The acromioclavicular cyst is a rare underdiagnosed presentation of a shoulder rotator cuff arthropathy with occasionally a normal functional shoulder.
Dr. Steve Fernandes, Department of Orthopaedics, SDM Medical College and Hospital, Dharwad, Karnataka, India. E-mail: steveferns661@gmail.com
Introduction: The acromioclavicular (AC) ganglion cyst first described by a shoulder arthrogram by Craig in 1984, still remains an uncommon presentation of a shoulder pathology. Classified as a type one cyst by Hiller in the presence of a rotator cuff pathology, the management of these lesions is governed by ill-defined guidelines. Literature shows the variability of surgical management ranges from simple cyst excision and lateral end clavicular excision to reverse shoulder arthroplasty. Type two cysts are usually benign ganglion cysts, filled with mucinous putty material, and arise from the AC joint as a result of constant pressure of the synovial fluid passing in sequence, from the glenohumeral joint to the subacromial bursa and then reaching the AC joint. They are painless, gradually enlarging masses that appear just at the tip of the shoulder and, unless large, do not limit shoulder movements.
Case Report: We present to you a 77-year-old male patient with hypertension and diabetes, who came with a painless swelling over the right shoulder, gradually increasing in size for the first 6 months. He gave a prior history of pain in the shoulder associated with stiffness, depicting a frozen shoulder 5 years ago. On examination, the swelling was soft, cystic, non-reducible, fluctuant, measuring 3 × 3 cm centred over the AC joint. The range of motion was near normal, comparable to the opposite side, associated with crepitus, although pain free. Clinical special tests revealed intact but weak cuff muscles. Imaging was performed that revealed superior migration of the humeral head and near complete chronic supraspinatus tear with glenohumeral arthritis on radiograph. Magnetic resonance imaging showed synovial thickening with a cystic homogenous swelling above the AC joint, a cutoff geyser sign with no communication to the AC joint or subacromial bursa. Complete excision of the cyst in toto was performed with no additional procedure. The histopathological examination revealed a ganglion cyst.
Conclusion: The AC joint cyst is a rare clinical diagnosis, requiring further insight into the spectrum of management of these lesions. In our case, the lack of clinical findings makes the management more challenging and thus, individualised.
Keywords: Acromioclavicular joint, rotator cuff, geyser sign, ganglion cyst.
The acromioclavicular (AC) ganglion cyst first described by a shoulder arthrogram by Craig in 1984, still remains an uncommon presentation of a shoulder pathology [1]. The cyst occurs in the subcutaneous plane of the superior aspect of the shoulder, commonly centred over the underlying AC joint. Classified by Hiller as type one when the pathology is within but only restricted to the AC joint and as type two when it is a manifestation of an underlying rotator cuff tear arthropathy [2]. The cyst progresses in size with time under a check valve mechanism; fluid enters under pressure during shoulder movement, and the valve closes [3]. Type one cysts, which are confined to the AC joint, present as cosmetic disturbances. These are treated by simple excision or arthroscopic debridement if symptomatic or develop secondary complications; rarely, a lateral end of clavicle excision is indicated. Type two cysts are more troublesome as the patient has a chronic cuff tear, principally the supraspinatus, that has retracted, leaving the humeral head to migrate proximally [4]. The geyser sign originally described by Craig [1] in an arthrogram and later extrapolated as a magnetic resonance imaging (MRI) finding, is the classic sign of a type two cyst [5]. The cyst occurring in this type of AC joint pathology can grow to a massive size with severe AC joint arthropathy and a complete rotator cuff tear [6]. The treatment of this type of cyst varies according to the patients presentation, age, and demand. Some authors have advocated simple cyst excision or excision of the lateral end of the clavicle when the functionality of the shoulder is preserved [7-9], and others have achieved good results with cyst excision followed by cuff repair [10] or reverse shoulder arthroplasty [11,12]. In consensus, the treatment of this lesion is primarily tailored to the patients requirements.
A 77-year-old male patient with right hand dominance, a known case of hypertension and diabetes, came to the outpatient department with a gradually increasing swelling over his right shoulder (Fig. 1) for the past 6 months. He was diagnosed with a frozen shoulder, having no history of trauma, 5 years ago, and recovered with a complete range of motion within a year. He gave a history of redeveloping shoulder pain 2 years ago, which disappeared within 6 months of onset. He had no limitations in his daily activities and continued to use his right hand with dominance. Sleeping on the right side was occasionally painful.
