Knee arthrodesis is a reliable salvage procedure in cases of failed Ilizarov fixation for complex periarticular fractures, offering pain relief and functional limb stability.
Dr. Raj Suhas Kamble, D. Y. Medical College, Pune, Maharashtra, India. E-mail: rajkamble201212@gmail.com
Introduction: The Ilizarov technique is a widely used method for managing complex fractures, especially those involving periarticular regions such as the distal femur and proximal tibia. Ilizarov is a versatile process which can also be used for limb lengthening, deformity correction and for septic and aseptic non-unions.
Case Report: We present the case of 48-year-old male with non-union of proximal tibia and distal femur fracture with Ilizarov in situ. A floating knee on the right side was unsuitable for open reduction and internal fixation due to poor skin health. Ilizarov fixation was planned for the patient. This instance demonstrates the difficulties associated with floating knee. The technique’s limits in treating specific periarticular fractures are highlighted by the Ilizarov fixation’s failure in this instance.
Conclusion: An efficient salvage technique that provides permanent pain relief and functional stability is knee arthrodesis. The need of customized treatment planning in handling complicated fracture situations is highlighted by this example.
Keywords: Ilizarov fixation, failed fracture fixation, periarticular fractures, knee arthrodesis, salvage technique, functional rehabilitation.
For complicated fractures, especially those with substantial comminution or bone loss, the Ilizarov procedure is a commonly used treatment. Through distraction osteogenesis, it has the benefit of stabilizing fractures and promoting bone healing [1,2]. Patients may have crippling pain and limited mobility as a result of such failures, requiring the use of other therapies. In these situations, knee arthrodesis, a salvage treatment, is a good choice, especially if joint preservation is no longer practical [3,4]. Arthrodesis is a good option in some Ilizarov failure situations because it provides permanent pain relief, enhances functional stability, and permits weight bearing.
The case report’s justification is that complicated fractures involving substantial bone loss or comminution frequently pose difficult therapeutic problems. Due to its capacity to stabilize fractures and encourage bone regeneration through distraction osteogenesis, the Ilizarov technique has become a mainstay in the management of such injuries.
However, despite its efficacy, treatment failures can occur, leading to persistent pain, non-union, or compromised joint function. In these difficult scenarios, where conventional joint-preserving options are exhausted, knee arthrodesis serves as a reliable salvage procedure. It offers definitive pain relief, restores limb stability, and enables functional weight-bearing. Evaluating such alternative approaches is crucial for guiding clinical decision-making in cases of Ilizarov failure, ensuring optimal patient outcomes [5,6].
A 48-year-old male presented with persistent right knee pain for the past 9 months, following a traumatic injury sustained in a road traffic accident. The initial trauma resulted in comminuted fractures of the distal femur and proximal tibia. There was no history of head injury, loss of consciousness, or ear, nose, and throat bleeding.
Initial evaluation
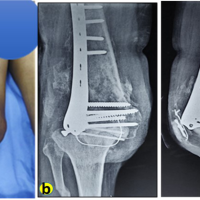
On admission, the patient’s local examination revealed poor skin integrity over the right knee, with evidence of bruising and abrasions (Fig 1). The skin was at risk of post-operative infection, and this influenced the decision to proceed with a primary Ilizarov fixation, instead of internal fixation. The fracture was classified as a Gustilo-Anderson Type III B open fracture, and further categorized as AO/OTA Classification 33C2 for the distal femur and 41C2 for the proximal tibia.

Surgical history
The Ilizarov fixation was performed on January 16, 2024. The construct included three full rings on the femur and three on the tibia, connected by threaded rods with tensioned wires. A bone transport protocol was initiated due to segmental bone loss (Fig 2). The distraction rate followed standard principles (1 mm/day in four increments), and docking site compression was performed later. Prophylactic antibiotics were administered, and regular pin site care was ensured.

