Xanthogranulomatous osteomyelitis tends to resemble malignancy and should be taken into account as a differential diagnosis in scenarios where malignancy, chronic inflammation, and Tuberculosis is suspected and is unresponsive to treatment.
Dr. Pamidimukkala Sanjana, Department of Pathology, Sree Balaji Medical College and Hospital, Chromepet, Chennai - 600 044, Tamil Nadu, India. E-mail: shambu1297@gmail.com
Introduction: Xanthogranulomatous osteomyelitis (XO) is a rare form of chronic osteomyelitis. (XO) is invariably pathological. This lesion tends to extend into the adjacent soft tissues, mimicking malignancy. Non-specific symptoms associated are pain at the site of involvement, fever, leukocytosis, increased C-reactive-Reactive protein (CRP), and erythrocyte sedimentation rate (ESR). A Hallmark feature is the presence of lipid-laden macrophages or histiocytes, with acute and chronic inflammatory cells, in the histopathology. Infective organisms are identified rarely by culture, That is, usually sterile.
Case Report: We discuss here a case of (XO) of the right hip joint, a 30-year-old male patient presented with right hip pain throbbing type, which was insidious in onset. Accompanying symptoms included evening rise in temperature, loss of weight, and loss of appetite. The patient had a history of trauma for which he was treated with native splinting for 3 months. The laboratory investigations showed leucocytosis, elevated CRP, and ESR.
Conclusion: Histopathology examination is the gold standard in diagnosis as clinical and radiological findings are not so conclusive.
Keywords: Xanthogranulomatous, osteomyelitis, foamy histiocytes, chronic inflammation.
Xanthogranulomatous osteomyelitis (XO) is a rare form of chronic osteomyelitis.(XO) is invariably a pathological diagnosis as preoperative radiologic features are hardly helpful. Non-specific symptoms associated are pain at the site of involvement, fever, leucocytosis, increased C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR). A Hallmark feature is the presence of abundant lipid-laden macrophages or histiocytes, with acute and chronic inflammatory cells, in the histopathology[1]. Infective organisms are identified rarely by culture, that is, usually sterile. We discuss here a case (XO) of the right hip joint.
A 38- year- old male, presented with complaints of shortening of the right lower limb and limping for the past 20 years and pain in the right hip for 2 year. The patient had a history of trauma, 20 years back and was on native splinting for a period of 90 days. Following which, the patient complained of swelling and discharge from the right hip joint. He underwent wound exploration followed by drainage. Following which, the history is vague and non-contributory. He presented to the outpatient department of Sree Balaji Medical College and Hospital with pain in the right hip, which was insidious, throbbing type, associated with evening rise of temperature, along with a history of loss of weight and appetite for 2 mon. The patient had difficulty in performing daily activities. On physical examination, a swelling of 5 ×5 cm was identified along with local signs of infection / inflammation. X-ray imaging revealed sclerotic changes in the right acetabulum along with multiple lytic areas in the right ilium and right greater trochanter (Fig. 1).Computed tomography hip showed small cortical defects in right ilium with linear soft tissue calcified tract in the superior aspect of the right gluteal region (Fig. 2). Magnetic resonance imaging hip showed multiple pockets of fluid collections in the pelvis, along right iliacus and inguinoscrotal region, closely abutting the urinary bladder. Chest X-ray was normal. Laboratory investigations showed raised ESR-112 mm/hr, CRP-8.8mg/dL, total leucocyte count- 14,000/mm3, and differential count showed the predominance of neutrophils-81%, liver function tests showed elevation of gamma-glutamyl transferase and renal function tests were normal. Mantoux-negative, acid-fast bacillus-negative, pus culture and sensitivity showed no growth in culture. Gene X-pert Mycobacterium tuberculosis with rifampicin was not detected. An arthrotomy of the right hip was performed and the dissected material was sent to the histopathology lab for further evaluation. Grossly, the specimen received showed multiple gray-white to gray-brown soft tissue fragments altogether measuring-2×2 cm. Microscopically, sections showed spicules of necrotic bone, fibrocollagenous stroma, collections of foamy macrophages, and chronic inflammatory cell infiltrates composed of lymphocytes, plasma cells, and histiocytes (Figs. 3-5). Degenerated neutrophils, foreign body type of giant cells, and areas of necrosis are also seen. Thus, a HPE diagnosis of XO was signed out after carefully examining multiple sections in view of radiological changes not directly pointing toward a diagnosis of osteomyelitis. He was started on a course of antibiotics (linezolid), anti-inflammatory medications, calcium, and vitamin supplements for 1 month. The applied dressing was intact, sensations were present, and no distal neurovascular deficit was detected. He was advised an X-ray of the pelvis involving both hips anteroposterior view, after 1 week, after which patient contact was lost.
