A combined physiotherapeutic approach involving muscle energy technique (MET), strengthening exercises, and patellar mobilization significantly improves pain, function, and mobility in patients with patellofemoral osteoarthritis.
Miss. Namrata Srivastava,Department of Physiotherapy, NIMS University, Jaipur, Rajasthan, India. E-mail: nam.fdi@gmail.com
Introduction: Patellofemoral osteoarthritis (PFOA) is a prevalent degenerative joint disorder characterized by anterior knee pain, stiffness, reduced functional mobility, and impaired quality of life, particularly in older adults. Due to its multifactorial etiology—including muscle imbalance, altered patellar tracking, and joint degeneration—conservative physiotherapy approaches are often prioritized over surgical interventions. This study aimed to evaluate the clinical effectiveness of an integrated physiotherapeutic regimen comprising muscle energy technique (MET), targeted strengthening exercises, and patellar mobilization in the management of PFOA. These findings support the inclusion of multimodal manual therapy and targeted exercise interventions as first-line conservative management strategies for patellofemoral joint degeneration. However, due to the small sample size, further large-scale studies are warranted to enhance generalizability and confirm these results.
Materials and Methods: A single-group pre- and post-interventional design was implemented involving 30 participants (aged 45–65 years) clinically and radiologically diagnosed with PFOA. The 6-week intervention protocol included MET applied to the quadriceps and hamstring muscle groups, progressive resistance strengthening exercises focusing primarily on the vastus medialis obliquus (VMO), and patellar mobilization techniques aimed at improving patellar tracking and joint mobility. Each participant received three supervised sessions per week. Outcome measures were assessed at baseline and post-intervention using the Visual Analog Scale (VAS) for pain intensity, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) for pain, stiffness, and functional limitation, and the Kujala Anterior Knee Pain Scale for patellofemoral joint function.
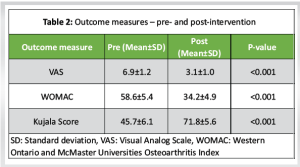
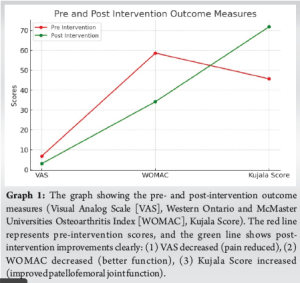
Results: Statistical analysis revealed significant improvements across all outcome parameters post-intervention. Mean VAS scores decreased from 6.9 ± 1.2 to 3.1 ± 1.0 (P < 0.001), indicating substantial pain relief. WOMAC scores showed a marked reduction from 58.6 ± 5.4 to 34.2 ± 4.9 (p < 0.001), reflecting improved joint function and reduced stiffness. The Kujala Score improved significantly from 45.7 ± 6.1 to 71.8 ± 5.6 (P < 0.001), denoting enhanced patellofemoral mechanics and functional mobility.
Conclusion: The study demonstrates that a physiotherapy program integrating MET, quadriceps strengthening (with VMO emphasis), and patellar mobilization is effective in significantly reducing pain and improving functional outcomes in individuals with PFOA. These findings support the inclusion of multimodal manual therapy and targeted exercise interventions as first-line conservative management strategies for patellofemoral joint degeneration. However, due to the small sample size, further large-scale studies are warranted to enhance generalizability and confirm these results.
Keywords: Patellofemoral osteoarthritis, muscle energy technique, quadriceps strengthening, patellar mobilization, physiotherapy intervention, joint function.
