Cementless total hip arthroplasty is a viable option for the management of recurrent aneurysmal bone cysts with pathologic fractures of the proximal femur, even among young patients.
Dr. Apurve Parameswaran, Consultant Orthoapedic Surgeon, Department of Orthopaedics, Medicover Hospitals, Opposite Cyber Towers, Ibis Hotel Lane, HITEC City, Hyderabad - 500 081, Telangana State, India. E-mail: doctorapurve@gmail.com
Introduction: The approach to the management of aneurysmal bone cysts has evolved over time, with the focus shifting from surgery to less invasive therapeutic modalities. Curettage with or without bone grafting was considered the procedure of choice until recently but is associated with high recurrence rates. The management of recurrent aneurysmal bone cysts is challenging, especially in the presence of pathologic fractures. Scant literature is available on total hip arthroplasty for aneurysmal bone cysts of the proximal femur.
Case Report: A 27-year-old man underwent extended curettage and bone grafting for an aneurysmal bone cyst of the right proximal femur in 1999. He presented to the emergency department 17 months after the surgery with a recurrence of the aneurysmal bone cyst and a pathologic fracture of the right femoral neck. He underwent cementless total hip arthroplasty with a ceramic-on-ceramic articulation. Intraoperatively, all residual tumor lining was cleared from the proximal femur. Following the fixation of the definitive prostheses, stable hip reduction was attained. Enhanced posterior soft tissue repair was performed. He was permitted partial weight-bearing for six weeks post-operatively, and full weight-bearing thereafter. At 24 years post-operatively, the patient had a Harris Hip Score of 97, with no radiologic evidence of osteolysis or component loosening.
Conclusion: Aneurysmal bone cysts primarily affect young individuals. Their initial treatment, therefore, should focus on joint-preserving modalities. However, total hip arthroplasty must be considered for suspected recurrent aneurysmal bone cysts with pathologic fractures of the neck of the femur in patients with extensive bone loss and poor-quality residual bone.
Keywords: Aneurysmal bone cyst, total hip arthroplasty, pathologic fracture, extended curettage, bone tumor, ceramic-on-ceramic.
The term “aneurysmal bone cyst” (ABC) was coined by Jaffe and Lichtenstein, to describe bony lesions with a vascular lining and a radiographic “soap-bubble appearance” [1,2]. ABCs are solitary expansile intraosseous lesions characterized by spongy or multilocular blood-filled cystic tissue [3,4]. Although benign, they are locally destructive and may result in severe functional impairment [3]. Primary ABCs are rare and account for approximately 1% of all bone tumors [5]. They affect both sexes in an almost 1:1 ratio, with their peak incidence being in the second decade of life [3]. Nearly 20% of ABCs occur in the major long bones of the extremities, preferentially in the metaphyses, with the region around the knee being the most common site of occurrence [3,6]. The optimal management protocol for ABCs has evolved over time, with the emphasis shifting from surgery to minimally- or non-invasive treatment modalities [7]. Curettage with or without bone grafting has been considered the procedure of choice until recently [7] but is associated with high recurrence rates [3]. The management of recurrent ABCs is challenging, especially in the presence of pathologic fractures, due to the extensive bone destruction and need for defect reconstruction. Scant literature is available on total hip arthroplasty (THA) for ABCs [8-10]. We report the case of a young patient with a recurrent ABC of the proximal femur following extended curettage and bone grafting, successfully managed through THA, with a follow-up of 24 years. The patient was informed that the data concerning the case would be submitted for publication; he consented to the same.
A 27-year-old businessman with no known comorbidities presented to our outpatient clinic in the year 1999, with complaints of pain over the right hip and upper thigh, and a limp since 4 months. The pain was insidious in onset, persistent, and aggravated by sitting or squatting. There was no history of trauma or constitutional symptoms. On physical examination, tenderness was elicited around the trochanteric region. There were no neurovascular deficits. Plain radiographs of the right hip revealed an extensive lytic lesion in the femoral head and neck with sclerotic margins. No breach of cortical bone was noted. Extended curettage of the lesion was performed using a high-speed burr, and the defect was reconstructed using a bone graft from the ipsilateral iliac crest (Fig. 1). Histopathologic evaluation of the lesion confirmed the presence of an ABC. Following surgery, the patient’s pain subsided, and he recovered functionally.