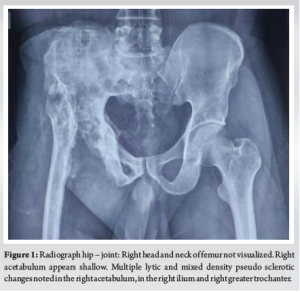
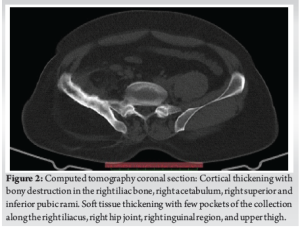
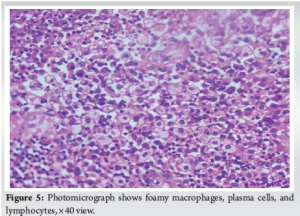
Xanthogranulomatous inflammation is a chronic inflammatory process, characterized by collections of foamy macrophages admixed with chronic inflammatory infiltrate. Delayed type hypersensitivity reaction of cell-mediated immunity has been implicated in the pathogenesis [2,3]. Xanthogranulomatous inflammation is seen involving organs such as gall bladder, kidney, colon, pancreas and salivary gland. Brain, lung, and bone are rarely affected (Borjan)[4]. very few cases of XO have been reported so far. When bone involvement ensues, the patient presents with both systemic and localized symptoms. It can present as a mass lesion extending into the surrounding tissue mimicking a tumor [5]. Our radiology revealed sclerotic and multiple lytic lesions noted in the right acetabulum, the right ilium, and the right greater trochanter. MRI in addition showed multiple pockets of fluid collection in the pelvis along the right iliacus and inguinoscrotal region closely abutting the urinary bladder, which is usually not associated in bone tumor. The earliest of these reports on XO were by Cozzutto and Carbone of the first rib and of the epiphysis of the tibia. In 1984, Cuzzoto identified and described it to be similar to Xanthogranulomatous lesions in the kidney and gallbladder characterized by foamy macrophages distributed in a mosaic pattern along with neutrophils, abundant plasma cells, and foam cells. Occasional foci of fibrin precipitates and multinucleated giant cells. The bacteriological assay carried out on the needle aspirate was negative in the first case [6]. In 2007, Vankalakunti et al. and colleagues reported ulnar XO in a post-menopausal woman. In this case, the patient had an increasing swelling on the extensor aspect of her right forearm for 2 years. The tissue culture was sterile, and XO was identified after a histopathologic examination [7]. There have been a few cases of XO mimicking a bone tumor, radiologically presenting as an osteolytic lesion along with the destruction of periosteum on X-ray. It may be associated with infection, obstruction, defective lipid transport, and immunological disturbances. The microscopic appearance of Xanthogranulomatous inflammation on histology shows characteristic clear and foamy cytoplasmic changes in the histiocytes along with plasma cell infiltration, multinucleated giant cells interspersed with lipid-laden macrophages, very rarely fibroblastic proliferation which imparts the characteristic yellow macroscopic appearance. This appearance, however, should be differentiated from a pseudoxanthomatous inflammation or malakoplakia characterized by Michaelis-Gutman bodies that stain positive with Von Kossa calcium and Prussian blue stains. Majority of XO cases, the patients undergo curettage of the involved bone along with bone grafting. To maintain the overall health of the patient antibiotics are started as a precautionary measure to maintain the surgical site wound. However, the exact role of antibiotics remains unclear, as XO is not always associated with active bacterial infection [8]. The histopathological differentials include lesions with foam cell collections – diagnosis for XO includes Langerhans cell histiocytosis, Erdheim-Chester disease, chronic recurrent multifocal osteomyelitis (chronic recurrent multifocal osteomyelitis) Xanthomas and some storage disorders with foam cell transformation, such as Gaucher’s and Nieman pick’s disease [9,10]. All these lack the inflammatory component seen in XO. In, Sinus histiocytosis with massive lymphadenopathy neutrophils are absent. It’s important to remember about the tumor with multiple lytic lesions metastatic clear cell adenocarcinoma from kidneys and other organs with clear cell components form challenges. IHC parameters are very useful in establishing the diagnosis.
