Use of distraction osteosynthesis to correct bilateral brachymetatarsia of the fourth ray and stabilization of the metatarsophalangeal joint using an external rail fixator.
Dr. Prithivi Selvan K, Department of Orthopaedics, Sree Balaji Medical College and Hospital, No 7 CLC Works Road, Chrompet - 600044, Chennai, Tamil Nadu, India. E-mail: prithiviselvan@gmail.com
Introduction: Brachymetatarsia is a rare congenital deformity characterized by a shortened metatarsal, frequently affecting the fourth ray. It can result in cosmetic concerns, pain, and functional discomfort. While distraction osteogenesis has been widely used, complications, such as joint subluxation remain a concern.
Case Report: A 21-year-old female presented with bilateral congenital brachymetatarsia of the fourth metatarsal, associated with pain and deformity. She underwent gradual lengthening using external rail fixators combined with axial trans-articular K-wire stabilization of the metatarsophalangeal (MTP) joints to prevent subluxation during distraction.
Results: The procedure resulted in satisfactory lengthening (2 cm/metatarsal), restoration of the metatarsal parabola, and full functional recovery of the MTP joints (MTPJ) without subluxation or major complications. Clinical and radiological outcomes were excellent at 6 months post-operatively.
Conclusion: The modified technique combining external rail fixators and trans-articular K-wire stabilization effectively corrected bilateral fourth metatarsal brachymetatarsia. It provided enhanced joint stability during distraction and minimized complications, such as MTPJ subluxation. This approach may be preferred in cases requiring gradual lengthening with structural joint protection.
Keywords: Metatarsal lengthening, external rail fixator, brachymetatarsia, distraction osteogenesis, axial trans-articular K-wire.
The rare foot ailment known as brachymetatarsia is characterized by the metatarsals becoming shorter. The reported occurrence is between 0.02% and 0.05%, with female patients outnumbering males by approximately 25:1 [1,2]. It is believed to result from either slowed growth or early fusion of the epiphysis[3]. The toe next to the shortened metatarsal may gradually shift over the adjacent metatarsal as a result In addition to being congenital and having no known etiology, brachymetatarsia has been related to a number of systemic disorders, including sickle cell anemia, poliomyelitis, multiple epiphyseal dysplasia, enchondromatosis, Turner’s syndrome, Apert syndrome, and Down’s syndrome [4,5] Brachymetatarsia can affect more than one metatarsal and can be present in one foot or both Reports indicate that over 50% of cases occur in both feet[6]. Typically, the deformity is identified between the ages of 1 and 5. Accompanying features, such as underdevelopment of the phalanx, soft tissue underdevelopment, short fingers, and toes, or osteochondromatosis are typically seen. Patients seek treatment, often concerned about their appearance. Nonetheless, many experience discomfort in the front of the foot or toes, calluses, or difficulties with footwear due to toe alignment issues[7] . There have been numerous surgical methods reported for addressing brachymetatarsia. The techniques include acute lengthening with plates and grafts and sequential lengthening through distraction osteogenesis[8]. All the methods require the use of pins to stabilize the metatarsophalangeal (MTP) joint during the lengthening process; however, no technique has been specified[9]. This article describes a variation on the distraction osteogenesis method that prevents MTP joint (MTPJ) subluxation by incorporating an axial wire into MTP joint. The benefit of this approach is the increase in structural stability, avoiding setbacks and complications.
A 21-year-old female patient complained of deformity of both feet since her childhood associated with pain. The patient had undergone conservative modalities, such as orthotics, medical treatments, and insoles. The patient took physiotherapy with lifestyle modifications but had no pain relief. The patient felt that her feet were esthetically unpleasing (Fig. 1a and b). The patient was clinically evaluated and had shortening of bilateral fourth toes (Fig. 1a and b), tenderness over the bilateral fourth metatarsal ray, cock-up deformity over bilateral fourth toes, and sulcus sign over the plantar aspect of bilateral fourth toes. The patient had no comorbidities. The patient was evaluated for any associated syndromes and found to be negative. Pre-operative blood investigations and anesthesia fitness for surgery were obtained. A pre-operative plan was made using a bilateral foot X-ray. Anteroposterior and oblique views showed a 2-cm shortening in both fourth metatarsals (Fig. 2a, b) and a 5-mm shortening of the bilateral proximal phalanx (Fig. 2a, b) and malalignment of the Lelièvre parabolic arch[10] (Fig. 2c). A diagnosis of congenital bilateral brachymetatarsia of the fourth metatarsal was made. The patient was planned for lengthening of bilateral metatarsals using distraction osteogenesis with an external rail fixator[11,12].


