Surgical fixation with interfragmentary screws and the NISE knot approach provides dependable results for complex midshaft clavicle fractures. This approach ensures anatomical alignment, resulting in high union rates, early shoulder movement, and minimum complications, lowering the likelihood of non-union, malunion, and long-term functional impairment.
Dr. Arvind Vatkar, Consultant Orthopaedic Spine Surgeon, Fortis Hiranandani Hospital, Vashi, Navi Mumbai, Maharashtra, India. Assistant Professor, Department of Orthopaedics, MGM Medical College, Nerul, Navi Mumbai, Maharashtra, India. E-mail: vatkararvind@gmail.com
Introduction: Midshaft clavicle fractures are common, with comminuted variants posing a higher risk of non-union, often necessitating surgical intervention. Anatomical repair is critical due to the clavicle’s sole osseous connection between the shoulder and trunk, impacting functional outcomes.
Case Series: This retrospective study evaluated 83 patients (74 males, nine females, aged 18–65 years) surgically treated for midshaft clavicle fractures (2010–2023). Dominant-side fractures accounted for 87% of cases. Severe comminution was managed using 2.7 mm cortical interfragmentary screws and the NISE knot technique with plating. Follow-up spanned 18 months, assessing clinical and radiological outcomes. Patients regained near-complete shoulder motion within 3 weeks. Complications included visible deformity (n = 4), keloid formation (n = 3), scar hypoesthesia (n = 5), and one refracture with plate failure. No non-unions occurred, though two cases exhibited delayed union. Radiological and functional recovery was achieved in 97.6% of cases, with minimal long-term sequelae.
Conclusion: Surgical fixation of 3- or 4-part comminuted midshaft clavicle fractures using plate and screws demonstrates high union rates, rapid functional recovery, and low complication rates. This approach is recommended for complex fractures, as non-operative management risks non-union, malunion, and functional deficits.
Keywords: clavicle fractures, midshaft clavicle fractures, comminuted fractures, Surgical fixation, suture techniques (including NISE knot technique), interfragmentary screws, anatomical plates, functional outcomes, union rates, oxford shoulder score.
Clavicular fractures are common injuries, accounting for 2.6–4% of all fractures [1]. Midshaft fractures make up 80% of these, and their significant displacement and comminution can hinder healing and functional recovery [2]. Conservative management is often sufficient to manage these fractures [3]. However, This can lead to non-union and malunion, decreased shoulder function, long-term disability, pain, limited range of motion, and reduced strength, significantly affecting a patient’s quality of life [4]. Anatomical plating is a surgical procedure that enhances union rates and functional results by restoring the clavicle’s native structure and biomechanics [5]. It promotes early mobilization, increases shoulder range of motion, and decreases stiffness, improving functional recovery [6]. The use of interfragmentary screw fixation improves stability and facilitates bone repair [7]. The NISE (Non-Invasive Screw Fixation) approach may improve fixation strength while reducing soft tissue irritation [8]. Hence, we conducted a retrospective study to review the results of the anatomical plating and interfragmentary screw fixation and NISE knot technique at our institute.
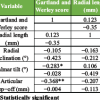
At our institute, retrospective interventional research on comminuted midshaft clavicular fractures was carried out. 951 admitted clavicle fractures treated between 2010 and 2023 were included in the hospital database from which the data were gathered. 83 patients with 3- or 4-part midshaft comminuted fractures who had surgery were included in the research. In their native language, each patient received information on the advantages and disadvantages of both surgical and non-operative care. The inclusion and exclusion criteria- The study included patients with comminuted midshaft clavicle fractures aged 18–65. Exclusion criteria included clavicle fractures not associated with segmental fractures, pathological fractures, chronic smokers and drug addicts, epilepsy patients, patients who refused surgery, refractures of previously operated clavicles, hemiplegic conditions, and those deemed medically unfit. Outcomes measured- The follow-up period was 18 months. The study assessed clinical and radiological outcomes of a shoulder joint injury. Clinical outcomes included range of motion, patient dependency, union rates, complications, such as visible deformity, keloid formation, hypoesthesia, and refracture, scores on the disabilities of the arm, shoulder, and hand (DASH) and Oxford Shoulder Score (OSS), and radiological outcomes, such as union rates, clavicular length restoration, malunion presence, and plate lift-off. Written informed consent had been obtained from the patient or guardian for participation and publication.