(XO) is a very rare entity described in literature. Here, we discuss the case of a 38-year-old male who came with complaints of right hip pain- throbbing type, insidious in onset associated with evening rise of temperature, loss of weight, and appetite. He had a past history of trauma 20 years back, for which he underwent native splinting over a period of 3 months. Recently, when he presented in the pod he was diagnosed with septic arthritis / chronic osteomyelitis. He underwent arthrotomy and incision and drainage. He was covered with antibiotic coverage post-surgery to avoid post-operative infections and the sample was sent to the lab for histopathological examination. It was diagnosed as a case of Xantho granulomatous examination. It is the gold standard for definitive diagnosis when the clinical and radiological findings are inconclusive. The patient was prescribed antibiotics, and painkillers, along with vitamin and calcium supplements for a period of 1 month. He was advised to review after 1 week, but he did not return for follow- up.
XO should be suspected in the absence of clinical and radiological signs, and also refractory/ poor response to antibiotic treatment. Sometimes the presence of both inflammation and neoplasm, are observed. In such situations, the surgeon needs to tread carefully weighing all options.
References
- 1.Lee SH, Lee YH, Park H, Cho YJ, Song HT, Yang WI, et al. A case report of xanthogranulomatous osteomyelitis of the distal ulna mimicking a malignant neoplasm. Am J Case Rep 2013;14:304-7. [Google Scholar | PubMed]
- 2.Rathi M, Khattri J, Budania SK, Singh J, Awasthi S, Verma S. Xanthogranulomatous osteomyelitis. Arch Med Health Sci 2014;2:228-30. [Google Scholar | PubMed]
- 3.Cheema A, Arkader A, Pawel B. Xanthogranulomatous osteomyelitis of the humerus in a pediatric patient with alagille syndrome: A case report and literature review. Skeletal Radiol 2017;46:1447-52. [Google Scholar | PubMed]
- 4.Borjian A, Rezaei F, Eshaghi MA, Shemshaki H. Xanthogranulomatous osteomyelitis. J Orthop Traumatol 2012;13:217-20. [Google Scholar | PubMed]
- 5.Maeda T, Shimada M, Matsumata T, Adachi E, Taketomi A, Tashiro Y, et al. Xanthogranulomatous cholecystitis masquerading as gallbladder carcinoma. Am J Gastroenterol (Springer Nature) 1994;89:628-30. [Google Scholar | PubMed]
- 6.Cozzutto C, Carbone A. The xanthogranulomatous process. Xanthogranulomatous inflammation. Pathol Res Pract 1988;183:395-402. [Google Scholar | PubMed]
- 7.Vankalakunti M, Saikia UN, Mathew M, Kang M. Xanthogranulomatous osteomyelitis of ulna mimicking neoplasm. World J Surg Oncol 2007;5:46. [Google Scholar | PubMed]
- 8.Nakashiro H, Haraoka S, Fujiwara K, Harada S, Hisatsugu T, Watanabe T.Xanthogranulomatous cholecystis. Cell composition and a possible pathogenetic role of cell-mediated immunity. Pathol Res Pract 1995;191:1078-86. [Google Scholar | PubMed]
- 9.Kamat G, Gramapurohit V, Myageri A, Shettar C. Xanthogranulomatous osteomyelitis presenting as swelling in right tibia. Case Rep Pathol 2011;2011:257458. [Google Scholar | PubMed]
- 10.Kaneuchi Y, Tajino T, Hakozaki M, Yamada H, Tasaki K, Hasegawa O, et al. Xanthogranulomatous osteomyelitis of the distal tibia: A case report. Int J Rheum Dis 2017;20:2238-41. [Google Scholar | PubMed]