Melorheostosis is an uncommon condition characterized by limited case reports, exhibiting a multitude of clinical and radiological manifestations that are imperative for orthopedic specialists to comprehend
Dr. Divya Nand Pandey, Department of Orthopaedics, GSVM Medical College and Associated LLR Hospital, Kanpur - 208002, Uttar Pradesh, India. E-mail: draanand29@gmail.com
Introduction: Melorheostosis is an extremely rare, non-hereditary bone disorder characterized by its distinctive radiographic feature of flowing hyperostosis, reminiscent of dripping candle wax, typically appearing unilaterally in long bones . Initially proposed by Leri and Joanny in 1922 , the exact cause remains largely speculative, and treatment is primarily symptomatic. This condition predominantly affects a single limb, with a higher incidence in the lower extremities, while axial skeletal involvement is uncommon.
Case Report: We present a severe melorheostosis affecting the left lower limb, accompanied by ipsilateral pelvic involvement and soft tissue abnormalities in the lumbar region, while the contralateral side remained unaffected. Radiographic imaging revealed substantial heterotopic ossification and dense hyperostosis in the periarticular soft tissues of nearly all bones in the affected limb, from the femur to the distal phalanges of the toes. Patient’s physical examination identified functional scoliosis, joint rigidity and distortion, and significant edema and deformity of the left extremities. In addition, a soft tissue mass over the L3 region, later identified as an arteriovenous malformation through fine needle aspiration cytology, was observed. The right side was entirely normal.
Conclusion: This case details a unique presentation of severe monomelic melorheostosis in a 28-year-old Indian woman, involving the left lower limb, pelvis, and lumbar soft tissues. Radiographic and computed tomography imaging revealed extensive cortical hyperostosis with associated soft tissue ossifications. We discuss the clinical presentation, diagnostic approach, and management of this intricate condition, supported by illustrative imaging.
Keywords: Melorheostosis, rare, dripping candle wax, Benign.
Melorheostosis is a benign but progressive bone dysplasia primarily affecting a single limb in a segmental fashion [1]. This disorder can lead to pain, edema, joint contractures, and skeletal deformities. Its hallmark radiological feature is cortical hyperostosis resembling dripping candle wax [2]. Laboratory findings remain unremarkable, showing normal serum calcium, erythrocyte sedimentation rate, alkaline phosphatase, and C-reactive protein levels [3]. The disease typically presents early in life, progressing insidiously, requiring symptomatic management with analgesics, and anti-inflammatory medications.
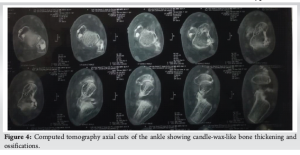
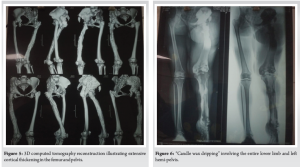
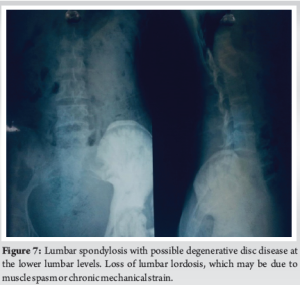
A 28-year-old woman arrived with a 20-year history of gradually increasing pain, swelling, and deformity of the left hemibody, particularly the lower limb, accompanied by functional scoliosis with right-side convexity. Symptoms first appeared in childhood. Upon examination, notable hypertrophy and joint stiffness were observed in the left lower limb (Fig. 1), with a 4.5 cm length discrepancy in the left lower limb, left-sided genu valgum, foot varus, and equinus deformity, along with hyperpigmentation and a scar over the left ankle. The skin over the lumbar region exhibited hyperpigmentation with a 4.5 cm soft tissue swelling at the L3 level (Fig. 2) and nodular thickening over the medial malleolus. Hip and knee fixed flexion deformities measured 25° and 90°, respectively. Digital radiographs and computed tomography (CT) scans demonstrated diffuse cortical thickening and hyperostosis affecting the pelvis, femur, tibia, talus, calcaneus, and tarsal bones of the left side, with partial joint fusion and medullary cavity obliteration, characteristic of “candle wax dripping” [4] (Fig. 3-7).

Ultrasound revealed a swelling in the lower back with multiple tortuous vascular channels in the lumbar region exhibiting both arterial and venous flow, with arterial flow showing a low-resistance waveform. Fine needle aspiration cytology confirmed the presence of an arteriovenous malformation [5]. Laboratory analysis revealed no abnormalities in serum calcium, erythrocyte sedimentation rate, alkaline phosphatase, or C-reactive protein levels. Conservative management led to mild symptom relief at the 6-month follow-up.
