Careful assessment of alignments on radiographs and intraoperative arthrogram findings can avoid unnecessary open reduction and its related complications in pediatric distal humerus fractures.
Dr Kalyan Deepak Sreenivas, Department of Orthopedics, All India Institute of Medical Sciences- Mangalagiri, Guntur district, Andhra Pradesh, India. E-mail id: drkalyan34@gmail.com
Introduction: The most common injuries around the elbow are the supracondylar humerus, followed by lateral condyle fractures. Transphyseal separations are uncommon, especially in children older than 3 years. Type 3 Weiss lateral condyle fractures appear similar to transphyseal separations on standard radiographs but have articular incongruity and may need open reduction. In comparison, transphyseal separations often need only closed reduction.
Case Report: We present a case of injury of the distal humerus in a 4-year-old child sustained due to a fall on the outstretched hand. Diagnoses, Treatment and Outcome: Transphyseal Separation and Lateral condyle humerus fractures were the differential diagnoses. The patient was treated with closed reduction and lateral pinning. The child had complete pain-free movements at the elbow at 3 and 12 months follow-up. With the help of the case report, we describe the importance of intraoperative post-reduction arthrograms to differentiate type 1, type 2 Weiss lateral condyle, and transphyseal separations from type 3 Weiss lateral condyle fractures.
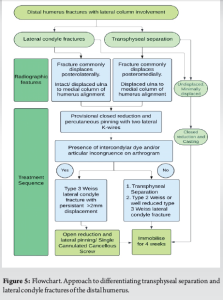
Conclusion: Transphyseal separation of the distal humerus can mimic lateral condyle fracture in children. Proper pre-operative radiographs and intraoperative arthrogram can avoid unnecessary open reduction and complications. This article presents a flowchart to help make a better decision regarding management.
Keywords: Transphyseal separation of humerus, elbow fracture, pediatric elbow injury, lateral condyle humerus, arthrogram.
Fractures around the distal humerus are common in pediatric age [1]. They are most commonly supracondylar fractures, followed by lateral condyle fractures and medial epicondyle fractures. Transphyseal separations of the humerus are rare and occur in children younger than 3 years, such as birth injuries in neonates or non-accidental injuries [2]. Lateral condyle fractures are classified based on their displacement. Weiss type 1, type 2, and type 3 are lateral condyle fractures with displacements of <2 mm, 2–4 mm, and more than 4 mm, respectively. Types 1 and 2 are treated by cast application or closed reduction with pinning. Type 3 fractures have articular incongruence and may need open reduction [3]. Transphyseal separations need closed reduction and pinning. It is challenging to differentiate transphyseal humerus from type 3 Weiss lateral condyle humerus fractures on plain radiographs [2]. Magnetic resonance imaging (MRI) is costly and needs sedation. Only limited literature is available to help the Orthopedician distinguish these fractures with overlapping clinical and radiological features, but different managements. In this case report, we describe the clinical and radiological features and provide a flowchart to help with decision-making.
A 4-year-old child was brought to the emergency department following an elbow injury due to a fall on the outstretched hand. Clinical examination showed swelling and deformity. There was no distal neurovascular deficit.
Diagnostic assessment
We preoperatively performed standard anteroposterior (AP) and lateral views of the elbow (Fig. 1). We performed a radiograph of the uninjured elbow for comparison. The differential diagnoses were transphyseal separation, lateral condyle humerus fracture, and elbow dislocation.

Therapeutic intervention
Under general anesthesia and in a supine position, closed reduction was done with longitudinal traction, mediolateral correction, and elbow flexion to stabilize the fracture. We did percutaneous pinning with two lateral 1.5 mm K-wires. We did arthrography by injecting Iohexol from the lateral aspect of the elbow. The arthrogram showed articular congruity (Fig. 2). Pins were bent, cut, left outside for easy removal, and immobilized at seventy degrees with a back slab. We did a post-operative CT to assess the fracture pattern and reduction. (Fig. 3).

Follow-up and outcome
The post-operative period was uneventful. We removed K wires at four weeks and started elbow mobilization. At the end of 3 months, a full range of movements was present, and the fracture showed good callus bridging over the medial and lateral metaphysis on the radiograph (Fig. 4).