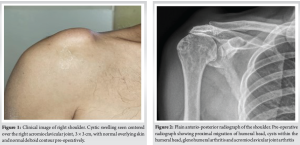
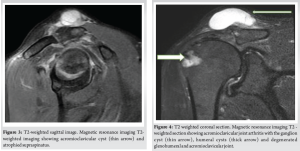
On examination, the shoulder swelling was globular, soft, cystic, fluctuant measuring 3 × 3 cm centered over the AC joint with the overlying skin stretched. There was no anterior joint tenderness or subacromial tenderness. The range of motion was comparable to the opposite side – forward flexion of 160°, abduction of 110° and near-normal internal and external rotations. The movements were associated with crepitus over the AC joint but no pain. Special tests revealed intact, but weak cuff muscles. Plain radiographs revealed superior migration of the humeral head, a sourcil sign of the greater tuberosity, glenohumeral and AC joint arthritis (Fig. 2). The MRI showed synovial thickening, degenerative changes in the AC joint and glenohumeral joint with a hyper-intense homogeneous cystic swelling above the AC joint on T2-weighted imaging (Fig. 3). There was a cut-off geyser sign with no communication to the AC joint or glenohumeral joint (Fig. 4). The supraspinatus was partially intact but atrophied. Considering the patients asymptomatic shoulder, wait and watch approach was considered for a period of 2 months for spontaneous regression. There was no subsidence in the size of the swelling and hence, the patient returned for removal of the lesion.
Under general anaesthesia, surgical resection of the cyst with fine dissection along the pseudo-capsule was performed and the cyst was removed in-toto (Fig. 5 and 6). The AC joint was visualised but not breached. The dead space was obliterated with absorbable sutures and wound closed; healing progressed normally. Histopathological examination revealed fibrocollagenous tissue with adipose tissue, congested blood vessels and histiocytes and overlying membranous mucin -– suggestive of a ganglion cyst. Cultures proved negative for tuberculosis and bacteria with no evidence of crystal disease. The patient was followed-up for a period of 6 months and had good functional recovery with no recurrence of the cyst.

An AC joint cyst is a rare presentation in the orthopaedic field. It is associated with or without an underlying rotator cuff tear and arthritis of the shoulder [2]. Type two cysts are far more common with a positive geyser sign present on MRI. Burns and Zvirbulis and Segmuller et al. were the first to report an AC joint cyst with a normal rotator cuff [13,14]. Several authors describe a symptomatic painful shoulder with a cyst that is gradually progressive in size. Occasionally the cyst may be tender, despite being non-infected or inflamed [3]. Aspiration of an asymptomatic cyst along with steroid injection has been associated with recurrences [15]. Spontaneous resolution of the cyst does occur, however, is unpredictable [16]. Some authors warrant a rotator cuff repair with arthroplasty as treatment of a functionally disabled shoulder in type two cysts [11]. In a rare case of repeated recurrences, despite aspiration and later, open debridement distal clavicle resection with cyst excision, the final resort was a reverse shoulder arthroplasty to gain symptom free shoulder movements [6]. In type one cysts, progressive degeneration of the AC joint due to trauma, infection, repeated overloading and metabolic disorders results in overproduction of synovial fluid and outpouching of the fluid through the superior surface of the joint bearing loose skin [17]. In type two cysts, a complete cuff tear is always present with retraction of the supraspinatus, this results in glenohumeral arthritis and proximal migration of the humeral head, displacing synovial fluid towards the AC joint. A subacromial spur may cause worsening of this process. With every movement of the shoulder, particularly above 45–70° in any plane, irritation of the inferior capsule of the AC joint ensues, degrading it and forcing fluid into the AC joint under pressure. This fluid passes across the joint to appear as a cyst superior to the joint. With progress of time the AC cyst may eventually get cut-off from the joint as an non-communicating independent cyst over the shoulder as seen on MRI [3]. In our case, we adopted a wait and watch policy to check for increasing size or any complications of the cyst. The MRI revealed a near complete cuff tear of the supraspinatus and no communication of the cyst with the glenohumeral joint. The humeral head had multiple cysts and degenerative changes of the glenohumeral and AC joint were plentiful. The patient did not have limitation of the shoulder function; the cuff was weak but did not cause disability to the patient. Aspiration of the cyst was abandoned for fear of creating a fistula tract in case of chronic tuberculosis infection. A mumford procedure consisting of excision of the distal clavicle has been performed by certain authors [18]. In an article by Purohit et al. with a geyser sign on MRI and normal shoulder function, cyst removal with distal clavicular excision and AC joint capsulorraphy was performed to prevent recurrence [8]. In our case, considering the good shoulder function, asymptomatic nature of the cyst and morbidity associated with clavicular excision, a simple cyst excision was performed. The histopathological examination of the biopsy were consistent with the contents of a ganglion cyst with mucinous material and focal myxoid degeneration encapsulated by fibrocollagenous tissue, similar to previous ganglion cysts [3].
