Simultaneous bilateral total knee arthroplasty (SBTKA) is safe for elderly patients over 70 years, even with comorbid conditions, when performed in a well-equipped hospital. Delaying surgery can lead to worse functional outcomes, highlighting the importance of timely surgical intervention.
Dr. Yogesh Chaudhari, Department of Orthopaedic Surgery and Joint Replacement Surgery, Nine Pearls Hospital, Nashik, Maharashtra, India. E-mail: dryogeshchaudhari6@gmail.com
Aims and Objective: The present study aims to investigate the perioperative outcomes of elderly patients undergoing simultaneous bilateral total knee arthroplasty (SBTKA).
Materials and Methods: A retrospective single-center observational study was conducted on elderly patients (>70 years) undergoing SBTKA. Perioperative outcomes were assessed, including the incidence of complications such as cardiac and renal dysfunction, rate of transfusion, and total length of stay (LOS). Descriptive statistical measures were used to summarize study parameters.
Results: The average LOS for patients was 4.71 days. A total of 38 incidences of adverse events were recorded. The most common adverse event was acute kidney injury (17.16%). There was a moderate positive correlation between LOS and complications, as well as LOS and blood transfusion requirements. Patients requiring blood transfusions during their hospital stay had a longer LOS of 5.47 days compared to non-transfused patients (4.45 days). Patients with chronic kidney disease had the highest LOS (5.10 days), followed by those with Parkinson’s disease (5.00 days). The LOS was relatively consistent across different age groups.
Conclusion: SBTKA is a safe and satisfactory procedure for patients over 70 years old and those with comorbid conditions at a multispecialty hospital with intensive care support. However, delaying surgery when indicated may lead to worse functional outcomes, highlighting the importance of timely intervention.
Keywords: Arthroplasty, knee replacement, simultaneous bilateral total knee arthroplasty, elderly.
Osteoarthritis (OA) is one of the most common joint disorders, contributing to chronic pain and disability, particularly in developed nations [1]. Knee OA is caused by mechanical damage and deterioration of the articular cartilage. In 2020, an estimated 595 million individuals worldwide were affected by OA, accounting for approximately 7.6% of the total population [2]. In India, the prevalence rate of OA is higher than the global burden, with knee OA affecting 22–39% of the Indians [3]. Notably, knee OA is more prevalent in India than in Western countries and remains the leading cause of joint dysfunction. The first line of treatment includes conservative options using medications, physical activity, and patient education for symptom management. However, the failure of these treatments to improve disease conditions requires surgical interventions. Total knee arthroplasty (TKA) is the preferred surgical option for patients who do not respond to conservative treatments and for those presenting with OA affecting multiple compartments of the knee [4]. In approximately 20% of knee OA patients requiring TKA due to advanced conditions, a bilateral knee involvement is reported, necessitating bilateral TKA (BTKA) [5]. The BTKA procedure can be conducted either simultaneously, where both knees are replaced in the same surgery, or in a staged manner, where each knee undergoes a separate procedure with a minimum interval of 3 months between the two surgeries [6]. Simultaneous BTKA (SBTKA) offers several advantages over staged BTKA. It provides greater convenience and satisfaction for patients due to single hospitalization, reduced anesthetic exposure, decreased overall duration under anesthesia, and lower intake of pain medications [6]. In addition, the simultaneous procedure results in the reduction of the duration of hospital stay by 4–6 days, reduced health-care costs by approximately 18–36%, faster recovery, accelerated rehabilitation, and fewer sessions of physical therapy [6]. The procedure provides similar post-operative function, radiographic outcomes, and implant survival to those observed in patients undergoing unilateral TKA (UTKA) [7-9]. Despite the several benefits of performing an SBTKA, many surgeons do not advise patients to undergo this procedure due to evidence indicating higher complications compared to UTKA and staged BTKA [10]. Consequently, SBTKA is typically performed in a highly selective group of patients [11]. Surgeons perform SBTKA on younger individuals with minimal comorbidities. This cautious patient selection is supported by studies identifying age and comorbidity burden as key predictors of major complications and mortality [11-13]. The impact of these factors is more significant in patients with bilateral OA, as this condition exacerbates functional impairments and predisposes individuals to comorbid conditions, including cardiovascular and pulmonary diseases [11,12]. These elevated risks have contributed to the exclusion of older patients from undergoing SBTKA, even in cases of severe bilateral symptoms. With the increase in the aging population across the globe and in India, the demand for SBTKA is expected to rise. Given the ongoing debate on whether performing SBTKA is safe and effective in elderly patients, identifying whether the age of the patients can influence surgical outcomes or increase the risk of complications is important. To address this, the present study aims to investigate the perioperative outcomes of elderly patients undergoing SBTKA, focusing on the length of hospitalization, comorbidities, complications, and the need for transfusions.