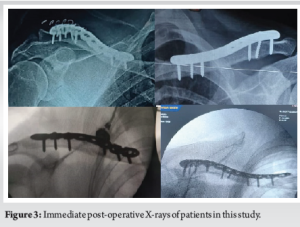
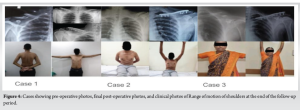
The surgical technique involved general anesthesia, aseptic precautions, and antibiotic coverage. A supra-clavicular incision was used to access the fracture site, preserving superficial nerves. Pointed reduction forceps were used to handle fracture fragments (Fig. 1a) and extra periosteal suture material was used for fragment reduction (Fig. 1b). In comminuted fractures, 2.7 mm cortical interfragmentary screws were used (Fig. 1c), with the NISE knot technique applied for severe comminution (Fig. 1d). The simplified method of the NISE knot is shown in Fig. 2, referenced from Hu et al. paper [9]. An anatomical clavicular plate was fixed with both non-locking and locking screws (Fig. 1e). Post-surgery, X-rays were taken (Fig. 3). Arm-to-body strapping was implemented for the early post-operative phase. Patients were discharged on the third post-operative day after one dressing change and given a body banian for protection. Suture removal was scheduled for the 11th day post-operation.

Statistical analysis
The study was done in SPSS version 21, with the descriptive analysis done for demographics and Oxford shoulder scores and a mixed design ANOVA test was done for Disability of arm, shoulder, and hand scores.
The research comprised 83 patients who had surgery for 3- or 4-part midshaft clavicle fractures; the average age of patient’s was 43.5 (±4.6 years)(range-: 18–65 years), showing a wide demography within that age group. The research included 74 male patients and nine female individuals. Notably, the dominant side was affected in 87% of fractures. The study found a near complete union rate with no malunions, surgical intervention, and no non-unions observed. The study showed effective restoration of clavicular length through superficial plating, interfragmentary screw fixation, and the NISE knot technique. NISE knot was applied in all cases, as in comminuted fractures, very often interfragmentary screws cant provide almost complete reduction with NISE Knot reinforces (Fig. 4).
Complications
Lateral lift-off was observed in two individuals due to varied clavicular curvatures. Two patients experienced delayed union, taking 4.5 months to show bony union.
Functional scores
The movements at the shoulder joint improved throughout 12 months, good SF-36 scores of 84–93 (SD ± 2.5) (Range 0–100) for surgical patients at the end of follow-up of 18 months.
- Patients experienced no dependency after 3–4 months of post-operative treatment, except for limb-bearing forces.
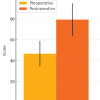
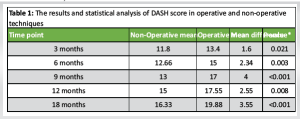
Disability of arm, shoulder, and hand (DASH) scores were taken from conservatively managed patients (92 patients) and operative patients (83 patients). A mixed-design ANOVA test was applied, with an independent t-test at each time period with Bonferroni correction (adjusted α = 0.01). There’s a statistically significant difference in how well people recover, depending on whether they had surgery for clavicle fracture or not, with the P-value being = 0.0029. The statistical significant difference between the surgery group and the non-surgery group changes over time (P = 0.0031) (Table 1).
The Oxford Shoulder Score (OSS ) were:
Scores: 22 (3 months) → 26 (6 months) → 30 (9 months) → 35 (12 months) → 40 (18 months), – Presumed scale: 0–48 (higher = better function).
OSS in operated patients’ data showed significant improvement over time. The study found that 86% of the variance in OSS scores can be explained by time, suggesting that time is a strong factor for shoulder scores. The shoulder function improved faster in the early months (3–9 months) compared to later months (9–18 months). By 6 months, OSS scores reached the “Minimal Clinically Important Difference” (MCID). By 18 months, 83% of the maximum OSS (40/48) had been recovered.