Melorheostosis, first designated in 1922 by Leri and Joanny [6], remains an exceedingly rare condition that can manifest at any age with equal prevalence among both sexes. Its etiology remains unclear, though hypotheses include defects in mesenchymal cell differentiation (notably mutations in LEMD3)[7], vascular anomalies, and inflammatory processes, though none have been definitively confirmed. In osteoblastic regulation, research by Kim J-E has indicated that adhesion proteins, particularly the transforming growth factor ß-induced gene product, may be downregulated. This occurrence might lead to hyperostosis and associated soft tissue abnormalities [8]. One conceivable explanation is a loss-of-function mutation in the LEMD3 gene (12q12–12q14.3), which is essential for bone morphogenic protein and tumor growth factor-β pathways. These genetic links emphasize the need for further research to clarify causative mechanisms and explore the potential of gene therapy in disease management. Manifestations vary widely, from asymptomatic cases to severe pain and deformity. Symptoms usually develop insidiously, presenting with pain, stiffness, skin changes, and skeletal deformities. Our patient reported pain beginning at age eight, progressing gradually with worsening deformity. Lesion distribution ranges from monomelic (affecting one limb, the most common form) to hemimelic (involving both upper and lower limbs). It may be monostotic (impacting a single bone) or polyostotic (affecting multiple bones). In this case, the disease presented in a hemimelic, polyostotic form, an atypical occurrence. While melorheostosis predominantly affects long bones, axial skeletal involvement is rare. In addition, it has been linked to neoplasms, such as malignant fibrous histiocytoma, osteogenic sarcoma, and dermoid tumors. Differential diagnoses include osteopathic striata, parosteal osteosarcoma, osteopoikilosis, myositis ossificans, and osteoma, particularly in forme fruste cases. In this patient, the diagnosis was straightforward based on clinical presentation, radiographic findings, CT imaging, and histological features. Diagnosis relies primarily on radiographic findings, with classic “dripping candle wax” appearance distinguished by cortical hyperostosis, increased bone thickness, linear density extending into cancellous bone [9]. In this case, radiographic evidence clearly supported the diagnosis. Laboratory investigations were unremarkable, a hallmark of this condition. Histopathological findings generally lack specificity, with a heterogeneous mix of mature and immature bone forming a dense structure with elevated trabecular bone. While osteoclastic activity has been uncommon, mild osteoblastic proliferation is frequently observed, aligning with findings in this case. Treatment is predominantly symptomatic, with most patients undergoing non-operative management. Surgery is reserved for cases involving contractures and severe deformities, including tendon lengthening, osteotomies, excision of hyperostotic bone, or, in extreme cases, amputation [10]. Our patient was prescribed aceclofenac 100 mg twice daily, which provided symptom relief. Melorheostosis remains an exceedingly rare disorder marked by linear hyperostosis laterally the cortical bone. On the clinical level, it manifests localized pain and deformity, and the diagnosis is determined through combining of imaging and clinical assessment. No definitive treatment exists, as well as management focuses primarily on symptomatic relief.
This case highlights the importance of early recognition of melorheostosis and the necessity for comprehensive imaging in extensive disease manifestations. Conservative therapy remains the foundation of management, but additional studies are needed to explore targeted therapeutic approaches.
Always think common first, but don’t forget to explore the rare. Melorheostosis is an infrequent benign mesenchymal disorder that affects both the skeletal system and the associated soft tissues. Radiologically, it exhibits a distinctive “dripping candle wax” pattern. Due to its rarity, this condition is frequently overlooked; therefore, it should be considered in the differential diagnosis of patients presenting with atypical and uncommon manifestations.
References
- 1.Kotwal A, Clarke BL. Melorheostosis: A rare sclerosing bone dysplasia. Curr Osteoporos Rep 2017;15:335-42. [Google Scholar | PubMed]
- 2.Greenspan A, Azouz M. Bone dysplasia series. Melorheostosis: Review and update. Can Assoc Radiol J 1999;50:324-30. [Google Scholar | PubMed]
- 3.Venkatesh R. Principles of surgical management of musculoskeletal conditions. Best Pract Res Clin Rheumatol 2008;22:483-98. [Google Scholar | PubMed]
- 4.Wenokor G, Suster D, De Leon AB, Liu JK, Wenokor C, Nimchinsky EA. Calvarial melorheostosis: An extremely rare case and diagnostic challenge. Skeletal Radiol 2025;54:1761-6. [Google Scholar | PubMed]
- 5.Mulliken JB, Young AE. Vascular Birth-Marks: Hemangiomas and Malformations. Philadelphia, PA: WB Saunders; 1988. [Google Scholar | PubMed]
- 6.Leri A, Joanny J. Une affection non décrite des os hyperostose “en coulée” sur toute la longeur d’un member ou “melorhéostose.” Bull Mem Soc Med Hosp Paris. 1922;46:1141–1145 [Google Scholar | PubMed]
- 7.Hellemans J, Preobrazhenska O, Willaert A, Debeer P, Verdonk PC, Costa T, et al. Loss-of-function mutations in LEMD3 result in osteopoikilosis, Buschke-Ollendorff syndrome and melorheostosis. Nat Genet 2004;36:1213-8. [Google Scholar | PubMed]
- 8.Chia KK, Haron J, Nik Malek NF. Atypical presentation of melorheostosis with soft tissues involvement: A case report. Egypt J Radiol Nuclear Med 2021;52:31. [Google Scholar | PubMed]
- 9.Mulligan ME. Classic Radiologic Signs: An Atlas and History. United States: CRC Press; 2020. [Google Scholar | PubMed]
- 10.Freyschmidt J. Melorheostosis: A review of 23 cases. Eur Radiol 2001;11:474-9. [Google Scholar | PubMed]










