Interpositional palmaris longus autograft reconstruction represents a viable surgical option for flexor pollicis longus tendon rupture following volar plate fixation of distal radius fractures when adequate muscle belly excursion is preserved.
Dr. Yehuda Masturov, CUNY School of Medicine, New York, New York State, United States. E-mail: ymastur000@citymail.cuny.edu
Introduction: Distal radius fractures constitute one of the most prevalent upper extremity orthopedic injuries, predominantly resulting from falls onto an outstretched hand with an extended wrist. Despite volar locking plate fixation emerging as the gold standard treatment for distal radius fractures, it is associated with well-documented complications, such as flexor pollicis longus (FPL) tendon irritation and even rupture. The surgical management of FPL tendon rupture following volar plate fixation poses significant challenges due to hardware-induced tendon attrition and compromised surgical exposure. This case report is the first documented case utilizing interpositional palmaris tendon autografting for FPL tendon rupture as a complication of volar locking plate fixation with volar locking plate fixation.
Case Report: The patient is a 62-year-old left-sided dominant female who underwent successful open reduction internal fixation with a volar locking plate for a distal radius fracture treated for a distal right radius fracture with a volar locking plate. The patient was 5 months post-operatively with acute loss of thumb interphalangeal joint flexion in the absence of preceding trauma. Following patient evaluation and discussion of alternative treatments, the patient underwent concurrent hardware removal and FPL tendon reconstruction with interpositional palmaris tendon autografting.
Conclusion: A clear consensus regarding the treatment of FPL tendon ruptures in the setting of distal radius fractures treated with volar plating has not been established in the present orthopedic literature. This case represents the first reported utilization of an interpositional palmaris tendon graft for FPL rupture following distal radius volar plating. The authors of this study propose this technique as a viable treatment option for FPL tendon rupture in patients with prior distal radius fractures treated with volar locking plate fixation.
Keywords: Distal radius fracture, tendon rupture, plate fixation, autograft.
Distal radius fractures are a common injury and typically result from a fall on an outstretched hand [1]. Distal radius fractures were classically treated with dorsal plate fixation. Due to theoretical decreased tendon irritation, volar locking plate systems are being utilized for surgical fixation with increasing frequency in orthopedic surgery practices [2-5]. Though rare, volar locking plates carry an increased risk of flexor pollicis longus (FPL) tendon irritation, especially when placed distal to the watershed line [6,7]. Flexor tendon injuries associated with volar locking plates most commonly involve the FPL and include tendon irritation, partial tendon rupture, and complete tendon rupture. Treating FPL ruptures may be difficult given tendon retraction and tenosynovitis secondary to hardware irritation. Surgical methods described in treating FPL ruptures include interphalangeal (IP) joint fusion, FPL tendon advancement, palmaris longus (PL) to FPL tendon transfer, flexor digitorum superficialis from long or ring digits to FPL tendon transfer, and interposition tendon grafting [8-11]. The purpose of this case report is to describe the surgical technique of interposition tendon grafting using PL autograft for treatment of FPL rupture following open reduction internal fixation of a distal radius fracture using a volar locking plate.
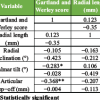
A 62-year-old left-hand dominant female presented to the emergency department after sustaining a ground-level fall with complaints of right wrist pain and right pelvic pain. Initial radiographs revealed an intra-articular comminuted distal radius fracture with approximately 40º of dorsal angulation (Fig. 1). The patient also sustained a right-sided complete sacral fracture, right anterior column acetabular fracture, right inferior rami fracture, and a left parasymphyseal rami fracture. Treatment options were discussed with the patient, and the patient elected to undergo operative intervention of both the wrist and pelvis by an orthopedic traumatologist.
