Successful surgical treatment of patella instability after total knee arthroplasty with Insall technique had a good clinical outcome.
Dr. Nikolaos Georgiadis, Department of Orthopedic Surgery and Traumatology, Unit for Sport Injuries, General Hospital of Thessaloniki “Agios Pavlos”, Thessaloniki, Greece. Email: ngeorgiadis1994@gmail.com
Introduction: Patella instability and maltracking is a serious complication following total knee replacement that can lead to poor outcomes for the patient and contribute to early failure. The incidence of patella maltracking ranges from 1% to 20% after total knee arthroplasty (TKA), with post-operative anterior knee pain being an important indicator. There are many different surgical approaches for the management of post-operative patella maltracking with very good outcomes. However, the most crucial step is to identify the underlying etiology.
Case Report: A 71-year-old Caucasian woman presented to our orthopedic department due to chronic right knee pain, which had worsened over the past year. She was diagnosed with osteoarthritis and was scheduled for a TKA. Three years postoperatively, she returned for examination due to anterior knee pain. Patellar instability was observed and intensive extensor mechanism strengthening and physiotherapy were recommended. Three months later, she presented with severe pain and inability to move her knee. Imaging revealed a fracture and dislocation of the patella. She was surgically treated with lateral release and proximal realignment of the extensor mechanism, according to Insall procedure, with great post-operative outcome.
Conclusion: The etiology of post-operative patella instability and dislocation in most cases is due to component malposition or extensor mechanism imbalance. The surgeon should be careful and should take measures preoperatively and intraoperatively to prevent this scenario.
Keywords: Total knee arthroplasty, patella instability, lateral release, insall procedure.
The aging population has made total knee arthroplasty (TKA) a common practice in the orthopedic community, generally yielding very good results [1,2]. However, there are still dissatisfied patients with the outcome despite advances in knowledge and materials [1,2]. One of the most serious post-operative complications is patellar instability and can cause anterior knee pain, functional limitation, early wear of the components, and patella fracture [1,2,3]. Although there are pre-operative and intraoperative techniques commonly accepted for preventing this scenario, when it comes to post-operative management that it appears to be less clear [1,2]. Many procedures have been suggested as the best way to treat patients with post=operative patella displacement and are still under debate. The most important step is to identify the underlying etiology [1,2]. When it comes to component malposition, one of the most common causes, the recommended approach is revision surgery. However regarding soft-tissue imbalance, there are many procedures described in the literature that can be used alone or in combination as complimentary [1,2].
History
A 71-year-old Caucasian woman presented to our orthopedic department due to chronic right knee pain, which had worsened over the past year. Clinically, mild valgus knee deformity of approximately 10° was observed. Her medical history included arterial hypertension, dyslipidemia, and osteopenia, with a body mass index of 33. She was diagnosed with the right knee osteoarthritis (Fig. 1) and was scheduled for a TKA.
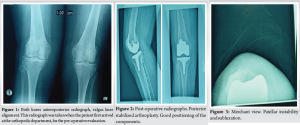
The patient underwent cemented posterior stabilized TKA. A medial parapatelar approach was used. During surgery, a bony prominence was observed on the lateral articular patellar surface which was then removed and reshaped. The patella was preserved, reshaped, and denervated.[4,5] The medial retinaculum was found to be loose and friable. During stability testing, the patella was centered in the trochlea groove throughout the full range of motion of the knee (Fig. 2).
Signs and symptoms
Three years later, the patient came to our orthopedic department due to anterior knee pain with difficulty in bending and extending the knee. She was clinically examined and the knee was found stable according to valgus, varus test. However, patellar instability was observed clinically and confirmed with X-rays (Merchant view) (Fig. 3). Initially, the patient was advised to undergo intensive physiotherapy, strengthening of the extensor mechanism and particularly the vastus medialis. Three months later, she presented with severe patellar pain and an inability to flex or extend the knee.
