Early diagnosis and customized treatment planning are crucial even without accompanying ligamentous injuries. Recognizing this variation and using suitable surgical fixation through an anteromedial approach can yield good outcomes.
Dr. Ghadeer A Alsager, Department of Orthopedics, King Saud Medical City, Riyadh, Saudi Arabia. E-mail: ghadeer.alsagr@gmail.com
Introduction: Anteromedial tibial plateau fractures are an unusual pattern of injury, mostly caused by high-energy trauma in conjunction with knee hyperextension and varus force. This type of fracture is usually accompanied by extensive soft tissue injuries, especially the posterior cruciate ligament, the posterolateral corner, and, rarely, the medial meniscus.
Case Report: A 44-year-old medically free male sustained a hyperextension injury to his left knee after being kicked by a horse. Imaging showed an anteromedial tibial plateau rim fracture, as well as a fibular head fracture. Examination under anesthesia revealed a stable knee. Open reduction and internal fixation were conducted using a 3.5 locking compression plate L-shaped plate, and screws. Post-operative outcomes at 7 months of follow-up, the patients had complete knee mobility, no significant ligamentous damage, and returned to regular activities without discomfort.
Conclusion: This case illustrates that anteromedial tibial plateau fractures may occasionally occur without overt ligamentous injury. However, the absence of pre-operative magnetic resonance imaging and reliance on intraoperative manual testing limits the ability to exclude subclinical soft tissue damage. While stable fixation using an anteromedial approach resulted in favorable short-term outcomes, further studies and long-term follow-up are necessary to determine the durability of function and joint stability.
Keywords: Case report, tibia plateau, ligament injury, open reduction and internal fixation, Schatzker IV.
Anteromedial tibial plateau fractures are a rare fracture pattern that is mainly associated with high-energy trauma combined with knee hyperextension and varus stress [1]. This mechanism leads to compression force being transmitted between the medial femoral condyle and the anteromedial part of the tibial plateau, leading to either a small marginal fracture or a more severe depression at the articular surface [2]. Those fractures are usually marked by major soft tissue injuries, especially those of the posterior cruciate ligament (PCL), the posterolateral corner (PLC), and sometimes, the medial meniscus, as well as the bone damage[3]. Early and exact detection of such injuries is vital for both adequate diagnosis and surgical management [4]. Surgical treatment becomes necessary in circumstances when the injury encompasses a large anteromedial component. The ideal treatment in these situations is open reduction and internal fixation (ORIF) since it promotes proper anatomical alignment in addition to re-establishing mechanical stability and restoring joint congruency. Furthermore, it enables early mobilization [5]. The success of surgical treatment relies very much on choosing the appropriate surgical approach and repairing technique, which must be altered to match the morphology and location of the fracture [6]. For instance, the anteromedial approach provides direct and effective access to the fracture site when the fracture line runs along the anteromedial surface of the tibia [6]. Although more complicated fracture patterns may call for extra posterolateral or anterolateral incisions to provide sufficient exposure and reduction [6], this approach is usually used in solitary simple Schatzker type IV fractures. Herein, we report a case of anteromedial tibial plateau fracture treated with ORIF using an anteromedial method and an L-shaped locking compression plate (LCP) fixation. The purpose of this article is to report an unusual case of anteromedial tibial plateau fracture with arcuate fracture but with no significant ligament injury. We describe in detail the treatment and long-term follow-up for this uncommon subtype of fracture.
Initial patient assessment
We present a case of a 44-year-old male who has been medically free.
The patient presented to our facility after sustaining a hyperextension injury to the left knee by being kicked by a horse 1 day before presentation.
The patient presented with left knee pain and with inability to bear weight.
Presenting symptoms
Patient presented with left knee pain and with inability to bear weight.
Physical examination
Upon examination, the patient was hemodynamically stable, conscious, alert, and oriented. Local knee examination revealed a mild bruise over the anterior and medial surface of the knee, no open wounds, and moderate swelling. The patient’s compartments were soft and compressible, and distal neurovascular examination was intact. Tests for ligament stability were not conducted in the acute setting.