Surgical technique
Under sterile aseptic precautions, under spinal and epidural anesthesia, the patient was positioned supine, and the parts were painted and draped. Skin markings for the extent of the fourth metatarsal were made under an image intensifier (Fig. 3a). A K-wire was passed into the fourth toe to immobilize the MTPJ to prevent dislocation (Fig. 3a, b, c, d, e)[13]. A 4cm skin incision was made along the fourth metatarsal extent (Fig. 3b). Subcutaneous tissue was cut and retracted. The extensor digitorum longus tendon was visualized and retracted. Four Schanz pins of size 2.5 mm were inserted (two proximally and two distally) (Fig. 3b). An osteotomy was performed after the circumferential drilling of the metatarsal shaft with a 1.5 mm K-wire with one entry and three exits. The external fixator was attached to the Schanz pins (Fig. 3c). Skin was closed in layers, and a sterile dressing was applied[14].

Post-operative management and assessment
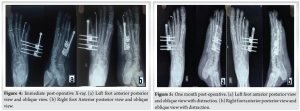
Post-operatively Immediate post op Xray taken followed by(Fig 4a,b) management with analgesics and antibiotics was started. Pin sites were regularly dressed to prevent post-operative infections. The patient was advised to be strictly non-weight bearing after surgery. Ten days post-operatively, the patient was given time for soft tissue healing and swelling to reduce. Distraction of the metatarsal was started with 0.25 mm twice daily. X-rays were taken every 10 days to check for callus formation, bone alignment, and MTPJ stability(Fig 5a,b). Distraction was conducted for 40 days, with X-ray showing regeneration of 2 cm along with callus and satisfactory arch of parabola connecting all metatarsal heads (Fig. 6a, b). The external fixator was removed after 2 months (Fig. 7a, b). After the fixator was removed and time was given for the callus to gain satisfactory strength, the patient was mobilized with full weight-bearing on day eighty[15].

Brachymetatarsia, though rare, can lead to both functional and esthetic concerns, especially when bilateral and symptomatic. The fourth metatarsal is the most frequently affected, and treatment is warranted in cases of pain, deformity, or patient-driven cosmetic dissatisfaction [1-3]. Among available surgical options, distraction osteogenesis is increasingly favored due to its ability to achieve gradual lengthening without bone grafts[12]. This method, originally described by Kawashima et al. allows for controlled soft tissue adaptation and minimization of neurovascular complications [16]. However, it carries risks, such as MTPJ subluxation, pin tract infection, and delayed union [9]. In our case, a modified technique using external rail fixators with axial trans-articular K-wire stabilization was employed. This approach ensured stability of the MTPJ during the distraction phase and helped maintain alignment of the regenerating segment, a modification supported by Peña-Martínez et al. who reported improved outcomes with joint stabilization during lengthening[13]. Compared to acute lengthening methods, which can achieve immediate correction but carry a higher risk of ischemia and graft complications [9], distraction osteogenesis enables more predictable biological regeneration[15]. Baek and Chung have shown that gradual distraction results in fewer complications and better cosmetic outcomes in multi-ray deformities[11]. Nonetheless, callotasis is not devoid of complications. Masada et al. documented pre-mature consolidation and MTPJ stiffness as frequent drawbacks[3]. Our use of a trans-articular K-wire likely contributed to the prevention of these issues in this case. Moreover, the incorporation of the Lelièvre metatarsal parabola concept guided the endpoint of distraction to restore functional forefoot geometry[10]. The results were clinically and radiologically satisfactory, with restored alignment, joint mobility, and complete resolution of the patient’s pain and deformity. No MTP subluxation, pin site infection, or hardware failure was observed, aligning with outcomes reported by Shim and Park [12]. This technique presents a reproducible and safe alternative for managing bilateral brachymetatarsia, particularly in young adults with high cosmetic expectations and good bone healing potential.