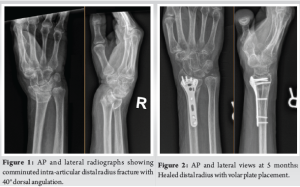
A standard volar approach was made over the flexor carpi radialis (FCR) tendon. Two separate intra-articular fragments were identified: A radial styloid component and a lunate facet component. A volar distal radius locking plate was used to provide primary fixation. The patient was placed in a volar-based splint. During the same anesthesia event, the patient underwent operative fixation of pelvis fractures as well. The patient was compliant with physical therapy protocols for distal radius fracture and pelvis fractures. Five months after the index injury, the patient presented to the orthopedic trauma clinic with acute inability to flex the right thumb without an inciting event. The patient was subsequently referred to the senior author for further management. Radiographs at that time revealed a well-healed distal radius fracture with plate placement on the volar rim (Fig. 2). Examination revealed inability to flex the thumb IP joint, with a lack of tenodesis effect, which confirmed atraumatic FPL rupture. Treatment options were discussed, and the patient elected to undergo removal of hardware and FPL tendon reconstruction with PL interpositional graft. The operation began with a standard volar approach over the FCR tendon. The proximal FPL tendon stump was found to be completely ruptured and the surrounding tenosynovium was sharply excised. There was an excellent excursion of the proximal FPL muscle belly, which was found to be >2 cm. The median nerve was found to be adherent to the FPL and was subsequently neurolyzed. The previously placed plate and screws were removed and fluoroscopic imaging confirmed a well-healed fracture. An incision was made over the thumb in a Brunner-like fashion. The A1 pulley was released. The distal FPL tendon stump was then pulled through the wound (Fig. 3). A 15 cm length of PL tendon was harvested. The PL tendon autograft was secured using a Pulvertaft weave technique into the distal portion of the FPL tendon and reinforced with 3-0 braided polyester suture (Fig. 4). The tendon was delivered through the palm and out through the forearm incision. The wrist was held in neutral position while appropriate tension was placed and a first proximal Pulvertaft weave was placed. The wrist was taken through a full range of motion and appropriate tension was confirmed (Fig. 5). The thumb maintained 5° of flexion with full wrist flexion. The patient was placed in a thumb-based dorsal blocking splint and made non-weight bearing with the right upper extremity.

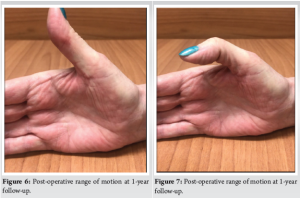
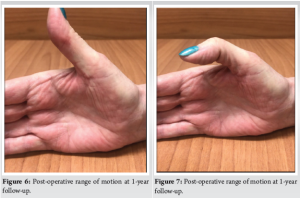
Post-operatively, the patient described numbness and burning over the ulnar aspect of the long finger and the radial aspect of the ring finger, which was attributed to median nerve irritation. At 5 weeks post-operatively, the patient was started on gabapentin 300 mg nightly to help with symptoms. The patient began occupational therapy at 2 weeks and was placed into a custom wrist brace. At 1-year follow-up the patient had regained satisfactory function and range of motion of her thumb (Fig. 6 and 7).
FPL rupture is a rare and serious complication when using volar plate systems in distal radius fracture fixation. Asadollahi and Keith [12] reviewed 47 cases from 21 studies that documented flexor tendon rupture as a complication of distal radius plating. The most commonly ruptured flexor tendon in the review was FPL (n = 27), followed by the flexor digitorum profundus to the index finger (n = 7). The majority of FPL ruptures occurred in women ages 60–70. This is likely given the increased incidence of distal radius fractures in women secondary to osteoporosis and likely decreased tensile properties of tendons as people age. Treatment of flexor tendon rupture after distal radius volar plating may be difficult, given tenosynovitis and degradation in tendon tissue secondary to irritation from volar plates. Hardware removal is indicated in the treatment of FPL rupture secondary to prominent hardware. Following the removal of symptomatic hardware, various methods have been described to repair the ruptured tendon. The PL tendon serves as a reasonable autograft given its proximity to FPL and suitable length and diameter [12]. To perform a tendon graft, an intact FPL muscle belly is required. Matev [13] stated that if passive stretch of the FPL-tendon of 1–1/2 cm is preserved, restoration of IP flexion would be adequate, while 3–4 cm of FPL tendon passive stretch, one would expect complete restoration of IP flexion. In our patient, passive excursion of the FPL tendon was greater than 2 cm intraoperatively, so functional IP joint flexion could be expected. Kilgore et al. [14] described needing 20–30° of IP joint flexion for functional use. Berger et al. [11] described a case series of four PL tendon transfers in the setting of FPL rupture after distal radius volar plating. They measured mean active IP flexion in operative and contralateral thumbs (44° and 80°, respectively). Patients reported excellent functional results despite having decreased flexion and opposition. This is likely given that the adductor pollicis is the principal muscle for thumb pinch and grasp [14]. There are no present guidelines for the various surgical options for FPL rupture following distal radius volar plating. The authors of this paper conclude that PL tendon interpositional autograft should be considered for FPL reconstruction for patients with intact PL tendon and FPL muscle belly. To our knowledge, there is a case series of using PL autografts out of Belgium [11], but interpositional PL autograft for FPL rupture has not been described in the literature from the United States.