Study design and participants
A retrospective single-center observational study was conducted. Medical records of patients who underwent SBTKA at our tertiary care hospital between July 1st, 2022, and June 30th, 2024, were screened. Patients fulfilling the selection criteria were included for analysis in the study. The inclusion criteria of the study were: (1) patients aged 70 years or older at the time of surgery, (2) patients who underwent SBTKA for bilateral end-stage primary knee OA, and (3) patients with a follow-up duration of at least 1 year. Patients undergoing a revision TKA or those having incomplete medical health records were excluded from the study.
Surgical procedures
All the study participants underwent SBTKA at a single institution utilizing identical surgical equipment under the supervision of the same senior joint replacement surgeon and a team of consultant anesthesiologists. SBTKA was performed using simultaneous inflation of both tourniquets with two sets of surgical tools and instruments. A medial subvastus capsular approach was uniformly adopted for all surgeries. Implant selection between bilateral cruciate-retaining (CR), posterior-stabilized (PS), or a combination of CR/PS was based on the surgeon’s pre-operative planning and intraoperative assessments. All the patients underwent implantation with coronal mechanical alignment technique using identical prostheses. Standard use of two drains, one placed intra-articularly and the other subcutaneously, was recommended. Both drains were removed within 48 h of SBTKA. A multimodal prophylactic strategy was used to prevent deep vein thrombosis, and all patients followed a standardized rehabilitation protocol. The hemoglobin threshold for transfusion was set at 8.0 g/dL for asymptomatic patients with intermediate cardiovascular risk, whereas a higher threshold of <9.0 g/dL was set for symptomatic patients and those at elevated risk of cardiovascular events.
Data collection
Data were retrospectively collected from existing health records of SBTKA patients. Patient demographic data such as age and comorbidities were collected. The presence of pre-operative comorbid conditions, including hypertension, diabetes mellitus, asthma, ischemic heart disease (IHD), chronic kidney disease (CKD), Parkinson’s disease (PD), and hypoparathyroidism was recorded. The perioperative assessment included the incidence of complications such as cardiac and renal dysfunction, rate of transfusion, and total length of stay (LOS).
Statistical analysis
Descriptive statistical measures were used to summarize demographic data, clinical characteristics, and perioperative outcomes. Categorical data were summarized using frequency and percentage, and continuous parameters were defined using mean and standard deviation (SD).
Patient demographic data
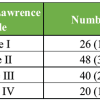
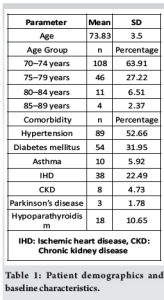
A total of 169 patients undergoing SBTKA were included in the study. The mean age of the study population was 73.83 years (SD = 3.50). Most patients (63.91%) were aged 70–74 years, followed by 27.22% in the 75–79 years category. A smaller proportion of patients were in the 80–84 years (6.51%) and 85–89 years (2.37%) age groups (Table 1). The study population had several comorbidities, with several patients presenting with multiple comorbidities (Table 1). The most prevalent comorbidity was hypertension, reported by 52.66% of the participants, followed by diabetes mellitus and IHD in 31.95% and 22.49% of the patients, respectively. Other less common conditions were hypoparathyroidism, asthma, CKD, and PD.
