In early stages of frozen shoulder, combining intra-articular steroids with calcitonin nasal spray provides superior pain relief and functional improvement compared to steroids alone , suggesting an augmented therapeutic effect.
Dr. Gaurav Kumar Sharma, Department of Orthopaedics, All India Institute of Medical Sciences, Bilaspur, Himachal Pradesh, India. E-mail: dr.gaurav.ortho@aiimsbilaspur.edu.in
Introduction: Frozen shoulder is one of the commonest debilitating conditions with characteristic features of by pain and globally restricted range of motion of the shoulder. This study compares the efficacy of intra-articular steroids alone in comparison to the combined intra-articular steroids and calcitonin nasal spray in the management of early-stage frozen shoulder. We hypothesized that the combination therapy of intra-articular steroids and calcitonin nasal spray results in a better increase in shoulder function and superior pain relief. Along with decrease in disability in comparison to treatment with corticosteroids alone.
Materials and Methods: Less than 3 months was chosen as a critical period for defining early frozen shoulder. A prospective study was conducted on 434 patients diagnosed with early-stage frozen shoulder. Randomization of the patients was done in two treatment groups according to computer-generated tables after applying appropriate inclusion and exclusion criteria and taking written consent. Patients were randomly assigned to two groups: Group A received intra-articular corticosteroid injections alone, and Group B received a combination of intra-articular corticosteroid injections and calcitonin nasal spray. Post-intervention physiotherapy protocol was the same for both the groups. Paracetamol @ 15 mg/kg was used for pain management as and when required. To measure the outcomes, the Oxford Shoulder Score (OSS) was used at 12 weeks post-intervention.
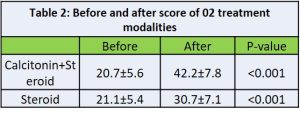
Results: There was improvement in OSS scores compared to baseline, which was found to be both clinically and statistically significant (P < 0.05). Patients who received combination therapy, i.e., Group B, exhibited superior clinical outcomes compared to patients who received intra-articular injections alone, i.e., Group A, at 12 weeks post-treatment. Group B demonstrated greater improvement in OSS scores (P < 0.001) as compared to Group A. Twenty-eight patients were lost to follow-up and 15 patients required analgesia like non-steroidal anti-inflammatory drugs other than paracetamol and hence excluded from the study.
Conclusion: The combination therapy of intra-articular corticosteroids and calcitonin nasal spray was found to be more efficacious as compared to intra-articular corticosteroids alone in the treatment of early-stage frozen shoulder. This combination therapy of intra-articular steroids and calcitonin provides better pain relief and shoulder function. This decrease in disability suggests its potential as a promising treatment option in the management of patients with early frozen shoulder.
Keywords: Frozen shoulder, adhesive capsulitis, intra-articular steroids, calcitonin nasal spray, combination therapy, pain relief, shoulder function.