Clinical presentation
Transphyseal separations are rare and often occur under 3 years of age [2]. They occur in newborns due to traumatic deliveries and child abuse. More common elbow injuries in children include supracondylar humerus fractures, lateral condyle fractures, and medial epicondyle fractures. Neurovascular injuries are uncommon after transphyseal separation and lateral condyle fractures when compared to supracondylar humerus fractures.
Investigations
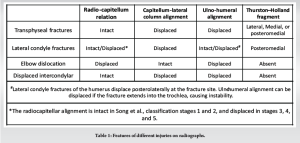
Radiographs include standard AP and lateral views. Transphyseal fractures are classified by DeLee into three groups based on ossification of the capitellum. Group A fractures (Salter-Harris Type-I) occur before the lateral condylar ossification center appears, usually in infants. Group B in ages 12 months to 3 years has a definite ossification center. They can be Salter–Harris II fractures with a small flake of metaphyseal bone. Group C includes large metaphyseal fragments (Salter–Harris II fractures), mostly seen in children aged 3–7 years. The classification was later modified by Zhou in 2019 to emphasize more on the size of the metaphyseal fragment rather than the age of the child [4]. In Weiss type 1 lateral condyle or medial epicondyle fractures, it is important to take internal and external oblique views [5,6]. We can detect Weiss type 2 and 3 injuries in standard AP and lateral views due to the higher displacement. The table shows the relation of various landmarks in different conditions (Table 1). Elbow dislocation also appears similar on radiographs but is uncommon in children. Intercondylar fractures can occur in older children and adolescents. They are often undisplaced, requiring only closed reduction and pinning, unlike in adults, where they are often displaced and rotated, requiring open reduction [1].
In inconclusive cases or suspected capitellum or intercondylar fractures, we can perform a CT or MRI or ultrasonography preoperatively or arthrogram intraoperatively. In transphyseal separations, CT can help identify the Thurston–Holland fragment. In our case, the CT showed a large medial Thurston-Holland fragment, a feature suggestive of entire distal humeral physeal injury, differentiating it from lateral condyle fracture. MRI is useful in differentiating these injuries accurately, but it needs sedation. Ultrasound is helpful in transphyseal separation of infants where the ossification of the lateral epiphysis has not started [1]. Treatment: Arthrography helps differentiate transphyseal separation and Type 3 Weiss lateral condyle fracture. It is a common conception to general orthopedic surgeons that lateral condyle requires open reduction. However, some lateral condyle humerus may be amenable for closed reduction. Hence, arthrogram is necessary during the surgery [6,7]. The continuous articular margin on the arthrogram suggests transphyseal separations, type 1, 2, or well-reduced type 3 Weiss lateral condyle fractures [8]. Type 3 Weiss fractures with displacement of more than 2 mm, even after closed reduction, need open reduction and pinning or cannulated cancellous screws [9]. A transverse column pin adds stability to the two lateral pins for lateral condyle fractures. Transphyseal separations can be treated similarly to supracondylar fractures with two to three lateral or cross wires [2]. Postoperatively, periosteal new bone formation is also an indicator of the type of fracture. The lateral condyle has a callus predominantly on the lateral column, and transphyseal separations have a callus on both medial and lateral columns. The flowchart (Fig. 5) can help in management.
Outcomes
If not reduced adequately, significant cubitus varus deformity can occur at later ages, needing corrective osteotomies. In contrast, lateral condyle fractures can have a wide range of complications, including osteonecrosis, nonunion, tardy ulnar nerve palsy, and cubitus valgus, which make long-term follow-up necessary [7,9,10].
Limitations of the case report include the need for proper pre-operative radiographs without backslab, including true AP, lateral, internal, and external oblique views. Furthermore, a pre-operative MRI is helpful in a more accurate diagnosis.
A careful assessment of alignments on radiographs and intraoperative arthrogram findings can help distinguish type 3 Weiss lateral condyle fracture from transphyseal separations. It can avoid unnecessary open reduction and its related complications.
Though distal humerus fractures are common injuries in children, it is important to know some rare injuries like transphyseal separation of the humerus. Following the flowchart provided in the report can help in streamlined management.
References
- 1.Anari JB, Arkader A, Spiegel DA, Baldwin KD. Approaching unusual pediatric distal humerus fracture patterns. J Am Acad Orthop Surg 2019;27:301-11. [Google Scholar | PubMed]
- 2.Abzug JM, Ho CA, Ritzman TF, Brighton BK. Transphyseal fracture of the distal humerus. J Am Acad Orthop Surg 2016;24:e39-44. [Google Scholar | PubMed]
- 3.Weiss JM, Graves S, Yang S, Mendelsohn E, Kay RM, Skaggs DL. A new classification system predictive of complications in surgically treated pediatric humeral lateral condyle fractures. J Pediatr Orthop 2009;29:602-5. [Google Scholar | PubMed]
- 4.Zhou W, Canavese F, Zhang L, Li L. Functional outcome of the elbow in toddlers with transphyseal fracture of the distal humerus treated surgically. J Child Orthop 2019;13:47-56. [Google Scholar | PubMed]
- 5.Knutsen A, Avoian T, Borkowski SL, Ebramzadeh E, Zionts LE, Sangiorgio SN. Accuracy of radiographs in assessment of displacement in lateral humeral condyle fractures. J Child Orthop 2014;8:83-9. [Google Scholar | PubMed]
- 6.Tejwani N, Phillips D, Goldstein RY. Management of lateral humeral condylar fracture in children. J Am Acad Orthop Surg 2011;19:350-8. [Google Scholar | PubMed]
- 7.Martins T, Tiwari V, Marappa-Ganeshan R. Pediatric lateral humeral condyle fractures. In: StatPearls. StatPearls Publishing; 2025. Available from: http://www.ncbi.nlm.nih.gov/books/nbk560664 [Last accessed on 2025 Mar 20]. [Google Scholar | PubMed]
- 8.Marcheix PS, Vacquerie V, Longis B, Peyrou P, Fourcade L, Moulies D. Distal humerus lateral condyle fracture in children: When is the conservative treatment a valid option? Orthop Traumatol Surg Res 2011;97:304-7. [Google Scholar | PubMed]
- 9.Song KS, Kang CH, Min BW, Bae KC, Cho CH, Lee JH. Closed reduction and internal fixation of displaced unstable lateral condylar fractures of the humerus in children. J Bone Joint Surg Am 2008;90:2673-81. [Google Scholar | PubMed]
- 10.Koh KH, Seo SW, Kim KM, Shim JS. Clinical and radiographic results of lateral condylar fracture of distal humerus in children. J Pediatr Orthop 2010;30:425-9. [Google Scholar | PubMed]