Perioperative outcomes
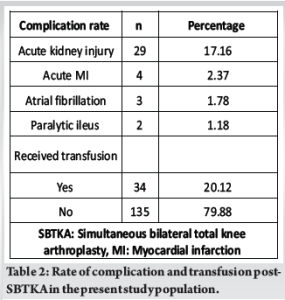
The average LOS for all patients was 4.71 days, with most patients hospitalized for 4–5 days. A total of 38 incidences of adverse events were recorded (Table 2). The most common adverse event was acute kidney injury (17.16%). Rare adverse events included acute myocardial infarction (AMI) (2.37%), atrial fibrillation (1.78%), and paralytic ileus (1.18%). A total of 34 patients (20.12%) required blood transfusions during their hospital stay.
Correlation between perioperative outcomes and LOS
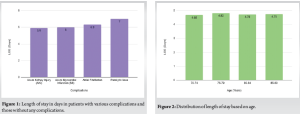
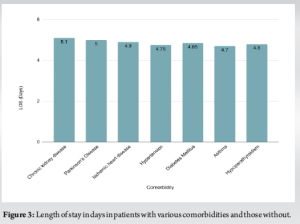
The LOS demonstrated heterogeneity with the presence of comorbidities and complications, age, and the need for transfusion. There was a moderate positive correlation between LOS and complications, and LOS and blood transfusion requirements. Patients with complications had significantly longer LOS (5.68 days) compared to those without (4.32 days). The LOS associated with different complications is outlined in Fig. 1. Patients requiring blood transfusions during their hospital stay had a longer LOS of 5.47 days compared to non-transfused patients (4.45 days). The LOS was relatively consistent across different age groups, with a slight increase in the 75–79 years age group (Fig. 2). Patients with CKD had the highest LOS (5.10 days), followed by those with PD (5.00 days) (Fig. 3).
The analysis of perioperative outcomes in elderly patients undergoing SBTKA demonstrated that the average LOS was influenced by several factors. A moderate positive correlation was identified between LOS and both the occurrence of complications and the need for transfusion. Patients experiencing complications or requiring transfusions had prolonged hospital stays compared to those without these factors. There was no significant association between age of the patients and hospitalization duration. Among comorbid conditions, CKD and PD were associated with extended hospitalization. The most frequently observed post-operative complication was acute kidney injury, whereas less common adverse events included AMI, atrial fibrillation, and paralytic ileus. A considerable proportion of patients required blood transfusions during hospitalization. Overall, the study identified acceptable rates of transfusion and a lack of association between age and LOS. This signifies that SBTKA offers similar outcomes regardless of the age of the patients. TKA is one of the most frequently performed orthopedic procedures globally, with an increasing number of patients electing to undergo this surgery [14]. However, Indian patient families and even health-care professionals show concerns regarding the safety of this elective procedure, particularly in older adults. Given that many of these elderly patients present with multiple comorbidities, their post-operative recovery may be influenced by both anesthetic and surgical factors [15]. TKA can be performed either simultaneously or separately for both knees. In advanced deformities in both knees, staged TKA may pose challenges in post-operative mobilization, as one knee has been treated, but the other remains the same. Delaying the second procedure for an extended period could contribute to early implant loosening in the previously operated knee [16]. Furthermore, staged procedures require patients and their caregivers to undergo two separate surgeries [17]. In addition, multiple studies have demonstrated that SBTKA is a more cost-effective alternative compared to the staged approach, offering both economic and surgical advantages [18]. The most frequently observed complication in the present study population was acute kidney injury. Acute kidney injury is a well-documented post-operative complication that may arise when a patient undergoes total hip or knee arthroplasty [19]. The high incidence of post-operative acute kidney injury may be attributed to the sudden increased consumption of pharmacological agents and medicines, which are required throughout the perioperative period. A study conducted by Nadkarni et al. identified a strong association between perioperative blood transfusion and the occurrence of acute kidney injury [20]. Their multivariate analysis demonstrated that patients who received a blood transfusion had a 128% higher risk of developing acute kidney injury. Therefore, patients receiving blood transfusions or high-dose medications with existing renal dysfunction may develop acute kidney injury post-surgery. The second most prevalent complications reported postoperatively were cardiac events, AMI, and atrial fibrillation. These complications were observed in a