In this case report, we evaluate the importance of a holistic approach in managing an incidental finding of tuberculous arthritis of the knee and the effectiveness of total knee arthroplasty for the same.
Dr. Andela Veerendra, Department of Orthopaedics, MGM Medical College, Sambhajinagar, Maharashtra, India. E-mail: andelaveerendra87@gmail.com
Introduction: Tuberculosis (TB) remains a significant global health challenge, with 10.6 million new cases and 1.3 million deaths reported in 2022. Extrapulmonary TB accounts for approximately 16% of all cases, with osteoarticular TB being a notable subset. Tubercular arthritis of the knee is a rare manifestation, often misdiagnosed due to its atypical presentation. Total knee arthroplasty (TKA) is considered the treatment of choice in advanced cases; however, evidence on outcomes in cases with incidental tubercular findings remains limited. This report highlights a case of tubercular arthritis of the knee diagnosed incidentally and evaluates the clinical outcomes following TKA.
Case Report: A 55-year-old female patient of South Asian descent presented with progressive left knee pain and restricted range of motion. Clinical and radiological investigations revealed signs of inflammatory pathology, including elevated serum markers and imaging findings consistent with arthritis. Histopathological examination of the synovial tissue confirmed tubercular arthritis. The patient underwent surgical debridement followed by TKA. Postoperatively, the patient demonstrated significant functional improvement and was closely monitored over a 2-year follow-up period, with no recurrence of infection or prosthesis-related complications.
Conclusion: The atypical presentation of tubercular arthritis of the knee poses a diagnostic challenge and carries a high risk of mismanagement if not properly evaluated. This case underscores the importance of thorough radiological and histopathological assessments for accurate diagnosis. Our findings suggest that a combined approach of debridement and TKA offers effective results, minimizing the risk of post-operative complications, including periprosthetic joint infections. This report adds valuable evidence to the orthopedic literature, demonstrating that TKA is a viable option for managing tubercular arthritis of the knee, which provided that the diagnosis is confirmed, and appropriate surgical and medical protocols are followed.
Keywords: Total knee arthroplasty, tubercular arthritis, osteoarticular tuberculosis.
Tuberculosis (TB) is a bacterial infection caused by Mycobacterium tuberculosis that primarily affects the lungs but can also affect other parts of the body, such as the joints. According to the World Health Organization’s (WHO’s) Global TB Report 2023, a global total of 8 million people were reported as newly diagnosed with TB in 2023, and an estimated 1 million deaths were reported in the same year, highlighting the major public health challenge that TB poses [1]. Bone and joint TB are the third most common form of extrapulmonary TB, representing ten to fifteen percent of case [2]. It primarily affects the spine and large joints. Patients with tuberculous arthritis of the knee may experience symptoms such as joint pain, swelling, stiffness, and loss of mobility. It is important to diagnose and treat TB arthritis promptly to prevent further joint damage and complications. Treatment for tuberculous arthritis often involves a combination of anti-TB medications as well as surgical intervention in some cases. Arthrodesis and total knee arthroplasty (TKA) are among the surgical options, but routine debridement followed by TKA is a frequently used technique for treating advanced degenerative osteoarthritis of the knee. Arthrodesis may lead to decreased function in the affected limb and is associated with multiple complications such as non-union and leg-length discrepancy. Although it can provide control of the infection and relief of pain, TKA is often preferred for better functional outcomes. In this case report, we evaluate the outcome of TKA in a patient with incidental findings of TB of the knee joint with severe joint destruction and no prior history of TB, leading to complicated surgical planning [3]. Patients are often misdiagnosed with a primary joint condition, such as rheumatoid arthritis or osteoarthritis, when they actually have other underlying disorders such as early-stage knee TB. If knee TB is mistaken for a noninfectious joint disease and treated with a total knee replacement (TKR), it can lead to more complications in treatment. This increases patient morbidity, financial costs, and the risk of complications, such as periprosthetic joint infections (PJIs), which can further complicate recovery and treatment. The knee is a frequently involved organ in osteoarticular TB. Due to a lack of specific clinical signs, TB of the knee has typically led to considerable bone destruction by the time that it is definitively diagnosed [4].
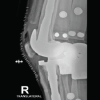
A 55-year-old female presented with complaints of pain and swelling of the left knee along with difficulty in walking and standing for 8 months. Serum inflammatory markers were elevated: Erythrocyte sedimentation rate (ESR) was 42 mm/h, and C-reactive protein-quantitative was twelve milligrams per deciliter. On examination, the left knee was swollen, with valgus deformity, warm on palpation, and painful on movement. The patient had a fixed flexion deformity of 30° and maximum flexion of up to 100° (Fig. 1a and b). Pre-operative knee radiographs showed significant destruction of the knee joint along with soft-tissue edema and erosion of the femoral and tibial condyles (Fig. 2).