Diagnostic evaluation
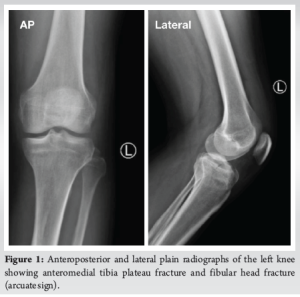
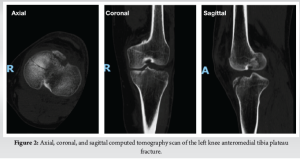
Imaging studies were done, including plain radiographs and computed tomography (CT), which revealed anteromedial rim fracture with anterior tibial eminence fracture of the left tibia and head of fibula fracture (arcuate sign) (Fig. 1 and 2). Although CT imaging provided adequate bony detail, no magnetic resonance imaging (MRI) was performed preoperatively to assess soft tissue structures. The presence of a fibular head fracture (arcuate sign), suggestive of possible PLC injury, was not explored further with advanced imaging due to financial considerations of the patient.
Initial therapeutic intervention
The patient consented to examination under anesthesia, along with ORIF of the left tibial plateau and possible ligament repair if indicated.
After swelling subsided, the patient was taken to the operating theater and, under spinal anesthesia, the patient was placed in the supine position and a left thigh tourniquet applied.
Examination under anesthesia or suspected ligament injury, including anterior and posterior drawer test, external rotation recurvatum, and tibial dial test, varus and valgus test were all negative, omitting the need for ligament repair.
Operative details
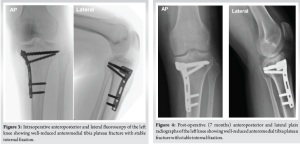
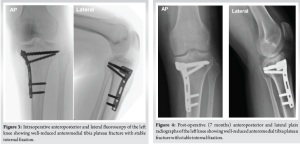
Prepping and draping were done in a sterile manner, and an anteromedial approach to the tibial plateau was used. Fracture exposed, and hematoma evacuated. There was an anteromedial plateau fracture, minimally displaced, and an anterior shell fracture not involving the articular surface. Under C-arm guidance, fracture reduction was done, and a 3.5 LCP L-shaped plate was placed on the anteromedial aspect. Three fully threaded cancellous screws were inserted proximally and 2 fully threaded locking screws were inserted in the shaft. Plate position was checked on anteroposterior and lateral C-arm views, which confirmed reduction and fixation. The anterior shell fracture was too small to be captured; thus, it was left intact (Fig. 3).
Then, the tourniquet was deflated. Hemostasis achieved. Closure is done in layers. Pressure dressing applied, and the patient placed on a knee immobilizer. The patient was shifted to the recovery room in a stable condition.
Postoperative course
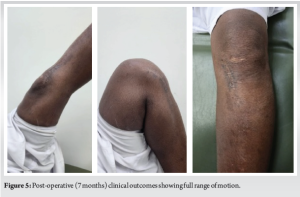
Postoperatively, the patient’s knee was immobilized in full extension using a hinged knee brace for the first 4 weeks to protect the fixation and facilitate early soft tissue healing. Passive range of motion (ROM) exercises was initiated at 4 weeks postoperatively, progressing to active-assisted and active ROM under supervised physiotherapy. Quadriceps strengthening and closed-chain exercises were gradually introduced between weeks 6 and 8. Partial weight bearing was permitted at 8 weeks, with progression to full weight bearing by 12 weeks, contingent upon radiographic evidence of healing. Throughout rehabilitation, emphasis was placed on joint stability, proprioceptive training, and return-to-function assessment tailored to the patient’s activity level. The patient was followed up in a 7-month period. In the last visit, the surgical scar was completely healed, the patient regained full knee ROM and was able to fully bear weight on it, and resumed his daily activities and job without complaining of pain. Patient was examined for ligamentous injuries which all were within normal range (Fig. 4 and 5).