significantly small number of populations. Patients having pre-existing cardiac conditions were predisposed to such events post-SBTKA. While cardiac events are the main cause of mortality in patients undergoing joint replacement surgeries [21], no mortality was reported despite the incidence of cardiovascular complications. This indicates that the complications were timely and appropriately managed at the institution. Therefore, SBTKA is associated with certain risks of renal and cardiac impairments. However, cautious monitoring of at-risk patients can help improve post-operative outcomes. Despite an increased risk of perioperative medical complications, the efficacy of SBTKA in alleviating severe knee pain in elderly patients cannot be disregarded. Stroh et al. demonstrated that individuals above 80 years undergoing TKA benefited significantly from the procedure, with improvements in mobility and quality of life outweighing the associated risks [22]. In addition, a study reported that among patients older than 85 years, approximately 76% were able to maintain independent living postoperatively, and nearly one-third were capable of driving again [23]. Beyond its orthopedic benefits, TKA can reduce the risk of serious cardiovascular events in patients with moderate-to-severe OA. A study by Ravi et al. found that total joint replacement surgeries resulted in a 40% decrease in cardiovascular complications, an indirect cardioprotective effect of the surgery caused by enhanced physical activity and reduced pain, painkillers, and psychological stress [24]. Therefore, SBTKA must be considered in the elderly after a risk-benefit analysis as it offers improved quality of life and functionality. The present study reported a mean LOS of 4.71 days. Kirschbaum et al. found an average LOS of 7.8 days in elderly patients (mean age of 69 years) undergoing SBTKA [25]. Another retrospective observational study on SBTKA patients revealed an average length of hospitalization as 9 days [26]. Similarly, reports from a tertiary center noted an 8–11-day LOS in patients undergoing SBTKA [27]. Compared to previous investigations, the present study has a significantly shorter duration of stay. The relatively short average hospital stay observed in our study may be due to optimal pain management, the presence of well-equipped rehabilitation facilities, and the implementation of structured physiotherapy protocols at our institution. No significant correlation between the LOS and age was identified, indicating a similar duration of hospitalization across all age groups. In alignment with these findings, Gupta et al. found the LOS to be similar across the various age groups: <60, 60–69 years, and over 70 years [28]. Other studies have found no significant association between age and outcomes of SBTKA. Kozai et al. observed that the incidence of blood transfusions was higher among patients older than 70 years; however, the overall complication rate remained comparable across different ages [29]. The study concluded that advanced age should not be considered an absolute contraindication for SBTKA. The study conducted by Piovan et al. supports the conduct of SBTKA in elderly patients, as it improves functionality while having acceptable risks of complications [1]. Therefore, age should not be the only determining factor for excluding older patients from undergoing SBTKA. Instead, proactive measures can be implemented such as perioperative risk assessment and robust surveillance. Apart from age, several factors influenced patient LOS. Patients undergoing transfusion required higher hospitalization, in accordance with existing studies [30]. In addition, the presence of post-operative complications further extended LOS, potentially due to the need for intensified medical management, prolonged monitoring, and delayed mobilization. Among the various complications, Paralytic ileus and atrial fibrillation required significantly higher hospitalization duration. Therefore, complications and the need for transfusion may be independent predictors of LOS. The study has several limitations. First, statistical correlation analysis between age and peri-operative outcomes was not included, which could have provided a better understanding of their associations. Second, key functional outcomes such as pain relief and post-operative mobility were not assessed, which limits the ability to comment on the surgical success of SBTKA. Third, a comparative group undergoing staged or UTKA would have allowed for comparisons between these surgical approaches. Nonetheless, the large sample size of the study supports the use of SBTKA in geriatric population aged over 70 years.
