Chronic patellar dislocation with femoral dysplasia and dynamic patellar maltracking.
Dr. Florent Francony, Department of Orthopedic and Trauma Surgery, CH Métropole Savoie, Place Lucien Biset - P.O. Box 31125, 73011 Chambéry Cedex, France. E-mail: dr.francony@gmail.com
Introduction: Chronic patellar dislocation during flexion is a rare condition associated with femoral dysplasia and dynamic patellar maltracking. The presence of an anterior femoral bump contributes to the mechanical conflict.
Case Report: We report the case of a young adult with chronic patellar dislocation during knee flexion, associated with patellofemoral dysplasia, anterior bump, and lateral laxity.
Conclusion: Treatment consisted of a distal femoral anterior subtraction osteotomy combined with medial patellofemoral ligament reconstruction. Pre- and post-operative documentation as well as imaging demonstrate the correction of the instability.
Keywords: Medial patellofemoral ligament reconstruction, patellar dislocation, trochlear dysplasia, trochleoplasty.
Chronic lateral dislocation of the patella occurring primarily during knee flexion is rare and frequently underdiagnosed. It is often linked to trochlear dysplasia and, in some cases, to a prominent anterior femoral bump that disrupts patellar engagement during flexion [1]. In such cases, static soft tissue restraints, particularly the medial patellofemoral ligament (MPFL), may be insufficient or stretched [2]. This case demonstrates the successful treatment of such a complex instability using a combined bony and soft tissue approach: distal femoral anterior subtraction osteotomy per Pujol’s technique [1] and MPFL reconstruction.
A 43-year-old woman originally from Ukraine presented with chronic instability from child of the right patella during flexion at 70°. No prior trauma or surgery was reported. The dislocation was reproducible during squatting or climbing stairs, without instability in extension.
Clinical findings:
- Positive J-sign
- Patella stable in extension, lateral dislocation at 60–90° flexion
- Positive Smillie test, with increased lateral translation in flexion
- Mild quadriceps atrophy, no hyperlaxity elsewhere
- Kujala score 55
- IKDC score 32
- KOOS score 55.
Imaging:
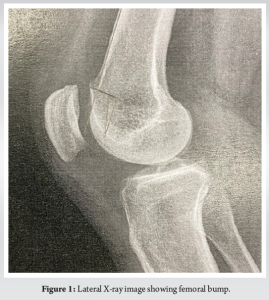
- X-ray (Fig. 1), computed tomography (Fig. 2) and magnetic resonance imaging showed Dejour type D trochlear dysplasia
- Anterior femoral bump visible in lateral view (9 mm)
- TT-TG: 11 mm
- Normal femoral version and tibial torsion.

Surgical technique
The patient underwent combined bony and soft tissue surgery:
- Distal femoral anterior closing-wedge osteotomy (Fig. 3)

- Via medial parapatellar approach
- Marking the osteotomies on the bone with a dermographic pen, according to the pre-operative planning
- Performing the anteroposterior cut first using a reciprocal saw
- Making the posterior cut, strictly parallel to the frontal plane of the femur:
Note: The cut is stopped approximately 5 mm from the sulcus terminalis to preserve the distal osteochondral hinge.
- Performing the anterior slanting cut to connect the two previous cuts
- Removing the bone wedge (proximally based)
- Progressive closure of the osteotomy by applying digital pressure on the trochlea
- Fixation of the osteotomy using 3.5 mm cancellous screws
Note: Positioned just laterally to the cartilage surface.
- MPFL reconstruction (Fig. 4)

- Autologous gracilis graft harvested
- Femoral tunnel positioned under fluoroscopic control at Schöttle’s point
- Patellar insertion through two anchors
- Tensioning at 30° of flexion to avoid overtightening
- Femoral fixation with screw.
Post-operative protocol:
- Knee brace in extension for 3 weeks
- Passive flexion from day 1 up to 90°
- Partial weight bearing at 3 weeks
- Active rehab with closed-chain strengthening at 6 weeks.
Outcomes
At 6 months:
- No episodes of dislocation or subluxation
- ROM: 0–130°, symmetrical with contralateral knee
- Kujala score improved from 58 to 87
- IKDC score improved from 32 to 82
- KOOS score improved from 55 to 85
- Clinical patellar tracking was centered throughout the range of motion
- Patella remained stable under manual testing (negative Smillie and J-sign)
- Radiographs showed complete bone healing and restored slope (Fig. 5).