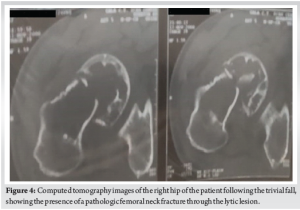
The patient presented to the emergency department 17 months following surgery, with complaints of sudden-onset severe right hip pain and inability to bear weight over the right lower limb following a trivial fall. A detailed history revealed that he had been experiencing moderate right hip pain since one month before the fall; a hip radiograph obtained elsewhere two weeks before the fall showed the reappearance of a multilocular lytic lesion in the right femoral head and neck (Fig. 2). On examination, it was noted that his right lower limb was externally rotated. His hip movements were restricted due to pain. There were no neurovascular deficits. Fresh radiographs showed the presence of a pathologic fracture in the neck of the femur (Fig. 3). A computed tomography (CT) scan confirmed the radiographic findings (Fig. 4). Given the poor bone quality, the occurrence of a fracture after a trivial fall, and the confirmed diagnosis of ABC following his first surgery, a provisional diagnosis of recurrent ABC was made. The patient was advised cementless THA.
The posterior approach to the hip was used. The fracture hematoma was drained. The femoral head was extracted easily. Standard acetabular preparation was performed. A 48 mm Plasmapore cup (BBraun-Aesculap, Tuttlingen, Germany) was implanted and fixed with two screws for additional stability. A Biolox Forte liner (CeramTec, Plochingen, Germany) with an inner diameter of 28 mm was seated onto the cup. Appropriate femoral neck resection was performed. All residual fibrous tumor lining was cleared from the proximal femur using a high-speed burr. The femoral canal was broached with A and B profilers, and an 11 mm dysplasia B profiler was found to be stable. An 11 mm primary BiCONTACT dysplasia stem (BBraun-Aesculap, Tuttlingen, Germany) was implanted. A 28 mm Biolox Forte long-neck head (CeramTec, Plochingen, Germany) was used. The hip reduction was stable. The external rotators and posterior capsule of the hip were sutured to the intertrochanteric line using pull-through osseous sutures [11]. The patient was mobilized on the 2nd post-operative day. The patient’s post-operative period was uneventful. Histopathologic examination confirmed the presence of a recurrent ABC (Fig. 5). He was permitted partial weight-bearing for 6 weeks, and full weight-bearing thereafter. He was followed up at 3 months, 1 year, 5 years, 10 years, 15 years, and 24 years post-operatively (Fig. 6). He had no complaints of squeaking or clicking. At the 24-year follow-up, his Harris Hip Score was 97. Radiographs showed no evidence of osteolysis or loosening (Fig. 6). A CT scan performed for academic purposes confirmed the absence of silent osteolysis or trunnionosis (Fig. 7).