Based on our experience at a multispecialty hospital with comprehensive, intensive care support and multidisciplinary expertise, SBTKA is a safe and satisfactory procedure for elderly patients above 70 years and those with comorbid conditions in the short term. Advanced age at the time of surgery is associated with poorer functional outcomes. Therefore, when SBTKA is indicated, delaying the procedure may lead to suboptimal results, emphasizing the importance of timely surgical intervention.
SBTKA is a safe and satisfactory procedure for patients over 70 years old and those with comorbid conditions in a multispecialty hospital with intensive care support. Timely intervention is crucial as delaying surgery may lead to worse functional outcomes. The study highlights the importance of careful perioperative management and timely surgical intervention in elderly patients undergoing SBTKA.
References
- 1.Piovan G, Screpis D, Natali S, Iacono V, Baldini M, Farinelli L, et al. Simultaneous bilateral total knee arthroplasty in elderly: Are there factors that can influence safety and clinical outcome? Adv Orthop 2022;2022:1989822. [Google Scholar | PubMed]
- 2.Steinmetz JD, Culbreth GT, Haile LM, Rafferty Q, Lo J, Fukutaki KG, et al. Global, regional, and national burden of osteoarthritis, 1990-2020 and projections to 2050: A systematic analysis for the global burden of disease study 2021. Lancet Rheumatol 2023;5:e508-22. [Google Scholar | PubMed]
- 3.Acharya N, Patel H. Prevalence of the knee osteoarthritis risk factors among young adult population - an observational study. Int J Health Sci Res 2023;13:158-63. [Google Scholar | PubMed]
- 4.Hsu H, Siwiec R. Knee Osteoarthritis. StatPearls; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/nbk507884[last accessed on april, 2025] [Google Scholar | PubMed]
- 5.McInnis DP, Devane PA, Horne G. Bilateral total knee arthroplasty: Indications and complications. Curr Opin Orthop 2003;14:52-7. [Google Scholar | PubMed]
- 6.Agarwala S, Menon A. Safety and efficacy of sequential simultaneous bilateral total knee arthroplasty: A single centre retrospective cohort study. J Clin Orthop Trauma 2020;11:S636-44. [Google Scholar | PubMed]
- 7.Dennis DA. Debate: Bilateral simultaneous total knee arthroplasty. Clin Orthop 2004;428:82-3. [Google Scholar | PubMed]
- 8.Ritter MA, Harty LD, Davis KE, Meding JB, Berend M. Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty. A survival analysis. J Bone Jt Surg Am 2003;85:1532-7. [Google Scholar | PubMed]
- 9.Kim YH, Choi YW, Kim JS. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br 2009;91-B:64-8. [Google Scholar | PubMed]
- 10.Ishii M, Wong K, Shimoda B, Andrews S, Au D, Nakasone CK. Do older patients fare worse following unilateral or single stage bilateral total knee arthroplasty? Arch Orthop Trauma Surg 2023;143:5283-92. [Google Scholar | PubMed]
- 11.Memtsoudis SG, González Della Valle A, Besculides MC, Gaber L, Sculco TP. In-hospital complications and mortality of unilateral, bilateral, and revision TKA: Based on an estimate of 4,159,661 discharges. Clin Orthop 2008;466:2617-27. [Google Scholar | PubMed]
- 12.Memtsoudis SG, Ma Y, Chiu YL, Poultsides L, Gonzalez Della Valle A, Mazumdar M. Bilateral total knee arthroplasty: Risk factors for major morbidity and mortality. Anesth Analg 2011;113:784-90. [Google Scholar | PubMed]
- 13.Pugely AJ, Martin CT, Gao Y, Belatti DA, Callaghan JJ. Comorbidities in patients undergoing total knee arthroplasty: Do they influence hospital costs and length of stay? Clin Orthop Relat Res 2014;472:3943-50. [Google Scholar | PubMed]