FPL tendon rupture represents a rare but significant complication following volar plate fixation of distal radius fractures. Although various reconstructive techniques have been described in the literature, no established consensus exists regarding optimal surgical management. This case demonstrates the successful application of interpositional PL autograft reconstruction for FPL rupture in the setting of prior volar plate fixation. The technique provided satisfactory restoration of thumb function with excellent patient-reported outcomes at one-year follow-up. Consideration of this reconstructive approach is recommended in patients with adequate FPL muscle belly excursion and intact PL tendon.
This case report is the first in orthopedic literature to describe the successful reconstruction of a ruptured FPL tendon utilizing interpositional palmaris tendon autograft with antecedent distal radius volar plate fixation. Future surgical management of FPL tendon ruptures in the setting of distal radius volar plate fixation may utilize the described surgical technique to optimize patient mobility post-operatively.
References
- 1.Pogue DJ, Viegas SF, Patterson RM, Peterson PD, Jenkins DK, Sweo TD, et al. Effects of distal radius fracture malunion on wrist joint mechanics. J Hand Surg Am 1990;15:721-7. [Google Scholar | PubMed]
- 2.Orbay JL, Touhami A. Current concepts in volar fixed-angle fixation of unstable distal radius fractures. Clin Orthop Relat Res 2006;445:58-67. [Google Scholar | PubMed]
- 3.Rozental TD, Blazar PE, Franko OI, Chacko AT, Earp BE, Day CS. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. J Bone Joint Surg Am 2009;91:1837-46. [Google Scholar | PubMed]
- 4.Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma 2007;21:316-22. [Google Scholar | PubMed]
- 5.Smith DW, Henry MH. Volar fixed-angle plating of the distal radius. J Am Acad Orthop Surg 2005;13:28-36. [Google Scholar | PubMed]
- 6.Johnson NA, Cutler L, Dias JJ, Ullah AS, Wildin CJ, Bhowal B. Complications after volar locking plate fixation of distal radius fractures. Injury 2014;45:528-33. [Google Scholar | PubMed]
- 7.Soong M, Earp BE, Bishop G, Leung A, Blazar P. Volar locking plate implant prominence and flexor tendon rupture. J Bone Joint Surg Am 2011;93:328-35. [Google Scholar | PubMed]
- 8.Schmitt S, Mühldorfer-Fodor M, Van Schoonhoven J, Prommersberger KJ. Restoration of thumb flexion at the interphalangeal joint by transposition of the flexor digitorum superficialis tendon from the ring finger. Oper Orthop Traumatol 2013;25:321-30. [Google Scholar | PubMed]
- 9.Schneider LH, Wiltshire D. Restoration of flexor pollicis longus function by flexor digitorum superficialis transfer. J Hand Surg Am 1983;8:98-101. [Google Scholar | PubMed]
- 10.Urbaniak JR, Goldner JL. Laceration of the flexor pollicis longus tendon: Delayed repair by advancement, free graft or direct suture. A clinical and experimental study. J Bone Joint Surg Am 1973;55:1123-48. [Google Scholar | PubMed]
- 11.Berger P, Duerinckx J. Flexor pollicis longus tendon rupture after volar wrist plating: Reconstruction with palmaris longus interposition graft. Acta Orthop Belg 2017;83:467-72. [Google Scholar | PubMed]
- 12.Asadollahi S, Keith PP. Flexor tendon injuries following plate fixation of distal radius fractures: A systematic review of the literature. J Orthop Traumatol 2013;14:227-34. [Google Scholar | PubMed]
- 13.Matev IB. Reconstructive Surgery of the Thumb. Brentwood: Pilgrim’s Press; 1983. p. 50-6. [Google Scholar | PubMed]
- 14.Kilgore ES Jr., Newmeyer WL, Graham WP 3rd, Brown LG. The dubiousness of grafting the dispensable flexor pollicis longus. Am J Surg 1976;132:292-6. [Google Scholar | PubMed]