Despite the passage of over eight decades since the first description of ABCs [1], their etiology remains elusive [12]. Several hypotheses regarding their pathogenesis have been put forward, proposing post-traumatic architectural changes of bone, vascular malformation in response to pre-existing bone tumors, or local circulatory disturbances as possible causes [5]. However, ABCs are known to develop not only secondary to pre-existing osseous lesions, but also de novo as primary bone lesions [3,5]. They have been known to regress in spite of incomplete removal in certain instances, which led to their exclusion from the neoplastic category initially [6]. Recent research, however, has shown the presence of USP6 fusion genes in several of these lesions [6], with the expression of giant cells with an osteoclast-like phenotype (CD14-, CD51+, CD68+, and cathepsin K+) [13]. These findings lend support to the perception that ABCs are neoplastic rather than reactive in nature. Viable USP6-targeted treatment options for ABCs have not been described in the literature yet [12]. Theoretically, complete surgical excision would be the most effective means of treating ABCs. However, wide or en bloc bone resection could lead to major bone loss mandating extensive reconstruction of skeletal defects, and functional impairment in several cases [3,12]. Moreover, these may result in considerable blood loss, pain, or growth disturbances [12]. Most ABCs, therefore, have conventionally been managed through curettage with or without bone grafting, and with or without the use of adjuvants (such as hydrogen peroxide, phenol, bone cement, high-speed burring, or percutaneous cryoablation), despite recurrence rates ranging from 20 to 70% in different studies [3,7]. Minimally- or non-invasive treatment modalities for ABCs have gained popularity recently. Radiotherapy and selective arterial embolization have been described, but the former poses the risk of secondary malignancies while the latter is technically demanding. Percutaneous instillation of sclerosants such as polidocanol is currently being studied as a possible first line of treatment, as it is considered safe and less technically demanding [7,14]. The optimal management of ABCs is still unclear [12]. Our patient presented with a proximal femoral ABC de novo and was managed through extended curettage and bone grafting, as was the norm at the time of his presentation. The recurrence of his tumor, though not unforeseen, presented certain surgical challenges in view of its periarticular location, the involvement of a weight-bearing joint, the extent of bone loss, the pathologic fracture, and the need for good joint functionality, given his young age. THA was preferred for his management as it permitted complete excision of the lesion and optimal joint function while preventing the added morbidity and prolonged course of rehabilitation which would have resulted from the harvest of additional bone autograft and attempted joint salvage. Ceramic-on-ceramic bearings in THA have recently been shown to have good long-term outcomes and survivorship [15]; this is consistent with the excellent outcome and prosthetic survivorship noted in our patient. The available literature on THA for proximal femoral ABCs is scant and limited by the lack of long-term outcomes. Shermato et al. [8] reported good six-month outcomes following THA for a proximal femoral ABC with hip arthritis in a 58-year-old patient. Ulici et al. [9] reported favorable outcomes at one year following THA for an 11-year-old girl with recurrent ABC following an initial embolization procedure. In their study on outcomes following bone marrow concentrate application for ABCs, Andreani et al. [10] described successful healing in 45 out of 46 patients, with the need for THA in one patient. Song et al. [16] presented a case of malignant transformation of a proximal femoral ABC in a 44-year-old patient, with no recurrence at two years following THA. Mittal et al. [17] reported good recovery in the immediate post-operative period following THA for a 23-year-old patient with ABC of the femoral head with a cortical breach. Gao-Rui et al. [18] outlined the management of a case of proximal femoral ABC with a pathologic fracture requiring THA in a patient with Graves’ disease and Moyamoya disease. To the authors’ knowledge, no prior reports in the literature have presented long-term outcomes following THA with primary endoprostheses for a recurrent proximal femoral ABC with a pathologic fracture in a young patient.
The ideal management of ABCs is unclear. Given that they primarily affect young individuals, their initial treatment should focus on joint-preserving modalities. However, the option of THA can be considered for patients suspected to have recurrent ABCs with pathologic fractures of the neck of femur, especially in the presence of extensive bone loss and poor-quality residual bone, irrespective of their age.
Recurrent ABCs of the proximal femur present therapeutic challenges in the form of bone loss, poor-quality residual bone, and/or pathologic fractures. Excision of the femoral head and neck, and total hip arthroplasty in these cases can result in good clinical outcomes, even among young patients.