A thorough understanding of the mechanism of injury of tibia plateau fractures can help in understanding fracture patterns, leading to an appropriate study and plan of the surgical treatment. Yang et al., study and analysis of type IV Schatzker fracture morphology divided type IV fractures further into three subtypes: Total medial plateau fracture, which accounted for 48%; posteromedial fracture, which accounted for 42.7%; and anteromedial fracture, which was the least common, accounting for only 9.3%. They emphasized the importance of distinguishing each type as it will affect surgical planning and thus patient outcome, for instance, medial buttress plating for posteromedial fractures has a high rate of fixation failure [7]. This classification scheme is also represented by the more comprehensive three-column theory, where this fracture pattern lies within the one-column “anteromedial” section [8,9]. The mechanism of the anteromedial column has been reported as hyperextension with varus injury [9]. All types of tibia plateau fractures have been associated with a potential ligamentous injury, and this fracture pattern is no exception [10]. The most commonly reported association with anteromedial tibial plateau fracture is concomitant PCL and PLC injuries [4,11]. Furthermore, reverse Segond fracture and anterior cruciate ligament (ACL) tibial avulsion fracture have been reported [1,2,12]. In a study of 353 tibial plateau fractures, anteromedial tibial plateau fractures were prevalent in 13.3% of which 51% had a fibular avulsion and 60% had posterior tension failure fragments [13]. In another study, 13.5% of anteromedial tibial plateau fractures had an arcuate sign [14]. It is also possible for this fracture pattern, to a lesser extent, to spare surrounding knee ligaments from injuries [11,12]. A correlation between fragment size and ligament injury has been suggested, whereas a small fragment – defined as less than a quarter of anteroposterior diameter of medial tibial plateau in CT-scan axial view – correlates with PCL injury followed by ACL injury and it also suggests an accompanying PLC injury, and when the fragment is large (more than a quarter), it can spare the PCL [15]. This was also confirmed in another recent study conducted in 2024 for patients with anteromedial tibial plateau fractures [16]. Fifty patients were subdivided into two groups: The first group (without fracture of the posterior column cortex) and the second group (with fracture of the posterior column cortex). The rate of PLC injuries was 28.6% in the first group without fracture of the posterior column cortex. Patients with PLC injuries showed fracture lines closer to the anterior rim of the medial plateau and had smaller fracture areas. Furthermore, 80% of the patients who had PLC injuries had associated PCL injuries[16]. A study by Li et al., 2019 defined a diagonal lesion, which is the combination of a triad of injuries: The PCL, PLC, and the anteromedial tibial plateau, and it was reported in their study with a 9.5%. They emphasized the importance of identifying these injuries as the failure of such can lead to residual instability and varus deformity [17]. Yoo et al., reported a missed case of PCL and posterolateral capsule disruption that was found on follow-up clinical visits after the patient had been treated conservatively. This was evident by patient complaints, physical examination, and confirmed by arthroscopic examination findings [18]. Another study reported a case of anteromedial tibial plateau injury, anterior depression of the articular surface accompanied by injury to the posterior ligament and tendon, and the popliteal artery. They treated the patient with ORIF with bone and symptomatic treatment of vascular injuries. However, ligament and tendon injuries have not been treated. The patient was followed up for 1 year and found that the fracture had healed, but the affected knee joint was unstable[19].
In terms of surgical treatment of this fracture pattern
As the fracture fragment is anteromedial, the usual choice to approach it is through an anteromedial approach, such as the one utilized in our case, and in the reported cases from the literature [4,19,20]. In regard to internal fixation, cannulated compression screws and a T-shaped or L-shaped pre-contoured plate acting as a buttress plate were reported and utilized in our case [4,19,20]. In this case, the anteromedial tibial plateau fracture involved a minimally displaced anterior rim fragment, without significant comminution or posterior column extension. Given this non-complex fracture morphology, the use of a 3.5 mm LCP L-shaped plate was deemed biomechanically appropriate. The L-shape configuration offered a direct buttress to the anteromedial cortex, aligning well with the trajectory of the fracture line. The fixed-angle locking construct provided reliable angular stability, which is particularly beneficial in countering anterior shear and varus forces – both of which are prominent in hyperextension – varus injury mechanisms typically associated with this fracture type. In addition, the plate’s low-profile design allowed for subpatellar application without interfering with soft tissue structures, particularly in the “bare area” under the patellar tendon. This eliminated the need for more invasive approaches or rim-specific plates, which are often necessary in comminuted or anteriorly displaced fractures. Radiographic follow-up confirmed maintenance of reduction and implant stability, supporting the construct’s adequacy for this specific injury pattern. However, the L-shaped plate does not offer dedicated anterior rim buttressing and may not optimally conform to the curvature of the “bare area” in cases with more anterior displacement or comminution. In such situations, rim-specific plates or supplementary fixation techniques may be biomechanically superior [4,19,20].
