Spinous process osteotomy minimizes the injury to the tissues by preserving the paraspinal musculature and the interspinous and supraspinous ligament complex and facets. Spinal process osteotomy can be considered a modality of treatment for high lumbar disc disease in young patients without the need for spinal fusion.
Dr. Naveenkumar kuppan, Department of Orthopaedics, Sri Manakula Vinayagar Medical College & Hospitals, Puducherry, India. E-mail: dgonnaven@gmail.com
Introduction: The spinal canal is narrower in the upper lumbar levels than in the lower lumbar levels. Due to these reasons, the selection of a surgical approach is challenging. Fenestration discectomy at this level is more prone to neurological injury in most cases. Wide laminectomy or transforaminal approach is commonly used in upper lumbar disc surgeries. Surgical procedures using wide laminectomy and facetectomy give wide decompression but cause instability and need surgical fusion in most cases. We discuss an alternative approach for high lumbar disc disease using spinous process osteotomy, where minimally invasive non-fusion spine surgery is done with the preservation of posterior spinal elements.
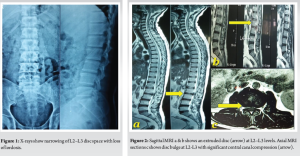
Case Report: A 38-year-old male presented with low backache and weakness of bilateral lower limbs for 2 weeks after lifting a heavy object. He also complained of bowel and bladder incontinence. Radiographs show L2–L3 disc space narrowing with no sign of instability in dynamic views. MRI showed an L2–L3 disc bulge with an extruded disc fragment compressing the central canal. Since the patient was young, to avoid fusion and adjacent segment disease, we planned for L2–L3 discectomy using a minimally invasive spinous process osteotomy approach. During the post-operative period, there was significant improvement in motor power and bowel and bladder control. The patient was mobilized from day 01 with support. With 1 year of follow-up, the patient is pain-free and has returned to his routine activities. Follow-up X-ray of the patient shows no sign of instability.
Conclusion: Spinous process osteotomy also minimizes tissue injury by preserving the paraspinal musculature and the interspinous, supraspinous ligament complex, and facets. Spinous process osteotomy is a modality of treatment for high lumbar disc disease in young patients without the need for spinal fusion.
Keywords: Spinous process osteotomy, high lumbar disc, bilateral decompression via unilateral approach.
Incidence of upper lumbar disc herniation L1–L2 and L2–L3 has been reported to occur in <1–2% of the population [1]. The spinal canal is narrower in the upper lumbar levels than in the lower lumbar levels, which may compromise the spinal nerve roots and conus medullaris. Due to these reasons, the selection of a surgical approach is challenging [2]. Fenestration discectomy at this level is more prone to neurological injury due to a narrow laminar window. Wide laminectomy or transforaminal approach is a commonly used approach in upper lumbar disc surgeries. Surgical procedures using wide laminectomy and facetectomy give wide decompression but cause instability and need surgical fusion [3] in most cases. These surgeries also lead to adjacent-segment degeneration. Compared with lower lumbar disc herniations, upper lumbar disc herniations have less favorable outcomes after surgery. Here, we discuss an alternative approach for high lumbar disc disease using spinous process osteotomy, where minimally invasive non-fusion spine surgery is done with the preservation of posterior spinal elements.
Pre-operative data was collected based on the history and the clinical presentation of the patient. A 38-year-old male presented with low back ache and weakness of bilateral lower limb for two weeks after lifting a heavy object. He also complained of bowel and bladder incontinence. Pre-operative motor and sensory assessment done. Detailed consent was obtained from the patient for the study. Radiographs show L2-L3 disc space narrowing [Fig. 1], with no sign of instability in dynamic views. MRI showed an L2-L3 disc bulge with an extruded disc fragment compressing the central canal [Figure 2]. Since the patient was young, to avoid fusion and adjacent segment disease, we planned for L2-L3 discectomy using a minimally invasive spinous process osteotomy approach, which is a well-established procedure described for minimally invasive spine surgeries.