Radiographic evaluation
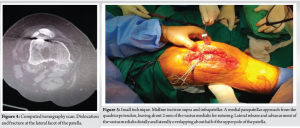
A computed tomography (CT) scan revealed dislocation and fracture at the lateral facet of the patella (Fig. 4). The placement of the TKA components was checked and found to be correct, so we focused on the instability of the extensor mechanism and the soft-tissue imbalance.
Treatment
Evaluating the proper placement of the arthroplasty components, the patellar fracture, the reduced anteroposterior diameter of the patella, the loose medial retinaculum, and the patient’s history of osteopenia, we decided on surgical management with proximal realignment of the extensor mechanism according to Insall procedure, as it is described in his book, complemented by a lateral release. We started with a midline incision supra and infrapatellar, approximately 10 cm long, following the previous scar. We continued with a medial parapatellar approach from the quadriceps tendon, leaving about 2 mm of the vastus medialis for suturing, down medially to the patellar ligament. We then proceeded with the eversion of the patella and located the fragment of the lateral facet, which was excised and found to be approximately 20% of the patella. Next, we performed a lateral release and advanced the vastus medialis distally and laterally in line with his oblique portion, overlapping about half of the upper pole of the patella (Fig. 5), and sutured the vastus medialis in this position. We checked the centering of the patella in the trochlea groove throughout the full range of knee motion and found it to be satisfactory (Fig. 6). After that, the incision underwent a rich lavage and was closed.
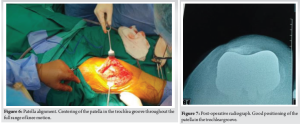
Postoperatively, we immobilized the knee with a thigh-calf brace at 30° of knee flexion for 4 weeks and the patient was advised to walk with partial weight-bearing using crutches. Then, a hinged knee brace was used, and the range of motion was gradually increased to 90° over the next 2 weeks. Finally, after 6 weeks, the brace was removed, and intensive physiotherapy was recommended with the goal of achieving full range of motion of the joint and full weight-bearing. One year postoperatively, the patient was revaluated at our department and was found to be pain free and with satisfactory range of motion of the knee joint up to approximately 100° of flexion. There were no clinical signs of patellar instability or subluxation and the patella was found centered in the trochlear groove on a Merchant X-ray view (Fig. 7).
In general, the risk factors for patellofemoral joint instability after total knee replacement can be categorized into three groups, component positioning and surgical technique, soft-tissue balancing, and other causes [1,2,3,6]. In our patient, the femoral and tibial components were found to be correctly placed on the CT scan. The patient had a mild valgus knee joint alignment of approximately 10°. As described in the literature, valgus knees are predisposed to patellar instability [2,7]. In cases of valgus deformity, the posterior cruciate ligament is often contracted, making it more difficult for the surgeon to correct the deformity.[8] In addition, posterior-stabilized components tend to be more stable and can be more lateralized to improve patellar tracking in the trochlear groove [9,10,11]. This is why we decided to use a posterior-stabilized total knee replacement in our patient, along with the fact that the medial retinaculum appeared very thin. There is also a greater risk of soft-tissue imbalance in patients who undergo a medial parapatellar approach [1,12]. We believe that in our patient, the main factors contributing to secondary post-operative patellar subluxation were the valgus malalignment, which led to chronic imbalance with a fragile medial retinaculum and chronic impingement of the lateral facet of the patella where the bony prominence was found. Due to the thinned and fractured patella, we chose not to reconstruct the medial patellofemoral ligament, even though excellent results are reported in the literature [1,13]. We also avoided distal realignment due to the risk of material failure, nonunion, patellar tendon rupture, and osteonecrosis of the fragment, especially after a cemented TKA in an osteopenic patient [1,2]. Hence, we proceeded with proximal realignment using the Insall procedure [1], which appeared to be safer [2] for the patient, along with a lateral retinaculum release. In addition, due to the removal of the fractured lateral facet, we performed a lateral facectomy, which in combination seem to have good results for patellar instability after TKA [1,12].