Patellofemoral osteoarthritis (PFOA) is a specific subset of knee osteoarthritis characterized by degenerative changes primarily affecting the articular cartilage of the patella and the trochlear groove of the femur. It is a major contributor to anterior knee pain, particularly in elderly and postmenopausal women, though it also affects younger individuals with predisposing biomechanical factors. Clinical manifestations typically include anterior or retropatellar knee pain, crepitus, joint stiffness, swelling, and difficulty in performing activities involving knee flexion, such as squatting, stair climbing, or prolonged sitting [1,2]. As the global population ages, the prevalence of PFOA is expected to rise, increasing the burden on health-care systems and necessitating cost-effective, conservative management strategies [3]. The etiology of PFOA is multifactorial and often involves a complex interplay of biomechanical, anatomical, and neuromuscular factors. Muscle imbalances, particularly weakness of the quadriceps and hip abductors, and tightness in the hamstrings or iliotibial band, can disrupt patellofemoral joint biomechanics, leading to abnormal joint stress and cartilage degeneration [4,5]. Patellar maltracking due to soft-tissue tightness or motor control deficits further contributes to accelerated wear of the joint surfaces, worsening the condition over time [6]. Pharmacological treatments such as non-steroidal anti-inflammatory drugs and analgesics are commonly used to provide symptom relief; however, they do not address underlying mechanical dysfunctions and carry potential side effects with long-term use [7]. Consequently, conservative physiotherapeutic interventions have become the mainstay of PFOA management, focusing on restoring joint mechanics, reducing pain, and improving functional capacity [8,9]. One such intervention is the muscle energy technique (MET), a form of manual therapy that uses voluntary isometric contractions of muscles against a controlled resistance to improve joint mobility and lengthen shortened or spastic muscles. MET is particularly effective in treating soft-tissue restrictions, improving flexibility, and enhancing proprioception without stressing degenerated joint structures [10,11]. Its application to the hamstrings and quadriceps is beneficial in restoring muscle balance around the knee joint in PFOA patients [12]. Strengthening exercises, especially those targeting the vastus medialis obliquus (VMO), play a crucial role in patellar stabilization. Weakness of the VMO relative to the vastus lateralis can cause lateral patellar tracking and increased patellofemoral joint stress. Focused VMO strengthening improves patellar alignment, enhances knee stability, and reduces pain [13,14]. Resistance-based closed kinetic chain exercises, such as mini-squats and step-downs, have shown significant benefits in improving lower limb function in individuals with patellofemoral dysfunction [15]. Patellar mobilization, another frequently employed manual therapy technique, involves passive gliding of the patella to improve mobility, reduce capsular stiffness, and restore optimal joint kinematics. Mobilization of the patella in the medial, lateral, superior, and inferior directions aids in correcting maltracking and improving synovial fluid distribution, which is essential for cartilage health [16,17]. Evidence suggests that patellar mobilization can significantly reduce anterior knee pain and facilitate improved function in patients with PFOA [18].
Despite the individual benefits of these interventions, limited studies have explored their combined effectiveness as a multimodal therapeutic protocol. Most clinical trials have investigated either strengthening or manual therapy in isolation, which may not reflect the complex interplay of impairments seen in PFOA patients [19]. A combination of MET, muscle strengthening, and patellar mobilization may yield synergistic effects by simultaneously addressing soft tissue flexibility, muscle strength, and joint mobility—key elements in the conservative treatment of this condition [20]. Therefore, the present study aims to evaluate the effectiveness of a physiotherapy program combining MET, quadriceps strengthening with VMO emphasis, and patellar mobilization in reducing pain, improving function, and enhancing patellofemoral joint mechanics in individuals diagnosed with PFOA. By employing validated outcome tools such as the Visual Analog Scale (VAS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and Kujala Anterior Knee Pain Scale, this research seeks to provide evidence for a comprehensive, conservative physiotherapeutic protocol tailored to address the multifactorial nature of PFOA.
The research proposal has been approved by the Institutional Ethics Committee under IEC No. Ref: NIMS/PTOT/Ethical/2024/09(i), dated 23.12.2024.
Study design
Pre–post-interventional study.
Participants
Thirty subjects (aged 45–65 years) with clinically diagnosed PFOA.
Inclusion criteria
- Anterior knee pain ≥3 months
- Radiographic evidence of PFOA (Kellgren–Lawrence grade I–II)
- VAS score ≥4.
Exclusion criteria
- History of knee surgery
- Systemic inflammatory joint disease
- Acute knee injury.
Intervention protocol (6 weeks)
- MET: Post-isometric relaxation for hamstrings and quadriceps (3 reps × 30 sec hold)
- Strengthening: VMO-focused isometric and isotonic quadriceps strengthening (progressive resistance)
- Patellar mobilization: Medial and inferior glides (3 sets × 30 s).
Frequency
Three sessions/week.
Outcome measures
- VAS
- WOMAC
- Kujala Anterior Knee Pain Scale.
Statistical analysis
The paired t-test is a statistical method used to compare the means of two related measurements taken from the same group, typically before and after an intervention. It evaluates whether the average difference between paired observations is statistically significant, thus determining the effectiveness of a treatment or intervention. This test is ideal for within-subject study designs, such as the present study, where pre- and post-intervention scores (VAS, WOMAC, and Kujala) were collected from the same participants. Using each subject as their own control, the paired t-test minimizes variability and enhances statistical power. It assumes that the differences between the paired scores are normally distributed and measured on an interval or ratio scale. In this study, the paired t-test was used to assess the impact of a 6-week physiotherapy intervention combining MET, strengthening, and patellar mobilization, with a significance level set at P < 0.05. A statistically significant result indicates that the observed improvements are unlikely due to chance and can be attributed to the intervention.
