Primary hyperparathyroidism (PHPT) due to adenoma in adolescents, though rare, can present with multiple pathological fractures, osteitis fibrosa cystica, and brown tumors. Early recognition and intervention, including surgical excision, are critical for resolving systemic complications and preventing long-term morbidity.
Dr. Kishore Parihar, Department of Orthopaedics, Shri Ganesh Shankar Vidyarthi Memorial Medical College, Kanpur, Uttar Pradesh, India. E-mail: drkishoreparihar@gmail.com
Introduction: Primary hyperparathyroidism (PHPT) is a rare endocrine disorder in adolescents, characterized by excessive parathyroid hormone (PTH) secretion leading to hypercalcemia and various systemic manifestations.
Case Report: We present a case of a 19-year-old female with PHPT secondary to parathyroid adenoma, who initially presented with right distal thigh pain and pathological fracture. A diagnostic workup revealed hypercalcemia, elevated PTH levels, and multiple osteolytic lesions throughout her skeletal system. Radiological imaging confirmed extensive bone involvement, including lytic lesions in the femur, phalanges, and skull. Surgical exploration and parathyroidectomy were performed, with histopathology confirming adenoma. Postoperative management included calcium supplementation to manage transient hypocalcemia.
Conclusion: This case underscores the diagnostic challenges and aggressive skeletal manifestations of PHPT in young patients, emphasizing the importance of early recognition and intervention to prevent long-term complications.
Keywords: Primary hyperparathyroidism, parathyroid adenoma, pathological fracture, surgery, adolescent, hypercalcemia, multiple endocrine neoplasm.
Primary hyperparathyroidism (PHPT) is a condition characterized by excessive secretion of parathyroid hormone (PTH) from one or more parathyroid glands. This overproduction of PTH results in hypercalcemia and various systemic manifestations. PHPT is relatively rare in adolescents and young adults, where its presentation can be more severe compared to the older population. In this case, we discuss an adolescent female presenting with multiple bone lesions due to parathyroid adenoma, an uncommon but significant manifestation of PHPT.
Clinical presentation and diagnosis
The patient, a 19-year-old female, presented with right-sided distal thigh pain, swelling, and inability to walk following minor trauma. The clinical history revealed a 4-month period of insidious onset of right thigh pain, which was mild to moderate in intensity and relieved by analgesics. On physical examination, there was swelling of the left lower lobe of the thyroid, moving with deglutition, suggestive of an underlying thyroid or parathyroid pathology. There was no family history of multiple endocrine neoplasm (MEN). Laboratory investigations showed hypercalcemia (total serum calcium 10.60 mg/dL), hypophosphatemia (serum phosphorus 1.87 mg/dL), elevated alkaline phosphatase ([ALP] 1123 IU/L), and markedly elevated PTH levels (795 pg/mL). These findings are indicative of PHPT. The patient also had low vitamin D levels (9.44 ng/mL), which can exacerbate bone pathology in the context of hyperparathyroidism (Table 1).