Frozen shoulder is well-known cause of progressive decrease in global glenohumeral movements. The reported incidence in literature is about 2.4/100,000 individuals/year with the prevalence rate of 1–2% the population [1]. Global painful restriction of both active as well passive range of motion (ROM) along with normal X-rays is the hallmark of frozen shoulder. The disease progresses through 3 main stages, which may overlap. Stage 1 lasts for 2–9 months with pain as the predominant symptom. Stage 2 lasts from 4 months to 12 months with stiffness as a predominant symptom. Stage 3 is the recovery stage with progressive decline in pain and stiffness lasting 5–24 months. However, this time frame is variable in different patients. The British Elbow and Shoulder Society/British Orthopaedic Association has published recommendations in patient care pathway for frozen shoulder [2]. They have suggested nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroid injection, domestic exercise program and supervised physiotherapy as interventions suitable for primary care. Secondary care interventions advised by them include manipulation under anaesthesia, arthroscopic capsular release, distention arthrogram or hydro dilatation, physiotherapy and corticosteroid injection to supplement any of the above interventions. Management of adults with primary frozen shoulder in secondary care (UKFROST): multicentric pragmatic three-arm, superiority randomized control trial compared manipulation under anesthesia, arthroscopic capsular release, and early structured physiotherapy [3,4]. They found that all mean differences on the assessment of shoulder pain and function, Oxford Shoulder Score (OSS) at primary endpoint of 12 months were less than the target differences. None of the 3 interventions was clinically superior. Arthroscopic capsular release carried higher risks, and manipulation under anaesthesia was most cost-effective. Among the primary care remedies against frozen shoulder, calcitonin has not been studied in majority of clinical trials. Calcitonin is a polypeptide hormone secreted from parafollicular cells off thyroid. Calcitonin has been administered intranasally to decrease pain in various conditions such as complex regional pain syndrome, rheumatoid arthritis, fracture, spinal metastasis, and bone tumours [5]. It has been shown that long-term administration of calcitonin is safe and devoid of any serious side effects. Calcitonin effectively improves the messenger ribonucleic acid (mRNA) expression of fibrosis-related molecules and decreases the enhanced cell substrate addition ability of frozen shoulder fibroblasts. Calcitonin might achieve these effects by interacting with calcitonin receptors expressed on frozen shoulder fibroblast’s surface and activating the downstream protein kinase C or protein kinase A pathways [6]. Calcitonin has shown faster pain relief and significant improvement in shoulder ROM in patients with frozen shoulder being treated for post-menopausal osteoporosis. Similar findings were found in a double-blinded randomized clinical trial which compared nasal calcitonin spray and placebo in treating frozen shoulder patients and found that the calcitonin-treated group experienced much more effective improvement than the control group [7-9]. Since intra-articular steroids are widely used primary care intervention for frozen shoulder, we proposed this study to investigate the added advantage of intranasal calcitonin spray to steroids, if any.
This was a prospective evaluation to study the outcome of intra-articular steroids and nasal calcitonin spray in early-stage frozen shoulder patients. This study involved the patients presenting to the orthopedics outpatient department with stage one frozen shoulder from January 1st, 2021, to December 2022.
Study design
This study was designed as a prospective study conducted at a single center. All participants were given the choice to opt for any arm and were provided written informed consent before enrolment.
Participants
The study included adult patients aged between 30 and 70 years with early-stage frozen shoulder based on clinical evaluation and imaging findings.
Exclusion criterion
- Patients with duration of symptoms more than 3 months
- Medical history of heart disease, thyroid disorders, stroke, parathyroid disorders, metabolic disorders
- Previous history of trauma
- Previous history of corticosteroid injection, bilateral frozen shoulder
- Previous history of infections, fractures, rotator cuff arthropathy
- Previous history of any kind of shoulder surgery.
Early frozen shoulder was defined as a painful and stiff shoulder with painful restriction of active and passive ROM of the shoulder, including abduction <100° and 50% reduction in external rotation, along with normal shoulder radiography along with a duration of these symptoms of not more than 3 months.
Sample size calculation
The sample size was calculated based on the anticipated effect size and power analysis. With an alpha error of 0.05 and a power of 80%, a minimum sample size of 60 patients per group was determined to detect a clinically significant difference in outcome measures.
Randomization
Participants were randomly assigned to two treatment groups using computer-generated randomization codes. Allocation concealment was ensured through opaque, sealed envelopes.
Interventions
Group A: Intra-articular corticosteroid injections
Participants in Group A received intra-articular injections of triamcinolone acetonide (40 mg/mL) under ultrasound guidance. A total of 3 mL of triamcinolone mixed with 2 mL of 2% lignocaine was administered under aseptic conditions into the glenohumeral joint under ultrasound guidance.
Group B: Combined intra-articular corticosteroid injections and calcitonin nasal spray
Participants in Group B received the same intra-articular corticosteroid injections as Group A. In addition, they were instructed to use calcitonin nasal spray (200 IU) twice daily for 10 weeks. Patients were instructed to take Paracetamol @ 15 mg/kg as and when required for pain management. Requirement of other NSAIDs was recorded, and such patients were excluded from the study.