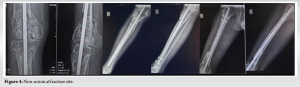
The patient was followed up for at least 4 months postoperatively (Fig 3 and 4). Serial radiographs showed callus formation at the distal femur, but incomplete consolidation at the docking site. There was partial resolution of infection and improvement in soft-tissue status.
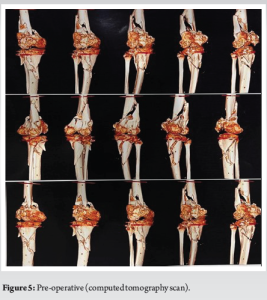
On August 13, 2024, due to inadequate radiographic signs of union and persistent discomfort, the Ilizarov fixator was removed (Fig 5). A computed tomography (CT) scan was performed, revealing non-union at the femoral-tibial junction, with sclerotic bone ends, a persistent fracture gap of approximately 1.5 cm, and no evidence of bridging trabeculae – confirming atrophic non-union.
On physical examination
Swelling
Localized over the medial and suprapatellar region of the right knee.
Abrasions
Multiple abrasions noted on the anterior aspect of the left leg, each measuring approximately 2–3 cm in diameter, with granulation tissue indicating partial healing.
Tenderness
Localized over the medial joint line and anterior knee, exacerbated by movement.
Range of motion (ROM)
Severely restricted; flexion limited to 20°, extension fixed at 15° flexion, with pain throughout the range.
Distal neurovascular status
Intact; no sensory or vascular deficits noted. Further imaging (such as magnetic resonance imaging [MRI]) and laboratory studies for inflammatory markers are recommended to evaluate the current status of the fracture site and soft-tissue structures around the knee joint.
Given the non-union, poor joint function, and prior failure of limb-salvage fixation, knee arthrodesis was planned as a salvage procedure to restore limb stability and allow for weight-bearing. Further imaging including MRI was advised to assess cartilage and ligament integrity, while C-reactive protein and erythrocyte sedimentation rate levels were ordered to rule out ongoing infection.
This case presents a failed outcome following Ilizarov external fixation for a complex periarticular injury involving both the distal femur and proximal tibia. Despite initial stabilization, the patient developed non-union and significant functional limitations, eventually requiring knee arthrodesis [7,8].
Several key factors may have contributed to the failure of Ilizarov fixation in this case. First, the fracture pattern – comminuted and periarticular in nature – posed inherent challenges to successful bone regeneration and alignment [9]. Second, although the Ilizarov technique is widely regarded for its versatility and ability to manage bone defects and infections, its success is highly dependent on proper application, patient selection, and adherence to distraction protocols [10,11].
This patient’s post-operative course was characterized by radiological evidence of non-union, limited ROM, and ongoing pain [12,13]. Sclerotic bone ends and a prolonged fracture gap were seen on a CT scan, indicating an atrophic non-union that could be caused by insufficient biological activity or mechanical stability [14-16]. Unfortunately, it is unable to draw firm findings due to the lack of documentation regarding the soft-tissue handling, fixation specifics, and distraction and docking techniques. However, it is impossible to completely rule out the potential of technological shortcomings such as bad alignment, insufficient compression at the docking location, or an inappropriate ring arrangement [17-19].
This instance further emphasizes how crucial it is to understand Ilizarov fixation’s limitations in periarticular fractures, particularly when soft-tissue integrity is at risk [20]. Although the device works well for diaphyseal rebuilding, it loses effectiveness close to joints where it is more difficult to preserve function and avoid stiffness. Even though there was no obvious infection, periarticular fibrosis and pain were probably caused by the hardware’s close closeness to the knee [21,22].
Knee arthrodesis was considered the best salvage option due to the patient’s ongoing discomfort and radiologic non-union [23]. Historically, arthrodesis has been saved for situations in which joint preservation is no longer feasible, such as post-infectious arthritis, failed total knee replacements, or persistent instability after several unsuccessful fixations. In this case, it provided a limb that was pain-free, stable, and able to support weight again [24].