The patient’s primary complaint of pain was treated as the parabolic arch of the metatarsal head (Fig. 8a, b and 9a, b-b) was restored, along with a lengthening of 2 cm. After removal of the external fixator (Fig. 10a, b, c, d), the patient was pain-free and functionally restored.


Bilateral congenital brachymetatarsia can cause significant functional limitations and psychosocial discomfort. Distraction osteogenesis offers a safe and effective method for gradual lengthening of the metatarsal, allowing both bone and soft tissue to adapt. Our case demonstrates that with proper planning, including joint stabilization using trans-articular K-wires, excellent radiographic and clinical outcomes can be achieved with minimal complications. This technique remains a preferred approach for managing symptomatic brachymetatarsia, especially in patients concerned about cosmetic restoration and foot function.
Distraction osteogenesis remains the best method for lengthening procedures using various external fixators and reducing neurovascular complication rates associated with lengthening procedures.
References
- 1.Park YH, Lee KB, Song EK. Clinical results of distraction osteogenesis in patients with brachymetatarsia. J Bone Joint Surg Br. 2012;94(5):655–660. [Google Scholar | PubMed]
- 2.Abraham E, Behrens F. Congenital brachymetatarsia. Foot Ankle. 1985;5(3):145–151. [Google Scholar | PubMed]
- 3.Masada K, Fujita S, Fuji T, Ohno H, Yamamoto K. Complications associated with lengthening of the forearm by the callotasis method. J Pediatr Orthop. 1990;10(3):274–277. [Google Scholar | PubMed]
- 4.Blumberg SN, Hennrikus WL. Brachymetatarsia associated with multiple hereditary exostoses: A case report. J Foot Ankle Surg. 2015;54(1):115–118. [Google Scholar | PubMed]
- 5.Al Kaissi A, Klaushofer K, Grill F. Congenital brachymetatarsia and its association with syndromes. Orphanet J Rare Dis. 2009;4:7. [Google Scholar | PubMed]
- 6.Yamaguchi S, Kakiuchi M. Bilateral congenital brachymetatarsia: A case report and review. J Orthop Sci. 2004;9(3):298–300. [Google Scholar | PubMed]
- 7.Fogel GR, Mankin HJ. Congenital shortening of the fourth metatarsal: A case report and literature review. Clin Orthop Relat Res. 1981;(157):139–141. [Google Scholar | PubMed]
- 8.Engel E, Staheli LT. The natural history of congenital brachymetatarsia. J Bone Joint Surg Am. 1974;56(6):1232–1234. [Google Scholar | PubMed]
- 9.Baek GH, Chung MS, Lee YH, Gong HS, Lee S, Park SY. Complications of distraction osteogenesis in patients with brachymetatarsia. J Pediatr Orthop. 2008;28(4):403–407. [Google Scholar | PubMed]
- 10.Lelièvre J. The architecture of the metatarsal parabola. Clin Orthop Relat Res. 1982;(165):249–253. [Google Scholar | PubMed]
- 11.Baek GH, Chung MS. Clinical outcome of distraction osteogenesis for first brachymetatarsia. Foot Ankle Int. 2000;21(3):230–235. [Google Scholar | PubMed]
- 12.Shim JS, Park SJ. Correction of brachymetatarsia by distraction osteogenesis. J Pediatr Orthop. 2006;26(2):250–254. [Google Scholar | PubMed]
- 13.Peña-Martínez V, García-Martínez L, Villanueva-Martínez M, González-Díaz R. Distraction osteogenesis for brachymetatarsia with joint stabilization: Clinical results. Foot Ankle Surg. 2017;23(4):299–304. [Google Scholar | PubMed]
- 14.Paley D. Principles of Deformity Correction. Springer; 2002. p. 159–190. [Google Scholar | PubMed]
- 15.Dumbre Patel M, Puttarajappa C. Clinical outcomes of metatarsal distraction osteogenesis in congenital brachymetatarsia. Foot Ankle Spec. 2018;11(4):341–347. [Google Scholar | PubMed]
- 16.Kawashima T, Yamada A, Ueda K, et al. Lengthening of the short metatarsals by callus distraction. Plast Reconstr Surg. 1997;99(3):779–785. [Google Scholar | PubMed]









