Superior medial genicular artery pseudoaneurysm is a rare complication of Total Knee Arthroplasty that can present as recurrent hemarthrosis post-TKA. Timely diagnosis and urgent management with minimally invasive techniques such as embolization can result in a favourable functional outcome.
Dr. Rudra Prabhu, Department of Trauma and Orthopaedics, University Hospitals Birmingham NHS Foundation Trust, Birmingham B15 2GW, England. E-mail: rudra.prabhu@uhb.nhs.uk
Introduction: Vascular complications following Total Knee Arthroplasty (TKA) are rare but can be potentially life-threatening. This case report describes a rare vascular complication after an elective TKA that was successfully managed with minimally invasive interventional radiology.
Case Report: We describe the case of a 79-year-old hypertensive male who underwent a left elective primary cemented TKA. 10 days postoperatively, he presented with acute-onset pain and swelling of his left knee, lower thigh, and calf. An initial ultrasound scan ruled out deep vein thrombosis but demonstrated a large organized hematoma anterior to the femur with no active bleeding. Due to persistent pain and swelling, the patient underwent an arthroscopic washout and evacuation of the hematoma. Post-procedure, he developed recurrent knee hemarthrosis. Repeat ultrasound scan and angiography revealed the formation of a pseudoaneurysm due to active bleeding from the superior medial genicular artery. This was successfully managed with fluoroscopic embolization. At the final follow-up of 1 year, the patient was pain-free and had a good knee range of motion. He had made excellent progress in terms of daily living and quality of life.
Conclusion: Pseudoaneurysms of the superior medial genicular artery are extremely rare complications following TKA. They can present as painful and recurrent hemarthrosis and can be effectively managed with minimally invasive interventional radiology, avoiding the complications and morbidity of traditional open repair.
Keywords: Total knee arthroplasty, pseudoaneurysm, recurrent hemarthrosis, superior medial genicular artery, deep vein thrombosis, angiography.
Symptomatic pseudoaneurysms following total knee arthroplasty (TKA) are rare, with an estimated incidence of 0.01–0.09% [1]. They are commonly caused by iatrogenic trauma to the popliteal, anterior tibial, or geniculate arteries [2]. Vascular complications following TKA have been associated with vascular comorbidities, including hypertension, diabetes, peripheral vascular disease, and atherosclerosis [1]. Although extremely rare, these injuries warrant a high index of suspicion as they can evolve rapidly and pose a risk to life and limb [3]. Hence, timely diagnosis and urgent management are of vital importance.
We report a rare case of a symptomatic superior medial genicular artery (SMGA) pseudoaneurysm following an elective primary TKA in a male with long-term vascular comorbidities. The patient was successfully managed with diagnostic angiography followed by fluoroscopic embolization of the lesion.
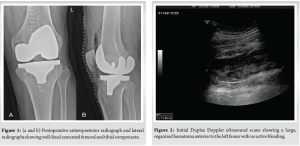
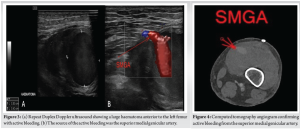
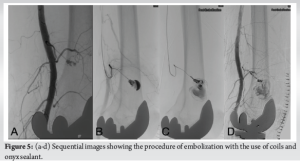
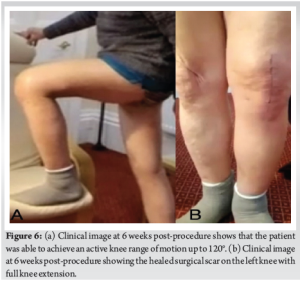
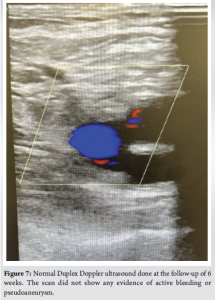
A 79-year-old male underwent an elective cemented left TKA (Stryker, Triathlon) for symptomatic knee osteoarthritis (Fig. 1). He had a background of chronic labile hypertension and atherosclerosis. The procedure was performed using the standard medial parapatellar approach using a tourniquet. There were no immediate intraoperative or perioperative complications. He was started on standard venous thromboembolism (VTE) prophylaxis using subcutaneous Enoxaparin (40 mg) to be taken once daily for 2 weeks. He was discharged on the 2nd day after surgery, having achieved knee flexion of 90°. Following discharge, the patient’s blood pressure remained high, and 10 days post-operatively, he presented to the hospital with acute-onset swelling and pain in the left knee, lower third of the thigh, and calf. Clinically, he was afebrile and hemodynamically stable, with no clinical evidence of compartment syndrome. On examination, he had a firm and non-fluctuant swelling around the knee and lower third of the thigh. There were no signs of localized infection, but there was a restricted range of motion with flexion limited to 45°. Initial bloods were unremarkable, with normal inflammatory markers and D-dimer levels. An urgent Duplex Doppler ultrasound scan showed no evidence of deep-vein thrombosis (DVT) with normal three-vessel runoff. A large, organized hematoma anterior to the left femur was demonstrated without any signs of active bleeding (Fig. 2). Due to intractable pain, the hematoma was evacuated arthroscopically. No active bleeding was noted. However, the patient developed recurrent hemarthrosis 24 h after the procedure. A repeat ultrasound scan demonstrated the recurrence of a large hematoma anterior to the left femur with the formation of a pseudoaneurysm with active bleeding. The source of the bleed was the SMGA (Fig. 3). An urgent computed tomography angiogram showed that the common femoral, superficial femoral, and popliteal arteries were patent with good three-vessel runoff. It revealed a large pseudoaneurysm arising from the SMGA and measuring 3.2 × 2.5 cm2. It was surrounded by a large hematoma extending into the left anterior thigh (Fig. 4). Following multidisciplinary discussion, the active small-vessel bleeding was managed with angiographic embolization of the atherosclerotic SMGA by the interventional radiology team. Embolization was achieved with multiple coils and onyx sealant (Fig. 5). Post-procedure, the patient made a rapid recovery and, within 6 weeks, regained 120° of knee flexion (Fig. 6). A follow-up ultrasound scan at 6 weeks showed that the hematoma in the right anterior thigh had resolved with no evidence of a pseudoaneurysm and no active bleeding (Fig. 7). At the final follow-up of 1 year, the patient had made an excellent functional recovery regarding activities of daily living and quality of life.