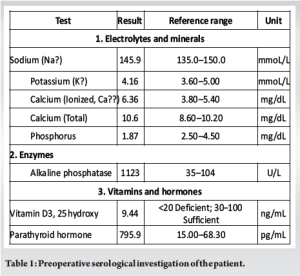
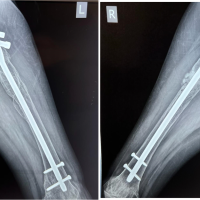
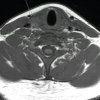
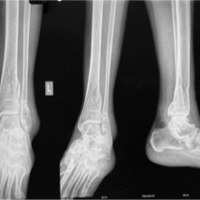
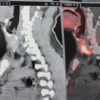
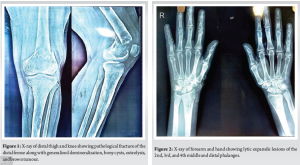
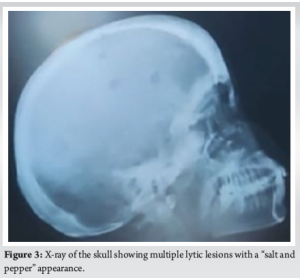
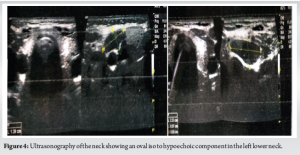
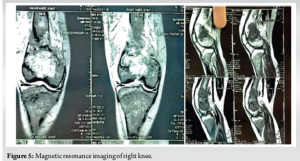
Radiological findings
Radiographs of the thigh revealed a right-sided pathological fracture of the distal femur along with generalized demineralization, bony cysts, osteolysis, and brown tumor (Fig. 1). X-rays of the forearm and hand showed lytic expansile lesions of the 2nd, 3rd, and 4th middle and distal phalanges (Fig. 2). X-ray of the skull revealed multiple lytic lesions with a “salt and pepper” appearance (Fig. 3). Ultrasonography (USG) of the right knee showed an ill-defined hypoechoic heterogeneous lesion on the medial aspect of the lower end of the femur with increased vascularity. USG of the neck revealed an oval iso to a hypoechoic component in the left lower neck, measuring 23.3 × 9.7 × 20.3 mm (Fig. 4). Magnetic resonance imaging of the right knee showed a large mass (7 × 2.9 × 5.8 cm) involving the distal end of the femur, including the diaphysis, metaphysis, and epiphysis, with a pathological fracture, soft tissue edema, and mild fluid collection in the distal thigh (Fig. 5). USG guided fine needle aspiration cytology of the lesion over the right distal femur was done which was suggestive of-giant cell-containing lesion. High-resolution computed tomography of the thorax revealed an expansile osteolytic lesion in the manubrium sterni, right head of the humerus, body of the right scapula, and multiple rib fractures. In addition, hypersensitivity pneumonitis, cardiomegaly, and mild hepato-splenomegaly were noted. USG of the abdomen showed mildly increased periportal echogenicity, a simple cyst (10 × 12 mm) at the midpole of the right kidney, increased bilateral renal echogenicity, and a few mesenteric lymph nodes (average size 10 × 5 mm) with maintained pancreatic hilar architecture. Although a sestamibi scan was highly recommended to confirm the diagnosis of PHPT, it was not performed due to the patient’s low economic status. The provisional diagnosis was a pathological fracture of the right distal femur with secondary osteoporosis at multiple levels caused by PHPT due to a suspected parathyroid adenoma.
Management
Initial management focused on stabilizing the patient’s condition, addressing the pathological fracture conservatively with a plaster of Paris cast, and correcting biochemical abnormalities with magnesium, calcium, and vitamin D supplementation, along with hydration and zoledronate infusion to stabilize serum calcium and ALP levels. This conservative approach was essential before definitive surgical intervention. The evaluation and management plan were formulated in collaboration with an endocrinologist, while the surgical intervention was carried out in coordination with an otorhinolaryngologist. Given the involvement of multiple organ systems, a multidisciplinary approach is crucial for the effective management of this condition.
Surgical intervention and histopathological findings
After preoperative evaluation, the patient underwent exploration of the swelling and parathyroidectomy of the left lower parathyroid gland, with the tissue sent for macroscopic and microscopic evaluation. Macroscopically, the thyroid nodule measured 3 × 2 × 1 cm, with a smooth, globular, and brown outer surface, and a cut surface showing colloid-filled areas. The parathyroid nodule measured 2.5 × 2 × 1 cm, with a brown cut surface. Microscopically, the thyroid nodule showed follicles of variable size composed of dilated and small follicles filled with colloid. The follicles were lined by cuboidal cells with round nuclei, bland chromatin, and a moderate amount of pale cytoplasm, with no evidence of malignancy suggestive of colloid nodule. The parathyroid nodule showed a well-circumscribed tumor composed primarily of chief cells forming follicles. These cells had small round nuclei and granular cytoplasm, with compressed normal parathyroid tissue seen at the periphery. Mild nuclear pleomorphism was observed, with no capsular invasion suggestive to parathyroid adenoma.