We report an unusual presentation of a type two AC joint cyst where the patient had no limitation of the shoulder movements and minimal pain. The treatment was directed towards addressing the patient’s demand. When encountered, a chronic cuff tear should be the first suspicion in these lesions. We recommend an MRI for all cases of AC joint cyst, which will help us understand the underlying pathology, the cuff status and the arthritis. In certain cases it might be possible to differentiate a simple synovial cyst from cysts with crystals or infection, each of which have a different approach in management. If a wait and watch policy fails in mildly symptomatic patients, simple excision can be done without the complications of clavicular excision.
Clinical correlation with MRI imaging in a functionally normal shoulder with AC joint ganglion cyst is a must but can lead to over enthusiastic management of this condition. The treatment, though having variable guidelines must be individually tailored for best results.
References
- 1. Craig EV. The geyser sign and torn rotator cuff: Clinical significance and pathomechanics. Clin Orthop Relat Res 1984;191:213-5. [Google Scholar] [PubMed]
- 2. Hiller AD, Miller JD, Zeller JL. Acromioclavicular joint cyst formation. Clin Anat 2010;23:145-52. [Google Scholar] [PubMed]
- 3. Chaudhari T, Gupta A. Acromioclavicular ganglion cyst: A rare case report. Cureus 2024;16:e54089. [Google Scholar] [PubMed]
- 4. Neer CS 2nd, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg Am 1983;65:1232-44. [Google Scholar] [PubMed]
- 5. Cooper HJ, Milillo R, Klein DA, DiFelice GS. The MRI geyser sign: Acromioclavicular joint cysts in the setting of a chronic rotator cuff tear. Am J Orthop (Belle Mead NJ) 2011;40:E118-21. [Google Scholar] [PubMed]
- 6. Maris S, Tsiotsias A, Balfousias T, Angelis S, Kosmas L, Papatheodorou A, et al. An unusual presentation of a massive acromioclavicular joint ganglion cyst geyser sign secondary to massive rotator cuff tear and cuff arthropathy. J Long Term Eff Med Implants 2019;29:187-90. [Google Scholar] [PubMed]
- 7. De Maio F, Di Marcantonio A, De Luna V, Caterini A, Tresoldi I, Farsetti P. Synovial cyst of the acromioclavicular joint with and without rotator cuff tear: A case series of two patients. Int J Surg Case Rep 2020;75:390-3. [Google Scholar] [PubMed]
- 8. Purohit S, Keny S, Raja B, Marathe N. Massive acromio-clavicular joint ganglion cyst associated with cuff tear arthropathy and acromioclavicular joint arthritis with normal functional shoulder-a case report. J Clin Orthop Trauma 2019;10:522-5. [Google Scholar] [PubMed]
- 9. Christodoulou KC, Kakagia DD, Galanis VG, Tsoucalas GI, Fiska AT. Gigantic acromioclavicular joint cyst: Presentation and mini review. J Shoulder Elbow Surg 2021;30:e18-24. [Google Scholar] [PubMed]
- 10. Nowak DD, Covey AS, Grant RT, Bigliani LU. Massive acromioclavicular joint cyst. J Shoulder Elbow Surg 2009;18:e12-4. [Google Scholar] [PubMed]
- 11. Shaarani SR, Mullett H. Reverse total shoulder replacement with minimal ACJ excision arthroplasty for management of massive ACJ cyst – a case report. Open Orthop J 2014;8:298-301. [Google Scholar] [PubMed]
- 12. Emam M, Singhani N, Persaud C, Aibinder W. Fistula of acromioclavicular cyst treated with a staged reverse total shoulder arthroplasty: A case report. BMC Musculoskelet Disord 2022;23:1005. [Google Scholar] [PubMed]
- 13. Burns SJ, Zvirbulis RA. A ganglion arising over the acromioclavicular joint: A case report. Orthopedics 1984;7:1002-4. [Google Scholar] [PubMed]
- 14. Segmuller HE, Saies AD, Hayes MG. Ganglion of the acromioclavicular joint. J Shoulder Elbow Surg 1997;6:410-2. [Google Scholar] [PubMed]
- 15. Gumina S, Candela V, Passaretti D. Acromioclavicular joint cyst in ASA 3-4 patients. Whether and how quickly it recurs after aspiration and steroid injection. Acta Orthop Belg 2016;82:161-5. [Google Scholar] [PubMed]
- 16. De Hartog B, Schimmel JW, Rijk PC. Spontaneous disappearance of an acromioclavicular joint cyst: A case report. Am J Orthop (Belle Mead NJ) 2011;40:367-8. [Google Scholar] [PubMed]
- 17. Nardini C. Sul significato delle cisti acromio-clavicolari. loro associazone con la rottura della cuffia dei rotatori. Minerva Orthop 1991;42:211-6. [Google Scholar] [PubMed]
- 18. Mullett H, Benson R, Levy O. Arthroscopic treatment of a massive acromioclavicular joint cyst. Arthroscopy 2007;23:446.e1-4. [Google Scholar] [PubMed]