Pseudoaneurysms are locally contained hematomas that develop secondary to arterial injury. If untreated, they can enlarge, compress surrounding structures, or rupture, resulting in a variety of clinical presentations. These include recurrent hemarthrosis, bruising, swelling, neurological injury, or, most severely, death [4]. As the blood flow is maintained, the patient can have normal distal pulses, and the diagnosis of the vessel injury is delayed. An expanding pseudoaneurysm may compress a vein and lead to symptoms of DVT [5]. Therefore, these lesions are often diagnosed on scans that have been originally ordered to rule out DVT.
Possible etiologies of pseudoaneurysm after TKA include intraoperative injury to the vessels during medial and lateral retinacular release [4]. Posterior capsular release poses a risk of injury to the popliteal artery, whereas a lateral retinacular release has a risk of injury to the superolateral geniculate artery [6]. Other reported mechanisms during TKA include direct perforation of the vessel by a retractor or secondary effects due to the exothermic reaction seen during cementing [7].
Vascular injuries to the geniculate arteries after TKA are extremely rare, with a few anecdotal reports in the literature [5-14]. Of these, only two authors have reported involvement of the SMGA [5,14]. Most commonly, the lateral geniculate artery is affected [3], with damage occurring during exposure when lateral release is performed [11]. It is unknown whether the anatomical location and course followed by the SMGA make it vulnerable to pseudoaneurysm formation following TKA [5].
The optimal management of pseudoaneurysms depends on the artery involved and the size and location of the pseudoaneurysm [1]. The main management options include endovascular stenting, coil embolization, or open vascular repair [1]. Therefore, a multidisciplinary approach is crucial for optimal management. In our case, the bleed was successfully managed with fluoroscopic embolization using multiple coils and sealant. Open surgery to manage the bleeding would have had a very high risk of failure as the bleeder was located posteriorly and had retracted. Moreover, due to atherosclerosis, the vessels were calcified and fragile, making repair difficult. Coil embolization has shown favorable results when managing geniculate artery pseudoaneurysms [1], with angiographic coil embolization considered the best of all management options [15]. This gave an evidence base to our choice of approach. In addition, this minimally invasive procedure avoided the significant complications associated with traditional open surgery [16]. Pseudoaneurysm formation, in our case, was multifactorial. The direct mechanism of injury was likely iatrogenic trauma to the SMGA, a small-vessel measuring approximately 1.6 mm in diameter [17]. Typically, in pseudoaneurysms <1.8 cm, spontaneous thrombosis occurs [1]. However, the presence of a large hematoma in such a small vessel suggests that additional factors predisposed the vessel to injury. The patient’s long-standing hypertension, atherosclerosis, and age-related capillary fragility contributed to the pseudoaneurysm formation as well as the hematoma’s failure to clot. In addition, routine postoperative VTE prophylaxis may have hindered clotting. Therefore, in patients with recurrent hemarthrosis following TKA, particularly those with these underlying comorbidities, a high index of suspicion for pseudoaneurysm formation is warranted to enable timely diagnosis and management.
To the best of our knowledge, only two cases of SMGA pseudoaneurysms have been reported in the literature. Julien et al. reported a case of SMGA pseudoaneurysm in a 71-year-old female that was managed by open ligation of the bleeding vessel via the direct posterior approach [5]. The aneurysm was 3.5 × 2.3 cm2 in size. Gaheer et al. reported a 2.5 × 3.5 cm2 in size, spontaneously resolving SMGA pseudoaneurysm in a 68-year-old male [14]. The size of the pseudoaneurysm in our case was 3.2 × 2.5 cm2, and it was successfully managed with minimally invasive coil embolization. Our case is the first documented case successfully treated with this modality. The patient achieved excellent functional recovery without postoperative complications, highlighting coil embolization as an effective treatment modality for SMGA pseudoaneurysms.