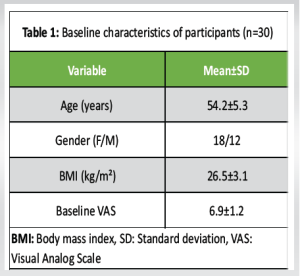
The results of this study demonstrate statistically significant improvements in all measured outcomes following the 6-week physiotherapy intervention combining MET, strengthening exercises, and patellar mobilization. The baseline characteristics show a middle-aged cohort with a moderate body mass index (BMI) and moderate pain levels, as indicated by the initial VAS score. Post-intervention analysis revealed a marked reduction in pain intensity (VAS), with scores significantly decreasing from 6.9 to 3.1, indicating effective pain relief. Functional ability, assessed by the WOMAC index, improved substantially, reflecting reduced joint stiffness and enhanced physical function. In addition, the Kujala score, which evaluates patellofemoral joint function and anterior knee pain, showed significant enhancement, suggesting better joint mechanics and mobility. The highly significant P-values (<0.001) across all outcomes confirm that these improvements are unlikely due to chance and support the effectiveness of the integrated physiotherapeutic approach in managing PFOA (Tables 1 and 2, Graph 1).
The present study demonstrated that an integrated physiotherapy program combining MET, targeted strengthening exercises focusing on the VMO, and patellar mobilization produced significant clinical improvements in pain, function, and patellofemoral joint mechanics among patients with PFOA. The findings highlight the multifaceted benefits of this multimodal approach, supporting its use as a conservative management strategy for PFOA.
MET likely contributed to clinical improvements by reducing muscle tightness and improving soft-tissue extensibility around the knee joint, particularly in the quadriceps and hamstrings. Muscle tightness and imbalance are known contributors to abnormal patellar tracking and joint stress, accelerating cartilage degeneration [1]. By employing controlled isometric contractions and relaxation, MET helps restore optimal muscle length and tension balance, which in turn enhances patellar alignment and increases joint mobility. This restoration of flexibility may reduce abnormal loading on the patellofemoral joint surfaces and contribute to pain relief. Targeted strengthening of the VMO is critical for dynamic stabilization of the patella. Weakness or delayed activation of the VMO relative to the vastus lateralis is implicated in lateral patellar maltracking and increased joint stress [2]. By strengthening the VMO, this intervention improves medial patellar pull and stabilizes the patella during knee movements, thereby reducing joint load and mitigating pain. Previous studies have underscored the importance of quadriceps strengthening in improving functional outcomes and reducing symptoms in PFOA [3,4]. The current results reinforce the role of muscle strengthening, specifically VMO activation, in restoring biomechanical integrity and improving patient-reported outcomes. Patellar mobilization likely enhanced synovial fluid distribution within the joint, promoting cartilage nutrition and reducing stiffness. Adequate cartilage nutrition and lubrication are essential for joint health, particularly in degenerative conditions like osteoarthritis, where cartilage breakdown is prevalent⁵. Mobilization also aids in correcting patellar malalignment by improving soft-tissue compliance and joint capsule mobility, which facilitates smoother joint mechanics during movement. This manual therapy technique has been shown to decrease pain and improve mobility in individuals with patellofemoral pain syndrome and osteoarthritis [6]. The significant improvements observed across the VAS, WOMAC, and Kujala Anterior Knee Pain Scale align with prior research emphasizing the combined importance of muscle flexibility, strength, and joint mobility in managing PFOA. For instance, Aminaka and Gribble, and Powers demonstrated that MET combined with quadriceps strengthening improved knee mechanics and reduced pain, highlighting the potential synergistic effect of these modalities when used together. Similarly, other studies have reported that manual therapy paired with exercise therapy produces superior outcomes compared to exercise alone [7,8]. This study’s findings also support the biopsychosocial model of osteoarthritis management, which advocates for multimodal interventions addressing not only pain but also functional limitations and biomechanical impairments [9]. By targeting different aspects of joint pathology – muscle tightness, weakness, and joint stiffness – the combined intervention offers a comprehensive approach that may yield longer-lasting benefits than unimodal treatments.