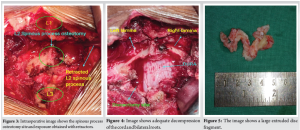
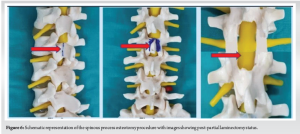
Surgical procedure: The patient was positioned in a prone position under general anesthesia, a posterior midline incision was made, and left-side paraspinal muscles were erased. L2-L3 level reached. Interspinous and supraspinous ligaments were slightly released from the above and below spinous process. L2 spinous process osteotomy is done using a curved osteotome, keeping a bridge of 10mm of the base of the spinous process intact. With discectomy distractors, the spinous process was retracted, and a broad exposure was obtained [Fig. 3]. Fenestration of lamina was done on either side, keeping the bilateral facet joint and pars interarticularis intact [Fig. 4]. Flavectomy and partial medial facetectomy were done. Intraoperatively, an extruded disc fragment was seen compressing the spinal cord [Fig. 5], and discectomy was done with minimal handling of the spinal cord. Once the distractors are removed; the spinous process falls back into position. Sutures were applied over the supraspinous and interspinous ligaments, and meticulous paraspinal muscle closure was done to keep the osteotomized spinous process in position. Fig. 6 shows the schematic representation of the procedure.
The post-operative period was uneventful. During the post-operative period, there was significant improvement in motor power and bowel and bladder control. The patient was mobilized from day 01 with support. With one year follow-up, the patient is pain-free and has returned to his routine activities. Fig. 7 shows the follow-up x-ray of the patient without any sign of instability.

Upper lumbar discs, due to the narrower spinal canal and anatomy of the conus medullaris, pose a significant challenge for surgical intervention. Limited laminotomy is inadequate to explore the herniated disc and needs extensive laminectomy to prevent violent handling of the dura. The conventional laminectomy technique involves exposure of lumbar posterior elements, which include stripping of the multifidus muscle bilaterally, with subsequent wide resection of the lamina, leading to various complications. Conventional laminectomy results in iatrogenic instability, which in turn needs posterior stabilization and fusion of mobile segments of the spine in most cases. Masashi et al. [4], in their study, mentioned that the technique of wide lumbar decompression that includes bilateral elevation of paraspinal musculature and aggressive bony resection could result in significant iatrogenic instability of the spine. Lin et al. [5] recommended lumbar fusion surgery for massive upper lumbar central discs or, if intraoperatively, more than 50% of lamina or facetectomy is done. Park et al. found that the incidence of adjacent segment disease after fusion ranged from 5.2–8.5% [6] in the lumbar spine. Sanderson et al. [7] stated that surgical outcomes were poor for L1–L2 and L2–L3 compared to L3–L4 discs in terms of post-operative back and radicular pain. Spinous process osteotomy is a less invasive technique that preserves the posterior midline elements while allowing them to be retracted away from the working area. It also offers better visualization [8]. Spinous process osteotomy provides a field similar to conventional midline laminectomy procedures. Bradley et al. [8] study found that spinous process osteotomy in lumbar decompressive surgery provides excellent visualization. Hermansen et al. stated that the dural sac area to be recreated had almost the average values through the spinous osteotomy process [9]. Spinous process osteotomy helps adequate cord decompression and bilateral foramina using unilateral exposure (bilateral decompression through unilateral approach), keeping the other side’s posterior elements and musculature untouched [10]. Since the lamina is not entirely removed and the posterior ligament complex (supraspinal and interspinal ligaments) are left intact, this procedure preserves the spine’s stability. Using the spinous process osteotomy, one retains the advantages of both laminectomy and fenestration procedures. Hermansen et al., in their study, assessed spinous process healing postoperatively. They discovered radiological union for 60 out of 135 (44%) spinous process osteotomies. It appears that the “complete union” of the osteotomy gives better clinical results. However, no statistical difference was noted in their study. They recommend that 10 mm of the base of the spinous process is left intact for a reunion. Delank et al. [11] concluded in their cadaver study on spinal canal decompression that bilateral hemilaminectomy, keeping the supraspinous and interspinous ligaments intact, did not result in increased motion. Hence, even when a spinous process is not united, the total stability of the spine should not be altered.