Chronic patellar dislocation during flexion without prior trauma is often misdiagnosed. The failure of patellar engagement with the trochlea during flexion may be due to both soft tissue and bony anomalies. The femoral bump, described by Pujol and Beaufils [1], is an anterior overgrowth of the distal femur, which impairs patellar glide and promotes lateral dislocation under flexion stresses. While MPFL reconstruction is commonly used to address recurrent patellar instability [2,3], its isolated use in cases with bony deformity can lead to recurrence or graft overload [4]. Thus, an osteotomy that corrects the anatomical abnormality, in this case via anterior subtraction, is justified. Previous work by Dejour et al. [5] has shown that patellofemoral instability is multifactorial, often requiring combined surgical techniques. Our patient presented with a positive Smillie test and demonstrated a femoral bump on CT imaging, with no rotational malalignment. The use of distal femoral osteotomy to remove the bump corrected the bony conflict and restored patellar tracking. The addition of MPFL reconstruction further enhanced medial stability, particularly in the early post-operative period. Biomechanical studies have confirmed that the MPFL contributes to 50–60% of medial restraint during early flexion [6,7]. Positioning the femoral tunnel correctly at Schöttle’s point is critical to avoid overtensioning or failure [8]. Other studies have described similar combined approaches with encouraging outcomes. Wagner et al. [9] noted improved tracking with dual interventions in patients with complex trochlear or femoral morphology. Long-term results are encouraging, but careful patient selection and anatomical analysis remain essential [10].
Combined trochleoplasty and MPFL reconstruction is a useful and reliable surgical technique to improve patellofemoral stability in patients with trochlear dysplasia.
Chronic patellar dislocation during knee flexion is a rare condition, often associated with femoral dysplasia and dynamic patellar maltracking. A thorough understanding of the underlying pathology and the available treatment options is essential for effective management.
References
- 1. Pujol N, Beaufils P. Osteotomy of the distal femur for flexion patellar instability: A novel concept. Orthop Traumatol Surg Res 2020;106:1603-6. [Google Scholar] [PubMed]
- 2. Schöttle PB, Fucentese SF, Romero J. Clinical and radiological parameters for patellar instability. Knee Surg Sports Traumatol Arthrosc 2008;16:1045-51. [Google Scholar] [PubMed]
- 3. Philippot R, Boyer B, Testa R, Farizon F. The medial patellofemoral ligament: Anatomy, biomechanics and treatment. Orthop Traumatol Surg Res 2009;95 8 Suppl 1:S60-7. [Google Scholar] [PubMed]
- 4. Stephen JM, Kader D, Lumpaopong P, Deehan DJ, Amis AA. The effects of medial patellofemoral ligament reconstruction on patellar tracking and patellofemoral joint contact pressures. Am J Sports Med 2011;39:181-8. [Google Scholar] [PubMed]
- 5. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: An anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 1994;2:19-26. [Google Scholar] [PubMed]
- 6. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 1998;26:59-65. [Google Scholar] [PubMed]
- 7. Conlan T, Garth WP Jr., Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 1993;75:682-93. [Google Scholar] [PubMed]
- 8. Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007 May;35(5):801-4. doi: 10.1177/0363546506296415. Epub 2007 Jan 31. PMID: 17267773. [Google Scholar] [PubMed] [CrossRef]
- 9. Wagner D, Pfalzer F, Hingelbaum S, Distal femoral osteotomy for treatment of patellofemoral instability. Int Orthop 2016;40:1881-7. [Google Scholar] [PubMed]
- 10. Ren B, Zhang X, Zhang L, Zhang M, Liu Y, Tian B, et al. Isolated trochleoplasty for recurrent patellar dislocation has lower outcome and higher residual instability compared with combined MPFL and trochleoplasty: A systematic review. Arch Orthop Trauma Surg 2019;139:1617-24. [Google Scholar] [PubMed]