Post-operative care
The postoperative period was uneventful. Oral calcium supplementation was initiated, but the patient developed symptoms suggestive of hypocalcemia on the first postoperative day. To address this, an intravenous infusion of calcium gluconate was started to prevent bone hunger syndrome. This infusion was continued for two additional days until there were no signs or symptoms of hypocalcemia. At further follow up S. Calcium and S. PTH levels normalized. A liquid diet was introduced 6 h post-surgery, and the patient was discharged on the third postoperative day with prescriptions for oral calcium carbonate (CaCO3) and calcitriol. Postoperative calcium supplementation is crucial to avoid symptoms of both hypercalcemia and hypocalcemia. The patient’s bone pain and other symptoms resolved following the surgical intervention, and she has remained asymptomatic during subsequent follow-up. For the pathological fracture, the patient was initially placed in an above-knee cast for 6 weeks with non-weight bearing. After cast removal, clinical and radiological signs of union were observed. An above-knee cast was then applied allowing weight bearing with support for an additional 2 weeks. After a total of 8 weeks, the cast was removed, and the patient was permitted to walk with the assistance of a stick for 1 month. By the 3-month follow-up, the patient was allowed to walk independently without support.
Parathyroid adenoma in adolescent with pathological fracture is a relatively rare condition which we do not encounter in our daily outpatient department routinely. Rao stated PHPT is the third most common endocrine disorder after diabetes and thyroid disorders, the most common cause of hypercalcemia in the outpatient setting, and the second-most common cause of all causes of hypercalcemia after malignancy-related hypercalcemia [1]. PTH affects multiple organs, contributing to the clinical features of PHPT. In kidneys, it increases calcium reabsorption and phosphate loss, causing hypercalcemia and hypophosphatemia. In the gut, it enhances calcium absorption through vitamin D activation. Skeletal effects include bone resorption, leading to osteoporosis and fractures. Cardiovascular involvement includes hypertension and left ventricular hypertrophy, with increased mortality risk. PTH may also impact the nervous system, causing mood and cognitive symptoms. While its role in skin and soft tissue is unclear in non-tumor settings, its systemic actions underline the broad impact of PHPT [2]. According to Minisola et al. the incidence of PHPT shows notable variation across regions, genders, and age groups. The highest incidence is reported in the USA (48.3–50.4/100,000 person-years), whereas European countries like Spain and Denmark report lower rates. South African hospital-based data (78/100,000) suggest increased detection in clinical settings. Women consistently show a higher incidence than men. For example, in Spain, the incidence in women (40.3) is nearly triple that in men (13.7). Age also plays a critical role, with a dramatic increase among elderly women. In the USA, prevalence among women aged 70–79 reaches 1409 (Black women) and 1110 (White women) per 100,000–much higher than in men (85). These differences may reflect hormonal influences, aging, Vitamin D deficiency, and regional disparities in screening practices. The particularly high prevalence in Scandinavian countries (2000–5000/100,000) highlights the role of active case finding [2]. According to Marcocci and Cetani PHPT, which is most often caused by a single adenoma (80–85%) or four-gland hyperplasia (10–15%), mainly occurs as a sporadic disease, but it may be part of a hereditary syndrome (e.g., MEN types 1 and 2A) [3]. A retrospective analysis of 15 children and adolescents with PHPT (age <20 year) done by George et al. in the clinic between 1993 and 2006 they found out that the mean age of patients was 17.73 year (Range – 13–20, Male-3: Female-12). Average duration of symptoms was 18.87 (range: 0–48) months. Clinical features at presentation included bone pain (86.67%), proximal myopathy (46.67%), bony deformities (53.33%), fractures (60%), palpable osteitis fibrosa cystica (33.3%), renal calculi (40%), palpable neck swelling (13.3%) and acute pancreatitis (6.67%). None had a positive family history or features suggestive of MEN. After biochemical confirmation, the tumor was localized in all before surgery. Histopathology