Combined trochleoplasty, distal femoral osteotomy, and MPFL reconstruction, though technically demanding, provides good results in patients with recurrent patellar instability caused due to a genu valgum and trochlear dysplasia.
Dr. Prannoy Paul, Department of Orthopaedics, M.O.S.C Medical College Hospital, Ernakulam, Kerala, India. Email: prannoypaul@gmail.com
Introduction: Patellar instability is a complex condition that may be caused by a variety of factors. This case report discusses a case of recurrent patellar instability due to genu valgum, trochlear dysplasia, and medial patellofemoral ligament (MPFL) tear.
Case Report: A 16-year-old boy presented with recurrent patellar instability with a deformity of the right knee for 3 years. Investigations revealed a genu valgum, Dejour type D trochlear dysplasia, and an MPFL tear. He was treated with a medial closing wedge distal femoral osteotomy (DFO), subchondral deepening trochleoplasty, and an MPFL reconstruction as a single procedure. Patient is at 1-year follow-up with good clinical outcomes.
Conclusion: Combined trochleoplasty, DFO, and MPFL reconstruction, though technically demanding, provides good results in patients with recurrent patellar instability caused due to a genu valgum and trochlear dysplasia.
Keywords: Trochleoplasty, distal femur osteotomy, genu valgum, patellar instability.
A normal patellofemoral gliding requires a complex interaction of the bony structures, soft tissues, and the neuromuscular control. Patellar instability may be caused by a variety of factors that include intra-articular or extra-articular pathologies. Recurrent patellar instability results in a poor quality of life, injury to cartilage, and secondary osteoarthritis [1]. All the factors that are contributing to the instability must be adequately assessed, recognized, and corrected in patients with multifactorial patellar instability. Trochlear dysplasia is one of the most important intrinsic factors resulting in recurrent patellar instability. Trochlear dysplasia is found in 85% of patients with recurrent patellar instability [2]. In patients with trochlear dysplasia, a sulcus deepening trochleoplasty is a very reliable procedure that can correct the depth, length, and orientation of the sulcus [3]. Genu valgum is another important risk factor for recurrent patellar instability. The increased Q angle caused by a valgus malalignment results in maltracking of the patella, resulting in instability [4]. In a skeletally mature patient with refractory patellar instability, a varus-producing distal femoral osteotomy (DFO) will correct the Q angle and restore the normal patellar tracking [4]. A medial closing wedge osteotomy is more preferred over a lateral opening wedge osteotomy because of the advantage of immediate weight bearing, inherent stability, and the lack of a need for bone grafting, though the opening wedge osteotomy provides better fine-tuning of the intra-operative correction [5]. When both genu valgum and a trochlear dysplasia are present, both anomalies need to be corrected for optimal results and good functional outcome. We present the results of a case of genu valgum with trochlear dysplasia and medial patellofemoral ligament (MPFL) tear in a 16-year-old boy treated with a combined DFO, trochloplasty, and an MPFL reconstruction.
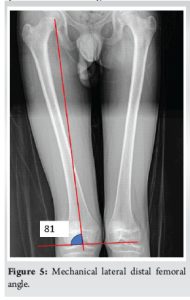
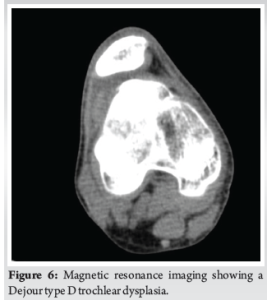
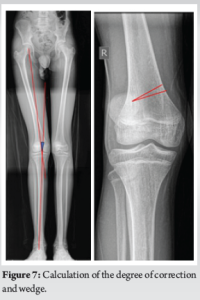
A 16-year-old boy presented to our outpatient department with a history of recurrent patellar dislocation in his right knee for the past 3 years. He also complained of a deformity of his right knee. On examination, his patella was grossly unstable, dislocating at about 30° of knee flexion (Fig. 1). Whole limb X-ray revealed a lateral mechanical axis deviation of 30 mm from the neutral (normal range – <10 mm) (Fig. 2). The opposite limb was normal. The Q angle of the right lower limb was measured to be 22°, which was abnormal (normal range 13–18°). The right knee was in valgus with a tibio-femoral angle of 15° (Fig. 3). The mechanical medial proximal tibial angle was 87.8° which was normal (normal range 85–90). However, the mechanical lateral distal femoral angle was 81°, which was abnormal (normal range 85–90) (Fig. 4 and 5). Hence, it was the distal femur that contributed to the genu valgum. The tibial tubercle–trochlear groove distance was 17 mm, which was normal (normal – under 20 mm), signifying that there was no rotational deformity. The Insall-Salvati ratio was 1.2, which was also normal (range – 0.8–1.2). Magnetic resonance imaging (MRI) revealed a Dejour Type D trochlea dysplasia (Fig. 6) with a trochlear depth of 1.2 mm (normal >3 mm) and a sulcus angle of 172 (normal <140). MRI also revealed an MPFL tear. The factors contributing to the patellar instability were recognized as the unacceptable genu valgum, trochlear dysplasia, and the MPFL tear. Considering that the patient had attained skeletal maturity and to avoid multiple procedures, a decision was made to correct all the anatomical abnormalities as a single procedure.
