Intraoperative identification of a large, diameter corona mortis artery is critical in perioperative safety to avoid life-threatening hemorrhage during pelvic surgeries, specifically in acetabular fractures.
Dr. Damarla Meghana, Department of Orthopeadic, Dr. D. Y. Patil Medical Hospital and Research Centre, Pimpri Chinchwad, Pune, Maharashtra, India. E-mail: meghanad9@gmail.com
Introduction: The corona mortis (CM) artery or (“crown of death”) is a vascular anastomosis between the obturator artery and either the external iliac or inferior epigastric artery. An anastomosis is defined as one or more vessels that merge with other vessels before dividing. The CM's clinical significance arises from its potential of bleeding you can have if injured while performing any pelvic or acetabular surgeries. It is estimated that 25–33% of people have a CM artery and anatomical diameter and location variability is common. Surgeons should have a high index of suspicion and awareness.
Case Report: We report the case of a 25-year-old woman who was involved in a motor vehicle accident where she sustained a displaced acetabular fracture involving the anterior column and superior pubic ramus. During the surgical approach for acetabular fracture fixation, we identified an artery that had characteristics of a CM artery. The artery in question measured approximately 16 mm in circumference, which would equal approximately 5 mm in diameter; this is large in comparison to the average diameter of 2–4 mm. Because of the increased possibility of bleeding, we were able to safely dissect, tag, and retract the artery. The surgery proceeded uneventfully and the patient had an uneventful consistent postoperative recovery.
Conclusion: This case highlights the need to recognize and deal with vascular structures, like a large-diameter CM artery in this case, during pelvic surgeries. The intra-operative identification and tagging were critical to avoiding hemorrhagic complications. Pre-operative vascular imaging and intra-operative awareness are an important way of avoiding surgical risk in the case of any anterior pelvis surgery.
Keywords: Corona mortis, acetabular fracture, vascular injury, pelvic trauma, anastomosis, case report.
The Corona Mortis (CM), Latin for “crown of death,” refers to a vascular anastomosis between the obturator artery (or vein) and either the external iliac or inferior epigastric artery. This anatomical variant, though often asymptomatic, holds significant clinical relevance due to its potential to cause uncontrollable hemorrhage during pelvic and acetabular surgeries or traumatic injuries involving the pubic region [1,2]. The incidence of CM has been reported in approximately 25–33% of individuals, although figures vary depending on the population studied and the method of detection—cadaveric dissection, angiography, or surgical observation [2,3]. The CM artery may originate from either side, be unilateral or bilateral, and vary significantly in diameter, course, and proximity to the pubic symphysis. This variability makes it a critical structure to identify and manage during surgical approaches to the anterior pelvis. In what comes next, we focus on the pertinent concerns associated with an enlarged CM artery found during the surgical intervention focus on the anterior column and acetabular fracture on young women. Its ligation posed no difficulty, even though it had an exceptionally high potential for bleeding. Herein, we present a rare case of a high-caliber CM artery discovered intraoperatively during the management of an anterior column acetabular fracture in a young woman. The artery, which measured approximately 5 mm in diameter, posed a high hemorrhagic risk and was successfully ligated without complication. We discuss its clinical implications, especially with respect to preoperative planning and intraoperative management.
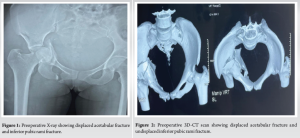
A 25-year-old female student presented to the emergency department following a high-velocity road traffic accident. She complained of unbearable right hip pain and inability to sit or stand. There was no history of comorbidities, prior surgeries, or anticoagulant use. On examination, the patient had swelling and marked tenderness over the right hip, with a limited and painful range of motion. Distal neurovascular examination was normal, and no signs of vascular compromise were observed. Pelvic radiographs and computed tomography (CT) scans revealed a displaced acetabular fracture involving the anterior column and superior pubic ramus (Fig. 1 and 2). Given the fracture pattern and patient’s functional demands, open reduction and internal fixation (ORIF) through an anterior intrapelvic (modified Stoppa) approach was planned.
Intraoperative findings
During surgical dissection, a prominent arterial structure was encountered traversing the superior pubic ramus in close proximity to the fracture site (Fig. 3). The artery’s location and morphology were consistent with the CM. Its size and turgidity suggested a significant blood flow, warranting precise assessment and cautious handling. To accurately estimate the vessel’s diameter, a sterile surgical tie was looped around the artery without compression. The tie was then measured against a standard surgical ruler, yielding a circumference of approximately 16 mm (Fig. 4). Using the formula: Diameter = Circumference/π = 16 mm/3.142 ≈ 5.09 mm, the vessel’s diameter was calculated to be approximately 5 mm—substantially larger than the average CM artery, typically described as 2–4 mm in prior literature. Due to its size and close proximity to the surgical field, the artery was carefully isolated, doubly clipped, and ligated. Hemostasis was secured, and the remainder of the procedure proceeded without incident. The patient recovered uneventfully and was discharged with standard postoperative rehabilitation.