Our study involved 83 patients with midshaft clavicle fractures, with an average age of 43.5 years. The dominant side experienced 87% of fractures, and the study found a near complete union rate. The study showed effective restoration of clavicular length through superficial plating, interfragmentary screw fixation, or the NISE knot technique. Functional scores improved throughout 12 months, with good SF-36 scores at 18 months. The Oxford shoulder score (OSS) significantly improved over time, with 86% of the variance explained by time. Dhadak et al. showed that the operative group saw 19 patients with excellent functional outcomes, four with good outcomes, and two with fair outcomes. Two patients had hypertrophic skin scars, 8% experienced plate prominence, 8% had superficial infection, 4% experienced plate loosening, 8% experienced delayed union, and 4% experienced plate breakage [10]. Annichirico et al. in her retrospective study on 32 patients with midshaft clavicle fractures treated with plate and screws between 2009 and 2014 found that all patients healed clinically and radiographically without deformities or non-unions. They returned to pre-injury sports activities with a mean Constant Score of 93.8 and a mean DASH score of 42 at 1 year follow-up [11]. Lui et al. evaluated the effectiveness of an Endobutton plate combined with high-strength suture Nice knot fixation in treating distal clavicular fractures with coracoclavicular ligament injuries. It involved 43 patients. The operative group showed an average shorter bone healing time (12.82 weeks) and improved VAS scores (9.25), Constant-Murley scores, and ASES scores post-operatively compared to the control group [7]. Hu et al. examine the effectiveness and prognosis of Nice Knots-assisted reduction in treating displaced comminuted clavicle fractures. Thirty-eight patients were treated with open reduction and internal fixation and the NISE knot technique. The Nise Knots group significantly reduced operation time, fluoroscopy time, and intraoperative blood loss (P < 0.001) [9]. Our study is among the first in the Indian population to use the NISE knot approach for fixing midshaft clavicle fractures. However, our study has a few drawbacks. This was a retrospective research. The study had a smaller number of patients and no control group. As a result, we advocate a multicenter randomized control trial with a control group comparing traditional plating to the NISE knot approach and plating for clavicle midshaft fractures, with a long follow-up period.
Anatomical plating combined with interfragmentary screw fixation and the NISE knot approach results in good union rates and efficient restoration of clavicular length in comminuted midshaft clavicle fractures. This method can surgically address these fractures with good functional outcomes and high union rates. Future multicenter randomized controlled trials with a control group comparing traditional plating to the NISE knot approach and plating and longer follow-up periods are required to confirm these findings and provide more support for the NISE knot technique’s superiority.
Early surgical treatment is highly beneficial for comminuted midshaft clavicle fractures. Cortical screws and the NISE knot with plate fixation provide early mobility and strong healing. Surgeons should consider surgical repair in multi-part fractures to minimize problems associated with conservative therapy, such as non-union and impaired shoulder function.
References
- 1.Kihlström C, Möller M, Lönn K, Wolf O. Clavicle fractures: Epidemiology, classification and treatment of 2 422 fractures in the Swedish fracture register; An observational study. BMC Musculoskelet Disord 2017;18:82. [Google Scholar | PubMed]
- 2.Song HS, Kim H. Current concepts in the treatment of midshaft clavicle fractures in adults. Clin Shoulder Elb 2021;24:189-98. [Google Scholar | PubMed]
- 3.Lenza M, Faloppa F. Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database Syst Rev 2016;12:CD007121. [Google Scholar | PubMed]
- 4.Van Der Burg FA, Baltes TP, Kloen P. Large segmental defects in midshaft clavicle nonunion treated with autologous tricortical iliac crest bone graft. Shoulder Elbow 2023;15:45-53. [Google Scholar | PubMed]
- 5.Page BJ, Ricci WM. Failed fixation of clavicle fracture. In: Failed Fracture Fixation. Cham: Springer International Publishing; 2024. p. 65-75. Available from: https://link.springer.com/10.1007/978-3-031-39692-2_5 [Google Scholar | PubMed | CrossRef]
- 6.Pastor T, Zderic I, Berk T, Souleiman F, Vögelin E, Beeres FJ, et al. New generation of superior single plating vs. Low-profile dual minifragment plating in diaphyseal clavicle fractures: A biomechanical comparative study. J Shoulder Elbow Surg 2024;33:409-16. [Google Scholar | PubMed]
- 7.Liu B, Shi L, Ma H, Yu H, Jiang J. Analysis of the efficacy of endobutton plate combined with high-strength suture nice knot fixation in the treatment of distal clavicle fractures with coracoclavicular ligament injuries. BMC Musculoskelet Disord 2024;25:927. [Google Scholar | PubMed]
- 8.Naderipour A, McKee MD. Precontoured plate fixation with interfragmentary lag screw use in a middle third clavicle fracture fixation. J Orthop Trauma 2015; Jul 28. doi: 10.1097/BOT.0000000000000402. Online ahead of print. [Google Scholar | PubMed | CrossRef]
- 9.Hu F, Liu X, Liu F, Jia H, Lv X, Wang F, et al. Intraoperative nice knots assistance for reduction in displaced comminuted clavicle fractures. BMC Musculoskelet Disord 2021;22:467. [Google Scholar | PubMed]
- 10.Dhakad RK, Panwar M, Gupta S. Plating versus conservative treatment in mid shaft fractures of clavicle: A comparative study. J Clin Orthop Trauma 2016;7 Suppl 2:166-70. [Google Scholar | PubMed]
- 11.Annicchiarico N, Latta A, Santolini E. Plate osteosynthesis for mid-shaft clavicle fractures: An update. Injury 2023;54 Suppl 1:S53-7. [Google Scholar | PubMed]