However, some limitations should be considered. The sample size was relatively small, and the absence of a control group limits the ability to generalize results broadly. Future randomized controlled trials with larger cohorts and longer follow-up periods are warranted to confirm these findings and explore the durability of clinical improvements. In addition, incorporating objective biomechanical assessments, such as gait analysis or imaging studies, could further elucidate the mechanisms underlying functional gains. In conclusion, the integration of MET, VMO strengthening, and patellar mobilization is an effective conservative treatment strategy for patients with PFOA, significantly reducing pain and enhancing joint function. This multimodal physiotherapy approach should be considered in clinical practice to improve the quality of life and functional independence in individuals suffering from PFOA. Despite the positive outcomes observed, the relatively small sample size (n = 30) presents a significant limitation. It reduces the statistical power of the study, potentially increasing the risk of Type II error – where small but clinically meaningful differences may go undetected. Furthermore, the limited cohort size restricts the ability to conduct subgroup analyses based on age, sex, or BMI, which are known to influence treatment response in PFOA. These factors should be addressed in future studies through larger, more diverse participant samples.
Despite the positive outcomes observed, the relatively small sample size (n = 30) presents a significant limitation. It reduces the statistical power of the study, potentially increasing the risk of Type II error – where small but clinically meaningful differences may go undetected. Furthermore, the limited cohort size restricts the ability to conduct subgroup analyses based on age, sex, or BMI, which are known to influence treatment response in PFOA. These factors should be addressed in future studies through larger, more diverse participant samples. This study supports the effectiveness of a multimodal physiotherapy approach incorporating MET, strengthening, and patellar mobilization in alleviating symptoms of PFOA. The protocol offers a cost-effective, non-invasive strategy that can be adopted in routine clinical practice for improved patient outcomes.
Small sample size
The study included only 30 participants, which limits statistical power and may not adequately represent the broader population of individuals with PFOA. A small cohort increases the risk of Type II error, meaning that subtle but clinically important treatment effects may go undetected. In addition, the sample size restricted subgroup analysis (e.g., age, sex, and BMI) could have offered valuable insights into population-specific outcomes.
No long-term follow-up
The study evaluated short-term outcomes over 6 weeks, and the durability of clinical improvements remains unknown without extended follow-up.
Absence of a control group
The lack of a comparative or placebo group limits the ability to isolate treatment effects from potential placebo responses or natural fluctuations in symptom severity.
Potential measurement bias
All outcome measures used in this study – VAS, WOMAC, and Kujala Score – are subjective and patient-reported. Although validated and widely accepted in clinical research, they are prone to reporting bias, placebo effects, and daily symptom variability. The absence of objective functional assessments (e.g., gait analysis, isokinetic strength testing, or joint kinematics) limits the ability to triangulate and validate the subjective improvements.
Single-center study
The research was conducted at a single institution, which may limit the generalizability of findings to other clinical settings or more diverse populations. Differences in therapist expertise, patient demographics, and treatment environments could affect outcomes in real-world applications.
Lack of blinding
Neither participants nor outcome assessors were blinded to the intervention, introducing potential performance and detection biases. Awareness of receiving an active, specialized intervention may have positively influenced participants’ self-reporting, while unblinded evaluators may have been subconsciously biased during data collection.
Intervention heterogeneity and interaction effects
The study utilized a multimodal protocol combining MET, VMO-focused strengthening, and patellar mobilization. However, the individual contribution of each component was not assessed. Without a comparative or factorial design, it remains unclear whether the benefits resulted from one intervention alone or from a synergistic interaction among all three.
No adherence or compliance monitoring
The study did not report on participant adherence to prescribed home exercises or attendance at supervised sessions. Without tracking compliance, it is difficult to establish a dose–response relationship or determine whether treatment outcomes were influenced by engagement variability.
Selection bias
Participants were included based on clinical diagnosis and willingness to undergo physiotherapy, potentially introducing a selection bias favoring more motivated or physically capable individuals. This may overestimate the effectiveness of the intervention and limit applicability to frailer or more sedentary populations.
Absence of imaging or biomechanical correlation
Although radiographic criteria were used for participant inclusion, the study did not perform follow-up imaging or biomechanical assessments to evaluate whether structural changes or functional improvements occurred in conjunction with reported symptom relief.
No evaluation of psychosocial factors
Important psychosocial variables – such as fear-avoidance behavior, depression, or pain catastrophizing – were not assessed. Given their known influence on pain perception and functional recovery in osteoarthritis, this omission may limit a comprehensive understanding of variability in treatment response.
Unmeasured confounders
Factors such as concurrent medication use, daily physical activity outside of therapy, nutritional status, or comorbid lower limb pathologies (e.g., hip or ankle dysfunction) were not controlled for in this study. These unmeasured confounders could have influenced the observed outcomes.
Recommendations
Future randomized controlled trials with larger cohorts and long-term follow-up are recommended to validate these findings and establish standardized treatment protocols for PFOA.
Integrating MET, targeted strengthening, and patellar mobilization into routine physiotherapy can enhance clinical outcomes and provide effective, non-invasive management for PFOA.