This example demonstrates the necessity of customized surgical planning in addition to the biological and technological difficulties involved in treating periarticular fractures with Ilizarov techniques. Prolonged handicap can be avoided by promptly identifying fixation failure and moving on to definitive salvage techniques like arthrodesis.
This example demonstrates the limitations of Ilizarov fixation in complex knee periarticular fractures, especially when fracture patterns are unfavorable and soft-tissue conditions are not ideal. Conversion to knee arthrodesis was required due to the protracted treatment’s inability to establish union and restore function. A dependable salvage option, knee arthrodesis offered functional restoration, enhanced stability, and permanent pain alleviation. When employing Ilizarov procedures, this example highlights the significance of meticulous patient selection, accurate surgical execution, and diligent post-operative monitoring. A tailored, patient-centered approach remains essential in determining the optimal treatment strategy for complex limb trauma.
Giant cell tumors (GCT) of the fibular head are rare and may present with peroneal nerve involvement, posing unique diagnostic and surgical challenges. Early imaging and careful surgical planning are essential to preserve nerve function and achieve complete tumor excision. This case highlights the importance of considering GCT in the differential diagnosis of proximal fibular swellings with neurologic symptoms and demonstrates that nerve-sparing surgery is achievable even in anatomically complex regions.
References
- 1.Adejuyigbe B, Gharpure M, Wahle CF, Kallini JR. Distraction osteogenesis: A comprehensive review. Appl Biosci 2024;3:503-16. [Google Scholar | PubMed]
- 2.Ghorab AS, Elngehy AA, Salama AM, Aziz HE. Management of tibial bone defects by segmental bone transport using Ilizarov technique. Zagazig Univ Med J 2024;30:552-60. [Google Scholar | PubMed]
- 3.Abdelhadi E, Zakaria Abdel-Salam ZM, Elhefnawy M. Evaluation of complex tibial plateau fractures with ilizarov external fixation with or without minimal internal fixation. Zagazig Univ Med J 2025;31:613-23. [Google Scholar | PubMed]
- 4.Wood JH, Conway JD. Advanced concepts in knee arthrodesis. World J Orthop 2015;6:202-10. [Google Scholar | PubMed]
- 5.Zajonz D, Zimmerlich B, Möbius R, Edel M, Przybyl J, Höch A, et al. Knee arthrodesis as last resort for persistent knee joint infections: Comparison of extramedullary and intramedullary treatment. Orthopade 2021;50:207-13. [Google Scholar | PubMed]
- 6.Gramlich Y, Parvizi J. Enough is enough: Salvage procedures in severe periprosthetic joint infection. Arthroplasty 2023;5:36. [Google Scholar | PubMed]
- 7.Nozaka K, Miyakoshi N, Sato T, Shimada Y. Ilizarov external fixation for a periprosthetic tibial fracture in severe osteoporosis: A case report. BMC Musculoskelet Disord 2020;21:145. [Google Scholar | PubMed]
- 8.Schweser KM, Crist BD. Use in arthrodesis. In: Essential Biomechanics for Orthopedic Trauma: A Case-Based Guide. Berlin: Springer; 2020. p. 283-97. [Google Scholar | PubMed]
- 9.Ferguson, J., Morgenstern, M., Stubbs, D., & McNally, M. (2021). Infected nonunions around the knee. In A. Nauth, D. Sanders, B. Hanson, & P. D. Henry (Eds.), Knee fractures (pp. 159–184). Cham: Springer. [Google Scholar | PubMed]
