Two-stage surgery for ABC- first stage posterior stabilisation and biopsy followed, a week later, after HPEconfirmation, by second stage anterior corpectomy and reconstruction with cage is an effective method to treat ABC of thoracic vertebra.
Dr. Ashok Thomas, Department of Orthopaedic Surgery and Traumatology, SP Fort Hospital, Trivandrum, Kerala, India. E-mail: ashokthomas.spine@gmail.com
Introduction: Aneurysmal bone cysts (ABCs) are rare, representing about 1% of primary bone tumors and 15% of all primary spine tumors. When they are located in poorly accessible regions such as the spine and pelvis, their management can be challenging. Treatment options include selective arterial embolization, curettage, en bloc excision with reconstruction, and radiotherapy.
Case Report: A 68-year-old male presented to the outpatient department with complaints of left flank pain and abdominal pain for 4 months. Clinical examination showed tenderness in the thoracolumbar region with other spine examinations within normal limits. Magnetic resonance imaging dorsal spine showed an expansile lytic multiloculated lesion in the T11 vertebral body with mild extramedullary thoracic cord compression with subtle cord edema. The lesion showed a multiloculated bubbly appearance with fluid-layered locules. He underwent 2 stage procedure. In the first stage, posterior decompression, posterior stabilization, and biopsy were done. The histopathology report was consistent with ABCs. In the second stage, T11 corpectomy, tumor excision, and reconstruction with an expandable cage were done. Postoperatively his pain was reduced and was neurologically intact. At 4-year follow-up, clinically, he has excellent functional outcome and free of recurrence.
Conclusion: 360° excision and reconstruction is an effective treatment option for ABCs of spine in the elderly.
Keywords: Aneurysmal bone cyst, thoracic spine, surgical excision, and reconstruction, curettage.
Aneurysmal bone cysts (ABCs) are rare skeletal tumors that are benign, locally aggressive lesions and most commonly occur in the first two decades of life [1]. ABC comprising 1.4% of all primary bone tumors and 15% of all primary spine tumors. Among spine, thoracic (32%) and lumbar (34%) spine involvement is common [1,2]. Clinically, patients present with back pain, pathological fractures, instability, and neurologic deficits [2,3]. The ideal treatment for ABC in the thoracic spine is controversial. Treatment options include selective arterial embolization (SAE), direct intralesional injection of sclerosant, intralesional excision (curettage), en bloc excision and reconstruction, and/or radiotherapy. The clinical course of ABCs is sometimes unpredictable and local recurrences have been described with various types of treatments [4,5]. En-bloc resection appears to have the highest rate of cure. Spinal stabilization appears to provide the optimal method of acquiring a high degree of local control and preventing or correcting spinal deformity and instability [6-8]. We report a case of thoracic spine ABC, treated as a two-stage surgical procedure with 360° excision and reconstruction with an expandable cage.
A 68-year-old male presented to the outpatient department with complaints of left flank pain and abdominal pain for 4 months. The patient did not have any history of trauma, fever, or previous surgery related to this event. Clinical examination showed tenderness over the thoracolumbar region with other spine examinations within normal limits. He did not have any motor or sensory deficits.
Investigations
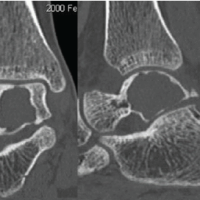
X-ray evaluation showed a pathological fracture of the T11 vertebra. Magnetic resonance imaging (MRI) dorsal spine showed expansile lytic multiloculated peripherally enhancing ill-defined lesion with a wide zone of transition replacing the entire normal marrow of the T11 vertebral body with grade II to thecal sac indentation, mild extramedullary thoracic cord compression with subtle cord edema. The lesion showed a multiloculated bubbly appearance with fluid-layered locules suggesting a possibility of ABC (Fig. 1). Differential diagnoses include Giant cell tumor, simple bone cyst, osteoblastoma, telangiectatic osteosarcoma, metastases, and plasmacytoma.
Diagnosis
His initial diagnosis was pathological fracture T11 with cord compression. In view of uncertain diagnosis, planned for a two-stage surgical procedure with decompression, stabilization, and biopsy in the first stage and resection and reconstruction in the second stage.
Treatment
The patient underwent two two-stage procedure.
First stage
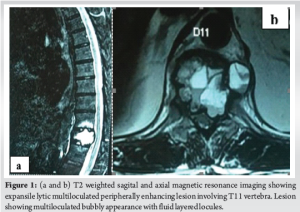
Posterior decompression, posterior stabilization, and biopsy were done. Bilateral pedicle screws inserted at T9, T10, T12 and L1. T11 posterior decompression was done by left hemilaminectomy and biopsy taken from T11 vertebra. The histopathology (HPE) report was consistent with ABC (Fig. 2).
Second stage
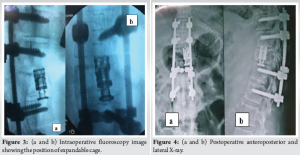
T11 corpectomy, tumor excision, and reconstruction with an expandable cage. Done 1 week after the first. Left lower thoracotomy. The 9th rib was exposed subperiosteally and excised. Pleura incised and the thoracic cavity entered. T11 was identified under c-arm guidance. ABC identified and removed in piecemeal. T11 corpectomy was done under the operating microscope. The defect is filled with local autograft and an expandable cage. Post-operative period, the patient was ambulated on day 1 with motor and sensory intact (Fig. 3, 4).
Follow up
At 4-year follow-up, clinically he has excellent functional outcome and is free of recurrence (Fig. 5 and 6).