Conventional lumbar decompression results in extensive back musculature injury, leading to iatrogenic instability. Spinous process osteotomy minimizes the injury to the tissues by preserving the paraspinal musculature and the interspinous and supraspinous ligament complex and facets. Spinous process osteotomy offers advantages such as minimal muscle trauma, less post-operative discomfort, maintenance of spinal stability, early mobilization, and shortening of post-operative hospital stay with satisfactory decompression of the spine. Spinous process osteotomy can be considered a modality of treatment for high lumbar disc disease in young patients without the need for spinal fusion.
The spinal canal is narrower in the upper lumbar levels than in the lower lumbar levels. Surgical procedures using wide laminectomy and facetectomy give wide decompression but cause instability and need surgical fusion in most cases. Microdiscectomy procedures have the risk of neurologic injury due to the narrower canal. Spinous process osteotomy offers advantages such as minimal muscle trauma, less post-operative discomfort, maintenance of spinal stability, early mobilization, and shortening of post-operative hospital stay with satisfactory decompression of the spine.
References
- 1.Albert TJ, Balderston RA, Heller JG, Herkowitz HN, Garfin SR, Tomany K, et al. Upper lumbar disc herniations. J Spinal Disord 1993;6:351-9. [Google Scholar | PubMed]
- 2.Saberi H, Isfahani AV. Higher preoperative Oswestry disability Index is associated with better surgical outcome in upper lumbar disc herniations. Eur Spine J 2008;17:117-21. [Google Scholar | PubMed]
- 3.Weinstein JN, Tosteson TD, Lurie JD, Tosteson A, Blood E, Herkowitz H, et al. Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the spine patient outcomes research trial. Spine (Phila Pa 1976) 2010;35:1329-38. [Google Scholar | PubMed]
- 4.Takaso M, Nakazawa T, Imura T, Okada T, Fukushima K, Ueno M, et al. Less invasive and less technically demanding decompressive procedure for lumbar spinal stenosis--appropriate for general orthopaedic surgeons? Int Orthop 2011;35:67-73. [Google Scholar | PubMed]
- 5.Lin TY, Wang YC, Chang CW, Wong CB, Cheng YH, Fu TS. Surgical outcomes for upper lumbar disc herniation: Decompression alone versus fusion surgery. J Clin Med 2019;8:1435. [Google Scholar | PubMed]
- 6.Yee TJ, Terman SW, La Marca F, Park P. Comparison of adjacent segment disease after minimally invasive or open transforaminal lumbar interbody fusion. J Clin Neurosci 2014;21:1796-801. [Google Scholar | PubMed]
- 7.Sanderson SP, Houten J, Errico T, Forshaw D, Bauman J, Cooper PR. The unique characteristics of “upper” lumbar disc herniations. Neurosurgery 2004;55:385-9. [Google Scholar | PubMed]
- 8.Weiner BK, Fraser RD, Peterson M. Spinous process osteotomies to facilitate lumbar decompressive surgery. Spine (Phila Pa 1976) 1999;24:62-6. [Google Scholar | PubMed]
- 9.Hermansen E, Moen G, Fenstad AM, Birketvedt R, Indrekvam K. Spinous process osteotomy to facilitate the access to the spinal canal when decompressing the spinal canal in patients with lumbar spinal stenosis. Asian Spine J 2014;8:138-44. [Google Scholar | PubMed]
- 10.Dalgic A, Uckun O, Ergungor MF, Okay O, Daglioglu E, Hatipoglu G, et al. Comparison of unilateral hemilaminotomy and bilateral hemilaminotomy according to dural sac area in lumbar spinal stenosis. Minim Invasive Neurosurg 2010;53:60-4. [Google Scholar | PubMed]
- 11.Delank KS, Gercek E, Kuhn S, Hartmann F, Hely H, Röllinghoff M, et al. How does spinal canal decompression and dorsal stabilization affect segmental mobility? A biomechanical study. Arch Orthop Trauma Surg 2010;130:285-92. [Google Scholar | PubMed]