When PCL injury/or any ligament injury was encountered, it was addressed accordingly, but as our clinical examination led to a stable condition, such repair was not needed. Furthermore, if bone defects were found, they should be filled with artificial bone graft as reported; however, it was not needed in our case as well [4,19,20]. The challenge arises when a compression or a fragment is located anteriorly behind the patellar tendon, as it has a low range of mobility of the patellar tendon [20]. This challenge was addressed in another study a retrospective analysis of 13 patients with hyperextension tibial plateau fracture of which three were of anteromedial tibial plateau fractures were treated with using anteromedial approach, they labeled the fractured most anterior part of rim area as the “bare area” and the specific reason they addressed this areas as it was challenging for fixation due to the shelter of the patella tendon and limited space for plate placement. To address this issue, they developed the 2.7 mm pre-contoured rim plate to buttress the anterior plateau [21]. In this case, the anterior rim fragment was minimally displaced, non-comminuted, and accessible through the anteromedial approach. The fragment did not lie entirely within the “bare area” beneath the patellar tendon, and the morphology allowed secure capture through the trajectory of the proximal screws of the 3.5 mm LCP L-shaped plate. Given these favorable characteristics and the absence of mechanical impingement or soft tissue obstruction, a dedicated anterior rim plate was deemed unnecessary. In addition, the rim fragment was too small for independent screw purchase, and the construct achieved intraoperative stability without supplemental anterior buttressing. Use of a rim-specific plate, while beneficial in larger or more anteriorly positioned fragments, was not justified based on the fracture configuration, displacement, and stable fixation obtained intraoperatively. All the above studies reported satisfactory clinical and radiographic outcomes [4,20], apart from Li, Kai, as they failed to address the ligamentous injury [19]. When knee instability and significant ligamentous injury are encountered, they must be addressed either open or arthroscopically [22]. Details from the literature in regard to ligamentous treatment were not studied thoroughly in this article, as it was not encountered in our case and was not of major concern.
The presented case supports the possibility that anteromedial tibial plateau fractures may present without clinically evident ligament injury and be managed effectively with ORIF through an anteromedial approach. While stable fixation using an LCP fixation resulted in favorable short-term outcomes. However, diagnostic limitations, particularly the absence of MRI, short follow-up duration, limit the strength of this conclusion. Future cases should emphasize comprehensive preoperative imaging, long-term functional assessment, and biomechanical evaluation of fixation constructs.
Limitation
This study presents a single case, inherently limiting the applicability of its conclusions to the broader patient population. Individual variation in anatomy, mechanism of injury, and response to treatment makes extrapolation unreliable. No statistical analysis or comparative evaluation was possible. The initial ligament evaluation was not performed in the acute setting due to swelling and pain. There was no pre-operative MRI to assess soft tissue injuries objectively; reliance was on intraoperative manual testing under anesthesia. This raises the possibility that subclinical or partial ligament injuries might have been missed. MRI, which is the gold standard for evaluating ligament and meniscal integrity, was not utilized. Follow-up was limited to 7 months, which is insufficient. There is no use of standardized outcome measures.
Although usually connected with ligamentous injuries, anteromedial tibial plateau fractures can also occur in isolation. Accurate diagnosis, thorough pre-operative evaluation, and early surgical intervention employing an anteromedial method with stable internal fixation can produce great results. Identification of this uncommon pattern and knowledge of its distinct features are critical to avoid missed injuries and guarantee joint stability even without ligamentous involvement.
References
- 1. Chanasit P, Sa-Ngasoongsong P, Chanplakorn P, Jaovisidha S, Suphachatwong C, Wajanavisit W. Anteromedial marginal fracture of medial tibial plateau without significant knee ligamentous injury in hypermobility patient: A case report and review of literature. Orthop Rev (Pavia) 2013;5:56-8. [Google Scholar] [PubMed]