- 10.Qin S, Zang J, Jiao S, Pan Q, Shi L, Zhu Y, et al. Application of the ilizarov technique. In: Lower Limb Deformities: Deformity Correction and Function Reconstruction. Singapore: Springer Singapore; 2020. p. 67-110. [Google Scholar | PubMed]
- 11.Miraj F, Nugroho A, Dalitan IM, Setyarani M. The efficacy of ilizarov method for management of long tibial bone and soft tissue defect. Ann Med Surg (Lond) 2021;68:102645. [Google Scholar | PubMed]
- 12.Thippeswamy PB, Nedunchelian M, Rajasekaran RB, Riley D, Khatkar H, Rajasekaran S. Updates in postoperative imaging modalities following musculoskeletal surgery. J Clin Orthop Trauma 2021;22:101616. [Google Scholar | PubMed]
- 13.Ibrahim MA, Alhomayani KM, Gaber U, Bukhary HA, Nematallah SA, Elgahel MM. Radiographic and functional results of Ilizarov fixation in the management of nonunion of tibia and femur fractures: A retrospective case series. Ann Saudi Med 2024;44:146-52. [Google Scholar | PubMed]
- 14.Panteli M, Vun JS, Pountos I, J Howard A, Jones E, Giannoudis PV. Biological and molecular profile of fracture non-union tissue: A systematic review and an update on current insights. J Cell Mol Med 2022;26:601-23. [Google Scholar | PubMed]
- 15.Dimartino S, Pavone V, Carnazza M, Cuffaro ER, Sergi F, Testa G. Forearm fracture nonunion with and without bone loss: An overview of adult and child populations. J Clin Med 2022;11:4106. [Google Scholar | PubMed]
- 16.Qin S, Jiao S, Zang J, Wang Y, Han Y, Pan Q, et al. Nonunion, bone defects and osteomyelitis. In: Lower Limb Deformities: Deformity Correction and Function Reconstruction. Singapore: Springer Singapore; 2020. p. 515-70. [Google Scholar | PubMed]
- 17.Boero S, Marrè Brunenghi G, Riganti S, Torchia S. Role of proximal tibiofibular fixation in leg lengthening with the Ilizarov method in the achondroplastic patient. J Pediatr Orthop B 2023;32:66-71. [Google Scholar | PubMed]
- 18.Scott H, Marti J, Witte P. Fracture classification, decision-making and bone healing. In: Feline Orthopaedics. United States: CRC Press; 2022. p. 43-52. [Google Scholar | PubMed]
- 19.Trompeter AJ, Knight R, Parsons N, Costa ML. The orthopaedic trauma society classification of open fractures. Bone Joint J 2020;102-B:1469-74. [Google Scholar | PubMed]
- 20.Zhang Y, Wang H, Wang T, Chen W, Zhu Y. Biomechanics of the fracture fixation. In: Frontiers in Orthopaedic Biomechanics. Berlin: Springer; 2020. p. 301-37. [Google Scholar | PubMed]
- 21.Çelik M, Bayrak A, Öztürk V, Kızılkaya C, Avkan MC. Functional and radiological comparison and evaluation of Gustilo-Anderson type 3 open tibia fractures treated with an ilizarov external fixator. Med J Bakirkoy 2024;20:308-14. [Google Scholar | PubMed]
- 22.Shchepkina EA, Solomin LN, Lebedkov IV, Netylko GI, Anisimova LO, Sheridan GA, et al. Distraction osteogenesis in combined sequential use of external fixation and nailing (lengthening and then nailing): An experimental study in rabbits. J Orthop Res 2024;42:1727-37. [Google Scholar | PubMed]
- 23.Mercurio M, Gasparini G, Cofano E, Zappia A, Familiari F, Galasso O. Knee arthrodesis for periprosthetic knee infection: Fusion rate, complications, and limb salvage-a systematic review. Healthcare (Basel) 2024;12:804. [Google Scholar | PubMed]
- 24.Valerio MS, Pace WA, Dolan CP, Edwards JB, Janakiram NB, Potter BK, et al. Development and characterization of an intra-articular fracture mediated model of post-traumatic osteoarthritis. J Exp Orthop 2023;10:68. [Google Scholar | PubMed]