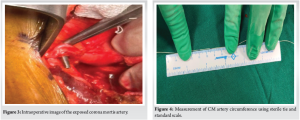
The measurement of the CM artery was conducted intraoperatively using a sterile surgical tie. After looping the tie around the artery, its length was measured using a standard graduated ruler (Fig. 4) while ensuring the vessel was not compressed or stretched. This unconventional yet practical method allowed immediate and real-time vascular assessment, which is especially valuable in emergency surgical settings lacking advanced imaging support. The vessel’s diameter was derived from its circumference using the mathematical relation: diameter = Circumference/π (16 mm/3.142≈5.09 mm). This technique, though simplistic, provided a reliable estimate in the context of operative decision-making. This measurement exceeds the commonly reported 2–4 mm diameter in most anatomical studies.
The CM is a critical yet often underappreciated anatomical variant in pelvic surgery. Its significance lies in the potential for massive hemorrhage if inadvertently transected. CM arteries larger than 3 mm in diameter pose a particularly high risk [2,4]. While most CM arteries range from 1–4 mm, our case involved a vessel approximately 5 mm in diameter—placing it among the upper extremes reported in the literature. Studies by Darmanis et al. found large-diameter CM arteries in up to 60% of cadaveric dissections [4], whereas Abbas et al. reported a 53.9% prevalence with associated surgical complications in 8% of cases [5]. Additional studies by Kashyap et al. and Rusu et al. highlighted the wide variability in prevalence (58.3% and 30%, respectively) and vessel size [6,7]. Interestingly, most anatomical studies do not describe a standardized measurement protocol for CM vessels, nor do they consistently compare their diameters to that of the conventional obturator artery. Early anatomical work by Engel (1859) and later surgical observations by Teague, Tornetta, and Okcu allude to the CM’s variability but lack precise, reproducible metrics [3]. In terms of management, preoperative identification of the CM artery is often limited by the cost and availability of vascular imaging, such as CT angiography. However, when feasible, preoperative vascular mapping is highly recommended. Intraoperative techniques for CM management include meticulous dissection, the use of vascular clips, and when necessary, embolization via interventional radiology [8-10].
This case underscores the importance of anticipating and managing vascular anomalies such as the CM during pelvic and acetabular surgeries. The presence of a large-diameter CM artery significantly increases the risk of hemorrhage, making intraoperative identification and control essential to avoid complications. Given its variable anatomy and potentially life-threatening consequences when injured, a high index of suspicion should be maintained, especially when operating near the superior pubic ramus. Surgeons must be familiar with both the anatomical variants and the appropriate management strategies to ensure patient safety.
Surgeons must be aware of the anatomical variability and potential size of the CM artery, particularly in acetabular fractures, where early recognition and ligation can significantly reduce intraoperative bleeding risks and improve patient outcomes.
References
- 1.Okcu G, Erkan S, Yercan HS, Ozalp T. The incidence and location of corona mortis: A study on 75 cadavers. Acta Orthop Belg 2004;70:163-7. [Google Scholar | PubMed]
- 2.Tornetta P 3rd, Hochwald N, Levine R. Corona mortis. Incidence and location. Clin Orthop Relat Res 1996;329:97-101. [Google Scholar | PubMed]
- 3.Teague DC, Graney DO, Routt ML Jr. Retropubic vascular hazards of the ilioinguinal exposure: A cadaveric and clinical study. J Orthop Trauma 1996;10:156-9. [Google Scholar | PubMed]
- 4.Darmanis S, Lewis A, Mansoor A, Bircher M. Corona mortis: An anatomical study with clinical implications in approaches to the pelvis and acetabulum. Clin Anat 2007;20:433-9. [Google Scholar | PubMed]
- 5.Abbas J, Tait WF, Shafik M, Timmons J, Doyle PJ. Surgical anatomy of the corona mortis. Ann R Coll Surg Engl 2009;91:313-6. [Google Scholar | PubMed]
- 6.Kashyap R, Garg N, Rajkumar A, Tuli SM. Corona mortis: Clinical significance during anterior approach to the pelvis-a cadaveric study. Med J Armed Forces India 2007;63:43-5. [Google Scholar | PubMed]
- 7.Rusu MC, Cergan R, Motoc AG, Folescu R, Pop E. Anatomical considerations on the corona mortis. Surg Radiol Anat 2010;32:17-24. [Google Scholar | PubMed]
- 8.Keating JF, Werier J, Blachut P, Broekhuyse H, Meek RN, O’Brien PJ. Early fixation of the vertically unstable pelvis: The role of iliosacral screw fixation of the posterior lesion. J Orthop Trauma 1999;13:107-13. [Google Scholar | PubMed]
- 9.Su A, Teh J, Whiteley G, Chesser TJ. Corona mortis: Its prevalence and anatomy using CT angiography. Clin Anat 2015;28:675-80. [Google Scholar | PubMed]
- 10.Sealy EB, Schammel CM, Varma R, Devane AM. Corona mortis in the setting of pelvic trauma: Case series and review of the literature. Am J Interv Radiol 2023;7:9. [Google Scholar | PubMed]