Proximal realignment according to Insall procedure appears to be a good choice in our case for patellar instability after TKA, especially when there is poor patellar bone stock for medial patelofemoral ligament reconstruction and also it avoids the risks associated with distal realignment. One year postoperatively, the patient was pain-free, fully functional, and had a satisfactory range of motion of the knee joint.
Care must be taken from the orthopedic surgeons preoperatively, but especially intraoperatively, as this is when the etiology for patellar instability most often occurs. There are many surgical procedures described in the literature for patellar instability after TKA with excellent results. However, it remains an additional surgery that the patient must undergo, leading to further physical and psychological stress.
References
- 1.Ferri R, Digennaro V, Panciera A, Bogucki BD, Cecchin D, Manzetti M, et al. Management of patella maltracking after total knee arthroplasty: A systematic review. Musculoskelet Surg 2023;107:143-57. [Google Scholar | PubMed]
- 2.Motsis EK, Paschos N, Pakos EE, Georgoulis AD. Review article: Patellar instability after total knee arthroplasty. J Orthop Surg (Hong Kong) 2009;17:351-7. [Google Scholar | PubMed]
- 3.Malo M, Vince KG. The unstable patella after total knee arthroplasty: Etiology, prevention, and management. J Am Acad Orthop Surg 2003;11:364-71. [Google Scholar | PubMed]
- 4.Xie X, Pei F, Huang Z, Tan Z, Yang Z, Kang P. Does patellar denervation reduce post-operative anterior knee pain after total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 2015;23:1808-15. [Google Scholar | PubMed]
- 5.Lie DT, Gloria N, Amis AA, Lee BP, Yeo SJ, Chou SM. Patellar resection during total knee arthroplasty: Effect on bone strain and fracture risk. Knee Surg Sports Traumatol Arthrosc 2005;13:203-8. [Google Scholar | PubMed]
- 6.Song SJ, Detch RC, Maloney WJ, Goodman SB, Huddleston JI 3rd. Causes of instability after total knee arthroplasty. J Arthroplasty 2014;29:360-4. [Google Scholar | PubMed]
- 7.Petersen W, Rembitzki IV, Brüggemann GP, Ellermann A, Best R, Koppenburg AG, et al. Anterior knee pain after total knee arthroplasty: A narrative review. Int Orthop 2014;38:319-28. [Google Scholar | PubMed]
- 8.Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am 2005;87 Suppl:1271-84 [Google Scholar | PubMed]
- 9.Rossi R, Rosso F, Cottino U, Dettoni F, Bonasia DE, Bruzzone M. Total knee arthroplasty in the valgus knee. Int Orthop 2014;38:273-83. [Google Scholar | PubMed]
- 10.Kurtz SM, Ong KL, Lau E, Widmer M, Maravic M, Gomez-Barrena E, et al. International survey of primary and revision total knee replacement. Int Orthop 2011;35:1783-9. [Google Scholar | PubMed]
- 11.Aglietti P, Buzzi R, Gaudenzi A. Patellofemoral functional results and complications with the posterior stabilized total condylar knee prosthesis. J Arthroplasty 1988;3:17-25. [Google Scholar | PubMed]
- 12.Shen XY, Zuo JL, Gao JP, Liu T, Xiao JL, Qin YG. New treatment of patellar instability after total knee arthroplasty: A case report and review of literature. World J Clin Cases 2020;8:5487-93. [Google Scholar | PubMed]
- 13.Lie DT, Gloria N, Amis AA, Lee BP, Yeo SJ, Chou SM. Patellar resection during total knee arthroplasty: Effect on bone strain and fracture risk. Knee Surg Sports Traumatol Arthrosc 2005;13:203-8. [Google Scholar | PubMed]