- 14.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [Google Scholar | PubMed]
- 15.Chockalingam DS, Arunkumar DC. Outcomes of total knee arthroplasty in patients aged 70 years and above. Kauverian Med J 2023;2023:13-5 [Google Scholar | PubMed]
- 16.Ritter MA, Harty LD. Debate: Simultaneous bilateral knee replacements: The outcomes justify its use. Clin Orthop 2004;428:84-6. [Google Scholar | PubMed]
- 17.Poultsides L, Memtsoudis S, Gonzalez Della Valle A, De Martino I, Do HT, Alexiades M, et al. Perioperative morbidity and mortality of same-day bilateral TKAs: Incidence and risk factors. Clin Orthop 2014;472:111-20. [Google Scholar | PubMed]
- 18.Arslan A, Utkan A, Ozkurt B. Are unilateral or staged bilateral total knee arthroplasty really safer than simultaneously bilateral TKA, or is it a myth? Acta Orthop Belg 2018;84:192-202. [Google Scholar | PubMed]
- 19.Ferguson KB, Winter A, Russo L, Khan A, Hair M, MacGregor MS, et al. Acute kidney injury following primary hip and knee arthroplasty surgery. Ann R Coll Surg Engl 2017;99:307-12. [Google Scholar | PubMed]
- 20.Nadkarni GN, Patel AA, Ahuja Y, Annapureddy N, Agarwal SK, Simoes PK, et al. Incidence, risk factors, and outcome trends of acute kidney injury in elective total hip and knee arthroplasty. Am J Orthop (Belle Mead NJ) 2016;45:E12-9. [Google Scholar | PubMed]
- 21.Yadav NK, Yadav J, Pradhan P, Kumar S. Assessment of risk factors associated with cardiac complications after total joint arthroplasty (TJA) of hip and knee. Eur J Cardiovasc Med 2024;14:133-7. [Google Scholar | PubMed]
- 22.Stroh D, Delanois R, Naziri Q, Johnson A, Mont M. Total knee arthroplasty in patients over 80 years of age. J Knee Surg 2011;24:279-84. [Google Scholar | PubMed]
- 23.Laskin RS. Total knee replacement in patients older than 85 years. Clin Orthop Relat Res 1999;367:43-9. [Google Scholar | PubMed]
- 24.Ravi B, Croxford R, Austin PC, Lipscombe L, Bierman AS, Harvey PJ, et al. The relation between total joint arthroplasty and risk for serious cardiovascular events in patients with moderate-severe osteoarthritis: Propensity score matched landmark analysis. BMJ 2013;347:f6187. [Google Scholar | PubMed]
- 25.Kirschbaum S, Hube R, Perka C, Najfeld M. Bilateral simultaneous knee arthroplasty shows comparable early outcome and complication rate as staged bilateral knee arthroplasty for patients scored ASA 1-3 if performed by a high-volume surgeon: A retrospective cohort study of 127 cases. Arch Orthop Trauma Surg 2023;144:417-24. [Google Scholar | PubMed]
- 26.Haddad B, Khan W, Mehta V, Mbubaegbu C, Qamar A. Bilateral simultaneous total knee arthroplasty: A patient-matched retrospective observational study. Open Orthop J 2015;9:499-503. [Google Scholar | PubMed]
- 27.Bawazir AO, Filimban HA, Halabi N, Bafageeh SW, Halabi R, Albukhari S, et al. Clinical outcomes of simultaneous bilateral total knee arthroplasty: A tertiary-center experience. Saudi Med J 2022;43:317-20. [Google Scholar | PubMed]
- 28.Gupta V, Arora M, Alva K, Dongre A, Thakur H, Shetty V. Factors influencing the length of hospital stay after simultaneous bilateral total knee arthroplasty. Int J Adv Jt Reconstr 2017;4:27-32. [Google Scholar | PubMed]
- 29.Kozai L, Matsumoto M, Mathews K, Andrews S, Nakasone C. Perioperative complications in patients over 70 years of age following simultaneous bilateral total knee arthroplasty. J Knee Surg 2023;36:362-7. [Google Scholar | PubMed]
- 30.Huang Y, Wang Z, Yang Q, Xie H, Wu J, Chen K. Incidence and risk factors of blood transfusion after total knee arthroplasty: A retrospective nationwide inpatient sample database study. Heliyon 2024;10:e34406. [Google Scholar | PubMed]