Pseudoaneurysm formation involving the SMGA following TKA is rare but extremely devastating if not diagnosed and managed promptly. Early diagnosis and prompt management using minimally invasive techniques like embolization ensure complete recovery without hampering rehabilitation after TKA.
Urgent diagnosis and timely intervention with minimally invasive techniques are critical to ensure recovery from SMGA pseudoaneurysms that occur following TKA.
References
- 1.Puijk R, Rassir R, Kaufmann LW, Nolte PA. A pseudoaneurysm of the inferior lateral geniculate artery following total knee arthroplasty. Arthroplast Today 2022;15:120-4. [Google Scholar | PubMed]
- 2.Daniels SP, Sneag DB, Berkowitz JL, Trost D, Endo Y. Pseudoaneurysm after total knee arthroplasty: Imaging findings in 7 patients. Skeletal Radiol 2019;48:699-706. [Google Scholar | PubMed]
- 3.Sundaram K, Udo-Inyang I, Mont MA, Molloy R, Higuera-Rueda C, Piuzzi NS. Vascular injuries in total knee arthroplasty: A systematic review and meta-analysis. JBJS Rev 2020;8:e0051. [Google Scholar | PubMed]
- 4.Shaw A, Stephen A, Lund J, Bungay P, Denunzio M. Geniculate arterial pseudoaneurysm formation following trauma and elective orthopaedic surgery to the knee: 2 case reports and a review of the literature. J Radiol Case Rep 2009;3:12-6. [Google Scholar | PubMed]
- 5.Julien TP, Gravereaux E, Martin S. Superior medial geniculate artery pseudoaneurysm after primary total knee arthroplasty. J Arthroplasty 2012;27:323.e13-6. [Google Scholar | PubMed]
- 6.Law KY, Cheung KW, Chiu KH, Antonio GE. Pseudoaneurysm of the geniculate artery following total knee arthroplasty: A report of two cases. J Orthop Surg (Hong Kong) 2007;15:386-9. [Google Scholar | PubMed]
- 7.Saini P, Meena S, Malhotra R, Gamanagatti S, Kumar V, Jain V. Pseudoaneurysm of the superior lateral genicular artery: Case report of a rare complication after total knee arthroplasty. Patient Saf Surg 2013;7:15. [Google Scholar | PubMed]
- 8.Dennis DA, Neumann RD, Toma P, Rosenberg G, Mallory TH. Arteriovenous fistula with false aneurysm of the inferior medial geniculate artery. A complication of total knee arthroplasty. Clin Orthop Relat Res 1987;222:255-60. [Google Scholar | PubMed]
- 9.Langkamer VG. Local vascular complications after knee replacement: A review with illustrative case reports. Knee 2001;8:259-64. [Google Scholar | PubMed]
- 10.Moran M, Hodgkinson J, Tait W. False aneurysm of the superior lateral geniculate artery following total knee replacement. Knee 2002;9:349-51. [Google Scholar | PubMed]
- 11.Pritsch T, Parnes N, Menachem A. A bleeding pseudoaneurysm of the lateral genicular artery after total knee arthroplasty--a case report. Acta Orthop 2005;76:138-40. [Google Scholar | PubMed]
- 12.Noorpuri BS, Maxwell-Armstrong CA, Lamerton AJ. Pseudo-aneurysm of a geniculate collateral artery complicating total knee replacement. Eur J Vasc Endovasc Surg 1999;18:534-55. [Google Scholar | PubMed]
- 13.Pai VS. Traumatic aneurysm of the inferior lateral geniculate artery after total knee replacement. J Arthroplasty 1999;14:633-4. [Google Scholar | PubMed]
- 14.Gaheer RS, Chirputkar K, Sarungi M. Spontaneous resolution of superior medial geniculate artery pseudoaneurysm following total knee arthroplasty. Knee 2014;21:586-8. [Google Scholar | PubMed]
- 15.Rajani AM, Rajani K, Shah UA, Mittal AR, Sheth R, Punamiya M. Pseudoaneurysm of the lateral genicular artery following unicompartmental knee arthroplasty: A rare case report. J Orthop Case Rep 2022;12:57-60. [Google Scholar | PubMed]
- 16.Ninomiya JT, Dean JC, Goldberg VM. Injury to the popliteal artery and its anatomic location in total knee arthroplasty. J Arthroplasty 1999;14:803-9. [Google Scholar | PubMed]
- 17.Shahid S, Saghir N, Cawley O, Saujani S. A cadaveric study of the branching pattern and diameter of the genicular arteries: A focus on the middle genicular artery. J Knee Surg 2015;28:417-24. [Google Scholar | PubMed]