Outcome measures
Primary outcome
Shoulder function, pain, ROM and activities of daily living assessed subjectively by OSS [10]. Assessments were conducted before the intervention and 12 weeks post-treatment by blinded assessors. Demographic characteristics such as age, gender, history of shoulder trauma, history of shoulder pain-related treatment other than steroids, nocturnal pain and history of systemic diseases were also recorded in both groups.
Statistical analysis
Data were analyzed using appropriate statistical methods, including repeated measures analysis of covariance (ANCOVA), independent t-tests, and Chi-square tests. Statistical significance was set at P < 0.05.
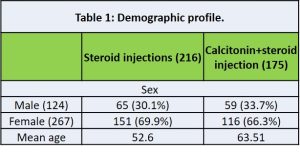
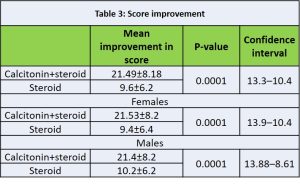
A total of 434 patients were enrolled in the study. 28 patients were lost to follow-up and 15 patients required analgesia other than paracetamol and were thus excluded from the study. So with the leftover of 391 patients recruited in the study were randomly assigned to Group A (n = 216) or Group B (n = 175). Demographic characteristics were comparable between the two groups at baseline (Table 1). Calculation of means, standard deviations, and frequencies for all variables (OSS scores, age, sex, treatment modalities) was done. Paired sample t-tests were used for each treatment group to compare pre- and post-treatment OSS scores. Unpaired sample t-tests were done to compare mean improvement in OSS scores across two different groups. The effect of two different modalities across different age groups and sex was done using ANCOVA. Regression analysis to explore the relationship between treatment modalities, age, sex, and improvement in OSS score was also explored. Both treatment groups demonstrated significant improvements in OSS scores compared to baseline (P < 0.05) (Table 2). However, Group B, receiving the combination therapy, exhibited superior outcomes compared to Group A at 12 weeks post-treatment. Group B showed greater improvement in OSS s indicating reduced pain and disability and better shoulder function (P < 0.001) compared to Group A (Table 3). On further ANCOVA analysis of age with treatment outcomes, no significant difference was found. Both groups had significant improvement after treatment, but the groups with calcitonin with steroid injections received a better outcome in terms of improvement of OSS score. There was no effect of gender or age on outcome.
Frozen shoulder management has been a controversy since its description by Codman in 1934 [11]. Histochemical studies have demonstrated synovial inflammation and fibrosis of the articular capsule [1,12]. Early immune response with elevated levels of alarmins and binding to the receptor of advanced glycation end products starts the cascade of inflammation [13-16]. The activation of nuclear factor κB pathway along with mechanical stress stimulates the release of inflammatory cytokines such as Transforming Growth Factor-beta (TGFb), which has a predominant role. Fibroblasts proliferate and differentiate into myofibroblasts, resulting in an imbalance of extracellular matrix turnover resulting in a thickened glenohumeral capsule and, henceforth, stiffness [17]. Based on the pathophysiological mechanism in frozen shoulder, it can be explained why intra-articular are successful in early frozen shoulder and why the intensity of physiotherapy should be guided by tissue irritability [18]. Intra-articular injection of corticosteroids is useful to reduce pain in patients during pain predominant phase [19-21]. Calcitonin decreases systemic inflammatory response and stimulates the release of endorphins [22]. Cultured fibroblast from frozen shoulder patient stimulated with salmon calcitonin showed a significant decrease in the production of collagen types 1 and 3. Synthesis of TGFb1 mRNA was suppressed by salmon calcitonin and the adhesion ability of fibroblasts also decreased. Apoptosis of the cultured fibroblast was also seen with high levels of salmon calcitonin. The efficacy of nasal calcitonin spray has been demonstrated in a placebo-controlled double-blind randomized trial [7,18]. The mean reported the duration of spontaneous frozen shoulder resolution without any treatment is 15–30 months [23]. However, the disease itself is debilitating and hence should be treated at the earliest to limit joint capsule fibrosis. In our study, the incidence of frozen shoulder was 2%. The incidence of frozen shoulder was higher in females as compared to males. We had to add intra-articular steroid to the calcitonin group because calcitonin does not give instant pain relief in frozen shoulder, and hence, the patient is likely to abandon calcitonin treatment. While the results of this study are promising, several limitations should be acknowledged. First, there was no untreated group of patients in this study to compare with. Second, it cannot be authenticated that all patients followed home-based physiotherapy protocol identically. Future studies with larger cohorts are warranted to confirm these results. In addition, the follow-up period of 12 weeks may not capture long-term outcomes and recurrence rates of frozen shoulder. Longer-term follow-up studies are needed to assess the durability of treatment effects and potential recurrence rates.