confirmed adenoma in all cases. Post-operative hungry bone syndrome occurred in 33.3% [4]. Like mentioned in the study we found out bony pain, browns tumor, palpable neck swelling, and pathological fracture in an adolescent female with no family history of (MEN), patient undergone parathyroidectomy and parathyroid adenoma confirmed by histopathology, post-operative hungry bone is not seen. Unlike the mentioned study there was no renal calculi. Multiple case reports also reported parathyroid adenoma with pathological fractures in adolescent and young patients such as Ebina et al. [5], Bhanu Murthy et al. [6], Sahu et al. [7], Kale and Vats [8], Deshmukh et al. [9], to support our study. As per Roizen and Levine [10] Genetic syndromes that are associated with multiple abnormal parathyroid glands may account for 5–15% of all cases of PHPT, and are relatively more common in patients younger than 40 years than in older patients making PTPH with pathological fractures in adolescent is relatively rare. As contrast to above mentioned studies, we have managed distal femur fracture conservatively by cast application. PHPT in adolescents is uncommon, and its presentation with multiple bone lesions due to a parathyroid adenoma is even rarer. The severity of bone involvement in this case, including osteitis fibrosa cystica and multiple brown tumors, underscores the aggressive nature of the disease in younger patients. The elevated PTH levels led to significant bone resorption, resulting in pathological fractures and cystic bone lesions. The case highlights the importance of considering PHPT in young patients presenting with unexplained bone pain, fractures, and systemic symptoms. Early diagnosis and management are crucial to prevent complications and improve outcomes. Surgical removal of the adenoma is the definitive treatment, leading to normalization of PTH and calcium levels and resolution of bone lesions over time.
This case of an adolescent female with PHPT due to a parathyroid adenoma and multiple bone lesions illustrates the need for awareness of this condition in young patients. Comprehensive evaluation and timely intervention are essential for effective management and to mitigate the long-term consequences of the disease.
PHPT in adolescents, though rare, can present with several pathological fractures, osteitis fibrosa cystica, and multiple brown tumors, as seen in our case. Early recognition and intervention, including surgical excision, are critical to resolving systemic complications and preventing long-term morbidity. Comprehensive evaluation is essential for diagnosing and managing such presentations effectively.
References
- 1.Rao SD. Epidemiology of parathyroid disorders. Best Pract Res Clin Endocrinol Metab 2018;32:773-80. [Google Scholar]
- 2.Minisola S, Arnold A, Belaya Z, Brandi ML, Clarke BL, Hannan FM, et al. Epidemiology, pathophysiology, and genetics of primary hyperparathyroidism. J Bone Miner Res 2020;37:2315-29. [Google Scholar]
- 3.Marcocci C, Cetani F. Clinical practice. Primary hyperparathyroidism. N Engl J Med 2011;365:2389-97. [Google Scholar]
- 4.George J, Acharya SV, Bandgar TR, Menon PS, Shah NS. Primary hyperparathyroidism in children and adolescents. Indian J Pediatr 2010;77:175-8. [Google Scholar]
- 5.Ebina K, Miyoshi Y, Izumi S, Hashimoto J, Naka N, Tsukamoto Y, et al. A case of adolescent giant parathyroid adenoma presenting multiple osteolytic fractures and postoperative hungry bone syndrome. Clin Case Rep 2015;3:835. [Google Scholar]
- 6.Bhanu Murthy R, Srihari V, Lakshmi Narayana M. Parathyroid adenoma in a young male with multiple fractures and varied clinical features. Indian J Otolaryngol Head Neck Surg 2014;66:114-7. [Google Scholar]
- 7.Sahu PK, Galagali JR, Singh ID, Kumar S. A large parathyroid adenoma presenting with pathological fractures in a young male. Int J Otorhinolaryngol Head Neck Surg 2015;1:88-92. [Google Scholar]
- 8.Kale PA, Vats H. Rare case presentation of parathyroid adenoma in a young female presenting as pathological fracture of long bones: A case study. Indian J Health Sci Biomed Res 2023;16:424-7. [Google Scholar]
- 9.Deshmukh RG, Alsagoff SA, Krishnan S, Dhillon KS, Khir AS. Primary hyperparathyroidism presenting with pathological fracture. J R Coll Surg Edinb 1998;43:424-7. [Google Scholar]
- 10.Roizen J, Levine MA. Primary hyperparathyroidism in children and adolescents. J Chin Med Assoc 2012;75:425-34. [Google Scholar]