References
- 1.Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst: With emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg 1942;44:1004-25. [Google Scholar | PubMed]
- 2.Lee SY, Lee SJ, Lee CS, Lee KR. Aneurysmal bone cyst originating from the first rib. Am J Surg 2008;195:104-5. [Google Scholar | PubMed]
- 3.Czerniak B. Dorfman and Czerniak’s Bone Tumors. 2nd ed. Philadelphia, PA: Elsevier Saunders; 2016. p. 1055-99. [Google Scholar | PubMed]
- 4.Sasaki H, Nagano S, Shimada H, Yokouchi M, Setoguchi T, Ishidou Y, et al. Diagnosing and discriminating between primary and secondary aneurysmal bone cysts. Oncol Lett 2017;13:2290-6. [Google Scholar | PubMed]
- 5.Cottalorda J, Bourelle S. Modern concepts of primary aneurysmal bone cyst. Arch Orthop Trauma Surg 2007;127:105-14. [Google Scholar | PubMed]
- 6.Unni KK, Inwards CY. Dahlin’s Bone Tumors. 6th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2010. p. 305-80. [Google Scholar | PubMed]
- 7.Jagiasi J, Rai AK, Sharan S, Bandebuche A. Management of aneurysmal bone cyst with pathologic femur fracture: A rare case report and review of literature. J Orthop Rep 2023;2:100119. [Google Scholar | PubMed]
- 8.Shermetaro J, Jajou L, Seidman A, McCall D. Total hip arthroplasty in a patient with a large proximal femur aneurysmal bone cyst: A case report and literature review. Arthroplast Today 2024;27:101392. [Google Scholar | PubMed]
- 9.Ulici A, Sterian AG, Tevanov I, Carp M, Dusca A, Cosma D. Aggressive development of an aneurysmal bone cyst of the proximal femur in a paediatric patient: A case report. J Int Med Res 2018;46:538-45. [Google Scholar | PubMed]
- 10.Andreani L, Shytaj S, Neri E, Cosseddu F, D’Arienzo A, Capanna R. Bone marrow concentrate in the treatment of aneurysmal bone cysts: A case series study. Stem Cells Int 2020;2020:8898145. [Google Scholar | PubMed]
- 11.Pellicci PM, Bostrom M, Poss R. Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop Relat Res 1998;355:224-8. [Google Scholar | PubMed]
- 12.Deventer N, Deventer N, Gosheger G, De Vaal M, Vogt B, Budny T. Current strategies for the treatment of solitary and aneurysmal bone cysts: A review of the literature. J Bone Oncol 202;30:100384. [Google Scholar | PubMed]
- 13.Taylor RM, Kashima TG, Hemingway FK, Dongre A, Knowles HJ, Athanasou NA. CD14- mononuclear stromal cells support (CD14+) monocyte-osteoclast differentiation in aneurysmal bone cyst. Lab Invest 2012;92:600-5. [Google Scholar | PubMed]
- 14.Rai AK, Rathod TN, Bansal D, Hadole BS, Rahman SH, Kumar KG, et al. Clinicoradiological outcome of percutaneous intralesional polidocanol in aneurysmal bone cysts: A prospective study of 43 patients in a single tertiary care centre. J Orthop 202;32:72-77. [Google Scholar | PubMed]
- 15.Alshammari MO, De Petrillo G, Epure LM, Huk OL, Zukor DJ, Antoniou J. Outcomes of ceramic-on-ceramic bearing total hip arthroplasty: A minimum 10-year follow-up study. J Arthroplasty 2023;38:S146-51. [Google Scholar | PubMed]
- 16.Song X, Qiao Y, Zhang H, Sha L, Lou J, Yu X, Liu H, et al. Malignant transformation of an aneurysmal bone cyst of the femoral neck: A case report. Exp Ther Med 2023;26:362. [Google Scholar | PubMed]
- 17.Mittal P, Prajapati P, Shah D, Chauhan K, Panchal S, Salar N. Development of an aneurysmal bone cyst of the femur head in a young patient: A case report. Int J Orthop Sci 2022;8:126-31. [Google Scholar | PubMed]
- 18.Gao-Rui C, Guo-Neng C, Wen-Xue J. Aneurysmal bone cyst of the proximal femur concomitant with Graves’ disease and Moyamoya disease: Report of a rare case. J Int Med Res 2022;50:3000605221097669. [Google Scholar | PubMed]