Surgical procedure
An anteromedial incision was made on the knee. The vastus medialis was retracted, and the osteotomy site was marked. The wedge to be taken and the degree of correction required was calculated previously based on X-rays based on geometric triangle method (Fig. 7). A 7 mm wedge was taken from the femur and the osteotomy site closed and fixed using a femoral osteotomy plate (Fig. 8). Following this, through a lateral parapatellar approach was taken for the trochleoplasty. The cartilage was sharply incised and elevated. Cancellous bone was removed using a 5 mm drill, preserving the subchondral bone stock (Trochlea Guide system – Arthrex, USA). The articular flap was then fixed to the underlying bone surface using 3 pushlock anchors and Vicryl tapes (Fig. 9). After this, the MPFL was reconstructed using a gracilis graft, fixed with 2 tunnels on the patella and to Schottle’s point on the femur.
Rehabilitation
Postoperatively, the patient was given a knee immobilizer and kept non-weight bearing for 6 weeks. Range of movement up to 45° was permitted for 2 weeks, and 90° was attained by the end of 6 weeks. Partial weight bearing was also started from 6 weeks.
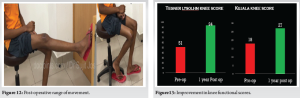
The valgus at the knee was corrected to neutral alignment (Fig. 10). The mechanical lateral distal femoral angle was corrected from 81° to 88° post-operatively. The trochleoplasty had increased the trochlear depth from 1.2 to 4 mm and the sulcus angle from 172° to 140° postoperatively (Fig. 11). The patient is currently at 1 year follow-up, and has attained full range of motion (Fig. 12). There has been no further episodes of patellar dislocation and the patient is leading an active lifestyle without apprehension or instability. The Tegner Lysholm knee score improved from a pre-operative value of 51 to a post-operative value of 94, and the Kujala knee score also showed improvement from 18 to 27 postoperatively (Fig. 13).

A variety of factors might contribute to patellar instability. For a good clinical outcome and to avoid re-operation, it is necessary to address all the etiological factors contributing to the patellar instability. This patient had an unacceptable genu valgum, which led to altered forces acting on the patella, causing maltracking, along with a Dejour type D trochlear dysplasia, making the trochlea very shallow. In addition, the MPFL was found to be torn. An effective treatment for this patient should address all these factors for correcting the patellar instability. As the patient had attained skeletal maturity and height, a decision was made to undertake a medial closing wedge DFO to address the genu valgum, a sulcus deepening trochleoplasty to address the trochlear dysplasia, and an MPFL reconstruction for the torn MPFL. A DFO is an effective procedure to address patellar instability in patients with moderate to severe valgus deformity. A varus-producing DFO corrects the malalignment, prevents maltracking and subluxation by decreasing the lateral patellar forces. Studies have reported that DFO with reconstruction of the medial soft tissues is effective in preventing in patellar maltracking [6]. A DFO can be done as a medial closing wedge or as a lateral opening wedge technique. Systematic reviews have reported no significant difference in the complication rates or re-operation rates from either techniques [7]. A medial closing wedge osteotomy negates the need for bone grafting because of the direct bone apposition and also allows for immediate weight bearing and range of movement in isolated DFOs. A medial closing wedge also has the advantage of having less symptomatic hardware on the medial side, as opposed to a lateral side implant, causing friction with the iliotibial band. Risks of this technique include under or overcorrection of the deformity, intra-articular fracture, injury to neurovascular structures, and post-operative stiffness of the knee [7]. Ultimately, the decision comes down to the surgeon’s preference. High-grade trochlear dysplasia (Dejour B and D) is an indication for trochleoplasty. Studies have reported improved outcomes after trochleoplasty in short- and mid-term results for patellar instability. There are different techniques described for trochleoplasty, including lateral facet elevation trochleoplasty, sulcus deepening trochleoplasty, subchondral deepening trochleoplasty, recession wedge trochleoplasty, and arthroscopic deepening trochleoplasty. All the techniques report good functional improvement and similar results with open and arthroscopic surgeries [8] We performed a subchondral deepening trochleoplasty in our patient. Schottle, in his study, reported only insignificant cartilage changes with maintained viability of chondrocytes after a trochleoplasty [9]. However, some authors have reported the development of arthritis in long term follow-ups [10]. Von Knoch et.al in their study reported that 30% of their patients who underwent trochleoplasty developed patellofemoral arthritis at long-term follow-up; however most of these patients who developed arthritis had chondromalacia at the time of their index procedure [11]. Some studies have suggested that in patients who have a pre-existing degenerative change in the knee, a trochleoplasty may lead to progression of trochleoplasty. However, in non-arthritic knees, there is no evidence from the literature to suggest that a trochleoplasty may lead to progression to osteoarthritis. Most studies assessing the results of trochleoplasty have reported good clinical outcomes with no re-dislocations at follow-up. [3] The MPFL is an important static stabilizer of the patella. Most patients with patellar instability would have a torn MPFL, and reconstructing the MPFL is an important step in the management of patellar instability [12]. In our case, we reconstructed the MPFL using a gracilis autograft. To the best of our knowledge, this is the first case reported in the literature that underwent a combined trochleoplasty, DFO, and MPFL reconstruction as a single procedure. Although technically demanding, this combined procedure addressed all the factors contributing to the patellar instability and provided a good functional outcome at 1-year follow-up. Future studies with longer follow-up are required to ascertain the good clinical outcomes.
