rupture; a rare tendon injury. Ned Tijdschr Geneeskd 2018;162:D2744. [Google Scholar | PubMed]
- 3.Walker CM, Noonan TJ. Distal triceps tendon injuries. Clin Sports Med 2020;39:673-85. [Google Scholar | PubMed]
- 4.Gaviria M, Ren B, Brown SM, McCluskey LC, Savoie FH, Mulcahey MK. Triceps tendon ruptures: Risk factors, treatment, and rehabilitation. JBJS Rev 2020;8:e0172. [Google Scholar | PubMed]
- 5.Thomas JR, Lawton JN. Biceps and triceps ruptures in athletes. Hand Clin 2017;33:35-46. [Google Scholar | PubMed]
- 6.Kokkalis ZT, Ballas EG, Mavrogenis AF, Soucacos PN. Distal biceps and triceps ruptures. Injury 2013;44:318-22. [Google Scholar | PubMed]
- 7.Van Riet RP, Morrey BF, Ho E, O’Driscoll SW. Surgical treatment of distal triceps ruptures. J Bone Joint Surg Am 2003;85:1961-7. [Google Scholar | PubMed]
- 8.Yeh PC, Dodds SD, Smart RL, Mazzocca AD, Sethi PM. Distal triceps rupture. J Am Acad Orthop Surg 2010;18:31-40. [Google Scholar | PubMed]
- 9.Tagliafico A, Gandolfo N, Michaud J, Perez MM, Palmieri F, Martinoli C. Ultrasound demonstration of distal triceps tendon tears. Eur J Radiol 2012;81:1207-10. [Google Scholar | PubMed]
- 10.Alnaji O, Erdogan S, Shanmugaraj A, AlQahtani S, Prada C, Leroux T, et al. The surgical management of distal triceps tendon ruptures: A systematic review. J Shoulder Elbow Surg 2022;31:217-24. [Google Scholar | PubMed]