The combination of intra-articular corticosteroids and calcitonin nasal spray appears to be more effective than intra-articular corticosteroids alone in the management of early-stage frozen shoulder. This combination therapy provides superior pain relief, improved shoulder function, and reduced disability, suggesting its potential as a promising treatment option for patients with early frozen shoulder. Further studies are warranted to elucidate these synergistic mechanisms and long-term outcome of this treatment approach.
In early frozen shoulder, combination therapy works better than monotherapy—delivering quicker pain relief and better function.
References
- 1. Akbar M, McLean M, Garcia-Melchor E, Crowe LA, McMillan P, Fazzi UG, et al. Fibroblast activation and inflammation in frozen shoulder. PLoS One 2019;14:e0215301. [Google Scholar] [PubMed]
- 2. Rangan A, Goodchild L, Gibson J, Brownson P, Thomas M, Rees J, et al. Frozen shoulder. Shoulder Elbow 2015;7:299-307. [Google Scholar] [PubMed]
- 3. Rangan A, Brealey SD, Keding A, Corbacho B, Northgraves M, Kottam L, et al. Management of adults with primary frozen shoulder in secondary care (UK FROST): A multicentre, pragmatic, three-arm, superiority randomised clinical trial. Lancet 2020;396:977-89. [Google Scholar] [PubMed]
- 4. Brealey S, Northgraves M, Kottam L, Keding A, Corbacho B, Goodchild L, et al. Surgical treatments compared with early structured physiotherapy in secondary care for adults with primary frozen shoulder: The UK FROST three-arm RCT. Health Technol Assess 2020;24:1-162. [Google Scholar] [PubMed]
- 5. Yazdani J, Khiavi RK, Ghavimi MA, Mortazavi A, Hagh EJ, Ahmadpour F. Calcitonin as an analgesic agent: Review of mechanisms of action and clinical applications. Braz J Anesthesiol 2019;69:594-604. [Google Scholar] [PubMed]
- 6. Yang R, Deng H, Hou J, Li W, Zhang C, Yu M, et al. Investigation of salmon calcitonin in regulating fibrosis-related molecule production and cell-substrate adhesion in frozen shoulder synovial/capsular fibroblasts. J Orthop Res 2020;38:1375-85. [Google Scholar] [PubMed]
- 7. Rouhani A, Mardani-Kivi M, Bazavar M, Barzgar M, Tabrizi A, Hashemi-Motlagh K, et al. Calcitonin effects on shoulder adhesive capsulitis. Eur J Orthop Surg Traumatol 2016;26:575-80. [Google Scholar] [PubMed]
- 8. Alghamdi A, Alyami AH, Althaqafi RM 2nd, Alzeyadi A, Alrubaei FS, Alyami AA, et al. Cytokines’ role in the pathogenesis and their targeting for the prevention of frozen shoulder: A narrative review. Cureus 2023;15:e36070. [Google Scholar] [PubMed]
- 9. Waldburger M, Meier JL, Gobelet C. The frozen shoulder: Diagnosis and treatment. Prospective study of 50 cases of adhesive capsulitis. Clin Rheumatol 1992;11:364-8. [Google Scholar] [PubMed]
- 10. Angst F, Schwyzer HK, Aeschlimann A, Simmen BR, Goldhahn J. Measures of adult shoulder function: Disabilities of the arm, shoulder, and hand questionnaire (DASH) and its short version (quickDASH), shoulder pain and disability index (SPADI), American shoulder and elbow surgeons (ASES) society standardized shoulder assessment form, constant (murley) score (CS), simple shoulder test (SST), Oxford shoulder score (OSS), shoulder disability questionnaire (SDQ), and western ontario shoulder instability index (WOSI). Arthritis Care Res (Hoboken) 2011;63 Suppl 11:S174-88. [Google Scholar] [PubMed]