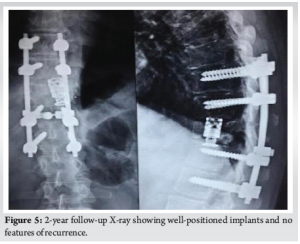
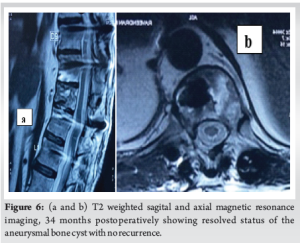
ABCs are a rare, benign locally aggressive type of lesion that usually appears in the early to mid-20s. They make up around 1% of primary bone tumors and 15% of primary spine tumors. Among the spine lumbar involvement is the most common, followed by the thoracic spine and cervical spine [1,2]. Here we report a case of thoracic spine ABC in an elderly patient. ABC arises from posterior elements of a vertebra and later involves the pedicles and vertebral body. Later on, there can be an intraspinal extension, which can cause neurological deficits [2]. Patients with an ABC often present with pain in the affected area along with neurological deficits. Paresthesia, paresis, and abnormal gait are common neurological manifestations when the spine is involved [1,2]. We e present a case of an elderly male patient with left-sided flank pain and abdominal pain and no other significant neurological symptoms. Computed tomography imaging typically shows an expansile, lytic lesion with a thin cortex and septae. MRI shows contrast enhancement with edema and fluid-fluid levels [9]. In this case, X-ray evaluation showed a pathological fracture of T 11 thoracic spine, and MRI showed expansile lytic multiloculated peripherally enhancing ill-defined lesion with a wide zone of transition replacing the entire normal marrow of the T11 vertebral body. The lesion showed a multiloculated bubbly appearance with fluid-layered locules. The differential diagnosis of lytic and expansive bone lesions includes solitary bone cyst, ABC, giant cell tumor, enchondroma, telangiectatic osteosarcoma, metastases, and plasmacytoma [2]. Treatment options for ABC are SAE, direct intralesional injection of sclerosants, intralesional excision (curettage), en-bloc excision and reconstruction, and/or radiotherapy [4,5]. We treated it with a 2-stage surgical procedure with posterior decompression, posterior stabilization, and biopsy in the first stage. HPE report was consistent with ABC. In the second stage T11 corpectomy, tumor excision and reconstruction with an expandable cage were done. Complete excision was achieved through the en bloc technique, However, this is a difficult procedure and has only been reported in rare cases[10]. The most common outcome of surgery is complete, piecemeal intralesional resection of ABC. The entire ABC must be removed, including all cyst walls and any abnormal tissues. In some cases, aggressive curettage may be used with high-speed drills to cut back into healthy bone. If the lesions are large and extensive, the most likely outcome is complete resection, which will likely result in iatrogenic instability and may necessitate instrumented fusion [2,8,9]. In this case, the postoperative period was uneventful. At 2 years follow up he demonstrated excellent functional outcome and showed no evidence of recurrence.
360° excision and reconstruction is an effective treatment option for ABC of spine in the elderly.
Two stage surgery for ABC- first stage posterior stabilisation and biopsy followed, a week later, after HPEconfirmation, by second stage anterior corpectomy and reconstruction with cage is an effective method to treat ABC of thoracic vertebra.
References
- 1.Cottalorda J, Kohler R, Sales de Gauzy J, Chotel F, Mazda K, Lefort G, et al. Epidemiology of aneurysmal bone cyst in children: A multicenter study and literature review. J Pediatr Orthop B 2004;13:389-94. [Google Scholar | PubMed]
- 2.Harrop JS, Schmidt MH, Boriani S, Shaffrey C. Aggressive “benign” primary spine neoplasms: Osteoblastoma, aneurysmal bone cyst, and giant cell tumor. Spine (Phila Pa 1976) 2009;4:S39-47. [Google Scholar | PubMed]
- 3.Boriani S, De Iure F, Campanacci L, Gasbarrini A, Bandiera S, Biagini F, et al. Aneurysmal bone cyst of the mobile spine: Report on 41 cases. Spine 2001;26:27-35. [Google Scholar | PubMed]
- 4.Papagelopoulos PJ, Currier BL, Shaughnessy WJ, Sim FH, Ebsersold MJ, Bond JR, et al. Aneurysmal bone cyst of the spine: Management and outcome. Spine (Phila Pa 1976) 1998;23:621-8. [Google Scholar | PubMed]
- 5.Simmons ED, Zheng Y. Vertebral tumors: Surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006;443:233-47. [Google Scholar | PubMed]
- 6.Refai D, Holekamp T, Stewart TJ, Leonard J. Circumferential vertebrectomy with reconstruction for holocervical aneurysmal bone cyst at c4 in a 15-year-old girl. Spine (Phila Pa 1976) 2007;32:E725-9. [Google Scholar | PubMed]
- 7.Yeung CM, Bilsky M, Boland PJ, Vaynrub M. The role of en bloc resection in the modern era for primary spine tumors. Spine (Phila Pa 1976) 2023;49:46-57. [Google Scholar | PubMed]
- 8.Glennie RA, Rampersaud YR, Boriani S, Reynolds JJ, Williams R, Gokaslan ZL, et al. A systematic review with consensus expert opinion of best reconstructive techniques after osseous en bloc spinal column tumor resection. Spine (Phila Pa 1976) 2016;41:S205-11. [Google Scholar | PubMed]
- 9.Mahnken AH, Nolte-Ernsting CC, Wildberger JE, Heussen N, Adam G, Wirtz DC, et al. Aneurysmal bone cyst: Value of MR imaging and conventional radiography. Eur Radiol 2003;13:1118-24. [Google Scholar | PubMed]
- 10.Thakar S, Hegde AS. Expansile thoracic vertebral lesion with fluid-fluid levels. Spine J 2016;16(9): e629 - e630. [Google Scholar | PubMed]