A combination of trochleoplasty and a DFO is a safe and effective procedure to simultaneously treat recurrent patellar instability in patients with combined genu valgum and trochlear dysplasia. Although technically demanding, the procedure provides good clinical and functional outcomes without any major complications.
A combined trochleoplasty, DFO, and MPFL reconstruction, eventhough technically demanding, provides very good outcomes in patients with recurrent patellar instability caused due to a genu valgum and trochlear dysplasia.
References
- 1.Paschos NK. Editorial commentary: Patellofemoral instability results in osteoarthritis, and nonanatomic surgery and surgical over-constraint may also cause osteoarthritis. Arthroscopy 2023;39:358-9. [Google Scholar | PubMed]
- 2.DeVries CA, Bomar JD, Pennock AT. Prevalence of trochlear dysplasia and associations with patellofemoral pain and instability in a skeletally mature population. J Bone Joint Surg Am 2021;103:2126-32. [Google Scholar | PubMed]
- 3.Duncan ST, Noehren BS, Lattermann C. The role of trochleoplasty in patellofemoral instability. Sports Med Arthrosc Rev 2012;20:171-80. [Google Scholar | PubMed]
- 4.Parikh SN, Redman C, Gopinathan NR. Simultaneous treatment for patellar instability and genu valgum in skeletally immature patients: A preliminary study. J Pediatr Orthop B 2019;28:132-8. [Google Scholar | PubMed]
- 5.O’Malley MP, Pareek A, Reardon PJ, Stuart MJ, Krych AJ. Distal femoral osteotomy: lateral opening wedge technique. Arthrosc Tech 2016;5:e725-30. [Google Scholar | PubMed]
- 6.Tan SH, Hui SJ, Doshi C, Wong KL, Lim AK, Hui JH. The outcomes of distal femoral varus osteotomy in patellofemoral instability: A systematic review and meta-analysis. J Knee Surg 2020;33:504-12. [Google Scholar | PubMed]
- 7.Chahla J, Mitchell JJ, Liechti DJ, Moatshe G, Menge TJ, Dean CS, et al. Opening- and closing-wedge distal femoral osteotomy: A systematic review of outcomes for isolated lateral compartment osteoarthritis. Orthop J Sports Med 2016;4:2325967116649901. [Google Scholar | PubMed]
- 8.Nelitz M, Dreyhaupt J, Lippacher S. Combined trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocations in severe trochlear dysplasia: A minimum 2-year follow-up study. Am J Sports Med 2013;41:1005-12. [Google Scholar | PubMed]
- 9.Schöttle PB, Schell H, Duda G, Weiler A. Cartilage viability after trochleoplasty. Knee Surg Sports Traumatol Arthrosc 2007;15:161-7. [Google Scholar | PubMed]
- 10.Rouanet T, Gougeon F, Fayard JM, Rémy F, Migaud H, Pasquier G. Sulcus deepening trochleoplasty for patellofemoral instability: A series of 34 cases after 15 years postoperative follow-up. Orthop Traumatol Surg Res 2015;101:443-7. [Google Scholar | PubMed]
- 11.Von Knoch F, Böhm T, Bürgi ML, von Knoch M, Bereiter H. Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Joint Surg Br 2006;88:1331-5. [Google Scholar | PubMed]
- 12.Krishna Kumar MS, Renganathan S, Joseph CJ, Easwar TR, Rajan DV. Medial patellofemoral ligament reconstruction in patellar instability. Indian J Orthop 2014;48:501-5. [Google Scholar | PubMed]