References
- 1. Crossley KM. Patellofemoral osteoarthritis: An important subgroup of knee osteoarthritis. Br J Sports Med 2015;49:325-32. [Google Scholar] [PubMed]
- 2. Smith BE, Selfe J, Thacker D, Hendrick P, Bateman M, Moffatt F, et al. Incidence and prevalence of patellofemoral pain: A systematic review and meta-analysis. PLoS One 2018;13:e0190892. [Google Scholar] [PubMed]
- 3. Deyle GD, Allison SC, Matekel RL, et al . Physical therapy treatment effectiveness for osteoarthritis of the knee: A randomized comparison. Phys Ther 2011;91:462-78. [Google Scholar] [PubMed]
- 4. Neal BS, Lack S, Lankhorst NE, et al . Does hip strengthening improve outcomes in people with patellofemoral pain? A systematic review and meta-analysis. Br J Sports Med 2019;53:593-603. [Google Scholar] [PubMed]
- 5. Jan MH, Lin JJ, Lin YF, et al . Effects of passive stretching and proprioceptive neuromuscular facilitation on the patellofemoral joint. J Orthop Sports Phys Ther 2012;42:286-95. [Google Scholar] [PubMed]
- 6. Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, et al. Patellofemoral pain. J Orthop Sports Phys Ther 2019;49:CPG1-95. [Google Scholar] [PubMed]
- 7. Aminaka N, Gribble PA. A systematic review of the effects of hip strengthening on knee pain and function in patients with patellofemoral pain syndrome. J Athl Train 2012;47:493-501. [Google Scholar] [PubMed]
- 8. Powers CM. The influence of abnormal hip mechanics on knee injury. J Orthop Sports Phys Ther 2010;40:42-51. [Google Scholar] [PubMed]
- 9. Ferber R, Bolgla LA, Earl-Boehm JE, Emery C, Hamstra-Wright K. Strengthening and movement retraining for treating PFP: A clinical commentary. Int J Sports Phys Ther 2015;10:378-92. [Google Scholar] [PubMed]
- 10. Watson L, Dixon J, Woby SR. Psychosocial factors in patellofemoral pain: A review. Man Ther 2012;17:447-52. [Google Scholar] [PubMed]
- 11. Willy RW, Meira EP, Powers CM. Rehabilitation of PFP syndrome: A review. J Orthop Sports Phys Ther 2012;42:A1-54. [Google Scholar] [PubMed]
- 12. Rathleff MS, Vicenzino B, Middelkoop M, et al . Patellofemoral pain in adolescence: A self-limiting condition? Br J Sports Med 2015;49:1004-9. [Google Scholar] [PubMed]
- 13. Selkow NM, Givens DL, Saliba EN, et al. The effects of patellar mobilization on pain and function in patients with PFOA. J Sport Rehabil 2013;22:1-8. [Google Scholar] [PubMed]
- 14. Selfe J, Callaghan M, Witvrouw E, et al . Targeted interventions for patellofemoral pain syndrome: A clinical commentary. Phys Ther Sport 2013;14:188-98. [Google Scholar] [PubMed]
- 15. Chevidikunnan MF, Al Saif A, Gaowgzeh RA, et al . The effectiveness of Muscle Energy Technique (MET) in musculoskeletal rehabilitation: A systematic review. J Phys Ther Sci 2016;28:3121-5. [Google Scholar] [PubMed]
- 16. Tennent DJ, Hylden CM, Johnson AE, et al. The efficacy of muscle energy techniques in treating musculoskeletal conditions. Am J Sports Med 2014;42:1012-9. [Google Scholar] [PubMed]
- 17. Petersen W, Ellermann A, Gösele-Koppenburg A, Best R, Rembitzki IV, Brüggemann GP, et al. Patellofemoral pain syndrome. Knee Surg Sports Traumatol Arthrosc 2014;22:2264-74. [Google Scholar] [PubMed]
- 18. Thomeé R, Augustsson J, Karlsson J. Patellofemoral pain syndrome: A review of current treatment strategies. Br J Sports Med 2012;46:275-81. [Google Scholar] [PubMed]
- 19. Al-Hakeim HK, Mahdi HK. Evaluation of muscle energy technique on knee OA patients. Int J Physiother Res 2014;2:670-6. [Google Scholar] [PubMed]
- 20. van der Heijden RA, Lankhorst NE, van Linschoten R, et al . Exercise therapy for adolescents and adults with patellofemoral pain: A systematic review and meta-analysis. Br J Sports Med 2015;49:327-34. [Google Scholar] [PubMed]