- 2. Chiba T, Sugita T, Onuma M, Kawamata T, Umehara J. Injuries to the posterolateral aspect of the knee accompanied by compression fracture of the anterior part of the medial tibial plateau. Arthroscopy 2001;17:642-7. [Google Scholar] [PubMed]
- 3. Cohen AP, King D, Gibbon AJ. Impingement fracture of the anteromedial tibial margin: A radiographic sign of combined posterolateral complex and posterior cruciate ligament disruption. Skeletal Radiol 2001;30:114-6. [Google Scholar] [PubMed]
- 4. Conesa X, Minguell J, Cortina J, Castellet E, Carrera L, Nardi J, et.al. Fracture of the anteromedial tibial plateau associated with posterolateral complex injury: Case study and literature review. J Knee Surg 2013;26 Suppl 1:S34-9. [Google Scholar] [PubMed]
- 5. Chellamuthu G, Chandramohan AK, Zackariya M, Perumal R, Jayaramaraju D, Shanmuganathan R. Uncommon pattern of anterior compression fractures of the tibial plateau: A report of 7 cases and review of literature. J Orthop Case Rep 2021;11:39-46. [Google Scholar] [PubMed]
- 6. Kandemir U, Maclean J. Surgical approaches for tibial plateau fractures. J Knee Surg 2014;27:21-9. [Google Scholar] [PubMed]
- 7. Yang G, Zhu Y, Luo C, Putnis S. Morphological characteristics of Schatzker type IV tibial plateau fractures: A computer tomography based study. Int Orthop 2012;36:2355-60. [Google Scholar] [PubMed]
- 8. Shetty V, Shekhar S, Wagh Y. Tibial condyle fractures: Current concepts of internal fixation. J Clin Orthop 2021;6:32-44. [Google Scholar] [PubMed]
- 9. Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma 2010;24:683-92. [Google Scholar] [PubMed]
- 10. Malik S, Herron T, Mabrouk A, Rosenberg NE. Tibial plateau fractures. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470593 [Last accessed on 2023 Apr 22]. [Google Scholar] [PubMed]
- 11. Bedeir YH. Reverse segond fracture associated with anteromedial tibial rim and tibial attachment of anterior cruciate ligament avulsion fractures. Case Rep Orthop 2017;2017:9637153. [Google Scholar] [PubMed]
- 12. Bennett DL, George MJ, El-Khoury GY, Stanley MD, Sundaram M. Anterior rim tibial plateau fractures and posterolateral corner knee injury. Emerg Radiol 2003;10:76-83. [Google Scholar] [PubMed]
- 13. Xie X, Zhan Y, Wang Y, Lucas JF, Zhang Y, Luo C. Comparative analysis of mechanism-associated 3-dimensional tibial plateau fracture patterns. J Bone Joint Surg Am 2020;102:410-8. [Google Scholar] [PubMed]
- 14. Zhang X, Tian X, Wang S, Hu Y, Pan S, Peng A. Different patterns of tibial plateau fractures associated with hyperextension injuries of the knee with or without varus/valgus component. Medicine (Baltimore) 2021;100:e28337. [Google Scholar] [PubMed]
- 15. Tomás-Hernández J, Monyart JM, Serra JT, Vinaixa MR, Farfan EG, García VM, et al. Large fracture of the anteromedial tibial plateau with isolated posterolateral knee corner injury: Case series of an often missed unusual injury pattern. Injury 2016;47 Suppl 3:S35-40. [Google Scholar] [PubMed]
- 16. Wang B, Ye T, Zhang B, Wang Y, Zhu Y, Luo C. Relationship of fracture morphological characteristics with posterolateral corner injuries in hyperextension varus tibial plateau fractures. J Bone Joint Surg Am 2024;106:2001-8. [Google Scholar] [PubMed]
- 17. Li X, Song G, Li Y, Liu X, Zhang H, Feng H. The “diagonal” lesion: A new type of combined injury pattern involving the impingement fracture of anteromedial tibial plateau and the injury of posterior cruciate ligament and posterolateral corner. J Knee Surg 2020;33:616-22. [Google Scholar] [PubMed]
- 18. Yoo JH, Kim EH, Yim SJ, Lee BI. A case of compression fracture of medial tibial plateau and medial femoral condyle combined with posterior cruciate ligament and posterolateral corner injury. Knee 2009;16:83-6. [Google Scholar] [PubMed]
- 19. Li K, Chen J, Liu Z, Li X, Wang J. Hyperextension type tibial plateau fracture: A case study and literature review. Open J Clin Med Images 2022;2:1025. [Google Scholar] [PubMed]
- 20. Liu ZY, Zhang JL, Liu C, Cao Q, Shen QJ, Zhao JC. Surgical strategy for anterior tibial plateau fractures in hyperextension knee injuries. Orthop Surg 2021;13:966-78. [Google Scholar] [PubMed]
- 21. Sun Z, Li T, Liu Y, Mao Y, Li W, Guo Q, et al. Rim plate in the treatment of hyperextension tibial plateau fracture: Surgical technique and a series of cases. BMC Musculoskelet Disord 2023;24:655. [Google Scholar] [PubMed]
- 22. Li L, Li Y, He Y, Deng X, Zhou P, Li J, et.al. Single-stage arthroscopic-assisted treatment of anteromedial tibial plateau fracture with posterolateral corner injury: A retrospective study. BMC Musculoskelet Disord 2022;23:420. [Google Scholar] [PubMed]