- 11. De La Serna D, Navarro-Ledesma S, Alayon F, Lopez E, Pruimboom L. A comprehensive view of frozen shoulder: A mystery syndrome. Front Med (Lausanne) 2021;8:663703. [Google Scholar] [PubMed]
- 12. Kim YS, Lee YG, Park HS, Cho RK, Lee HJ. Comparison of gene expression of inflammation- and fibrosis-related factors between the anterior and posterior capsule in patients with rotator cuff tear and shoulder stiffness. Orthop J Sports Med 2021;9:23259671211032543 . [Google Scholar] [PubMed]
- 13. Schaefer L. Complexity of danger: The diverse nature of damage-associated molecular patterns. J Biol Chem 2014;289:35237-45. [Google Scholar] [PubMed]
- 14. Yano T, Hagiwara Y, Ando A, Kanazawa K, Koide M, Sekiguchi T, et al. RAGE-dependent NF-kB inflammation processes in the capsule of frozen shoulders. J Shoulder Elbow Surg 2020;29:1884-91. [Google Scholar] [PubMed]
- 15. Hayashi K, Nikolos F, Lee YC, Jain A, Tsouko E, Gao H, et al. Tipping the immunostimulatory and inhibitory DAMP balance to harness immunogenic cell death. Nat Commun 2020;11:6299. [Google Scholar] [PubMed]
- 16. Roh JS, Sohn DH. Damage-associated molecular patterns in inflammatory diseases. Immune Netw 2018;18:e27. [Google Scholar] [PubMed]
- 17. Cho CH, Song KS, Kim BS, Kim DH, Lho YM. Biological aspect of pathophysiology for frozen shoulder. Biomed Res Int 2018;2018:7274517. [Google Scholar] [PubMed]
- 18. Kraal T, Lubbers J, Van Den Bekerom MP, Alessie J, Van Kooyk Y, Eygendaal D, et al. The puzzling pathophysiology of frozen shoulders – a scoping review. J Exp Orthop 2020;7:91. [Google Scholar] [PubMed]
- 19. Prestgaard T, Wormgoor ME, Haugen S, Harstad H, Mowinckel P, Brox JI. Ultrasound-guided intra-articular and rotator interval corticosteroid injections in adhesive capsulitis of the shoulder: A double-blind, sham-controlled randomized study. Pain 2015;156:1683-91. [Google Scholar] [PubMed]
- 20. Oh JH, Oh CH, Choi JA, Kim SH, Kim JH, Yoon JP. Comparison of glenohumeral and subacromial steroid injection in primary frozen shoulder: A prospective, randomized short-term comparison study. J Shoulder Elbow Surg 2011;20:1034-40. [Google Scholar] [PubMed]
- 21. Shin SJ, Lee SY. Efficacies of corticosteroid injection at different sites of the shoulder for the treatment of adhesive capsulitis. J Shoulder Elbow Surg 2013;22:521-7. [Google Scholar] [PubMed]
- 22. Cho CH, Bae KC, Kim DH. Treatment strategy for frozen shoulder. Clin Orthop Surg 2019;11:249-57. [Google Scholar] [PubMed]
- 23. Diercks RL, Stevens M. Gentle thawing of the frozen shoulder: A prospective study of supervised neglect versus intensive physical therapy in seventy-seven patients with frozen shoulder syndrome followed up for two years. J Shoulder Elbow Surg 2004;13:499-502. [Google Scholar] [PubMed]