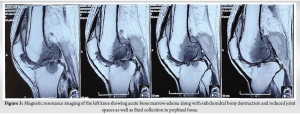
The patient was further evaluated through a series of clinical, radiological, and blood investigations. Magnetic resonance imaging (MRI) revealed acute bone marrow edema in the distal shaft and condyles of the femur and tibial plateau, subchondral bony destruction, and reduced joint spaces in the medial and lateral tibiofemoral compartments. In addition, loculated fluid collection in the popliteal fossa and mild collection in the suprapatellar bursa were noted (Fig. 3), confirming an inflammatory pathology.
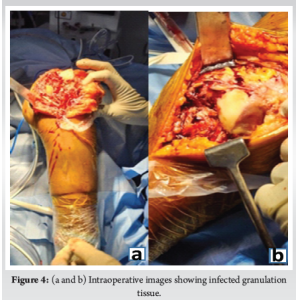
The patient first underwent surgical debridement. On dissection, extensive synovial proliferation and infected granulation tissue were seen (Fig. 4a, b) and debrided. The samples were sent for chip-based nucleic acid amplification test (TRUE NAT), histopathological, and microbiological culture and sensitivity tests. The reports confirmed tubercular arthritis, and further planning for arthroplasty was made. The histopathology and cytology report revealed multiple well-formed granulomas within fibrocollagenous tissue with granulomas composed of epithelloid cells, langhans gaint cells, and lymphocytes. Foci of caseous necrosis too were seen. M. tuberculosis was detected on TRUE NAT and there was no rifampicin resistance (Fig. 5 and 6).

The patient was considered for conventional TKA. The previous surgical scar for debridement through a midline incision followed by a medial parapatellar approach was used for the surgery. Using a legacy constrained condylar knee jig, distal femur and proximal tibia cuts were made. Size D femur was prepared with sequential rimming of the medullary canal of both the tibia and femur for stem placement. An intramedullary extension stem of size 12 mm by 100 mm was fixed with size D cemented femur and tibia size two with 11-mm by 100-mm extension stem, cemented with a 10-mm insert. The osteoporotic medial femoral condyle was supported with a 6-mm cannulated cancellous crew. Final implant placement was followed by thorough washing and closure in layers. Postoperatively, the patient was permitted to bear weight as tolerated, and the knee was immobilized in extension for 2 weeks. Thereafter, passive knee flexion was advanced gradually. Active knee extension with activity as tolerated was permitted after 6 weeks. One year later, the patient remained free of systemic and local infection and had a well-functioning prosthesis without any loosening. The range of motion was 0–100° with no extensor lag. Radiographs of 6 months and 1 year follow-up (Fig. 7 and 8) confirmed a well-fixed and well-positioned stemmed prosthesis with no evidence of bone destruction.

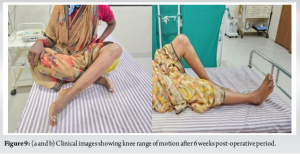
The patient was started on anti-tubercular treatment postoperatively after debridement according to weight class for 12 months with 2 months of intensive phase which includes isoniazid, rifampicin, pyrazinamide, and ethambutol and 10 months of continuation phase which includes isoniazid, rifampicin, and ethambutol according to the WHO guidelines for osteoarticular TB. The patient experienced improvement in knee range of motion with up to 100° of flexion and complete extension by the end of 6 weeks postoperatively (Fig. 9a and b). The levels of ESR decreased 2 months postoperatively. Patient’s pain significantly decreased, enabling a cautious rehabilitation process. The patient was followed up every 6 months for 2 years.
During the first 6 months follow-up, the patient showed elevated serum inflammatory markers but no clinical signs. This was managed by monitoring, and subsequently, the markers normalized after 6 months without any clinical signs of inflammation. There was no relapse of symptoms such as swelling, redness, or abscess formation in the following year. Follow-up X-rays did not show any loosening of the prosthesis, and the patient was walking comfortably without any walking aids.
Bone and joint TB are uncommon diseases, affecting 1–3% of all cases and 10–11% of extrapulmonary cases. The knee is ranked third, behind the spine and the hip. Imaging can occasionally help in diagnosis, allowing for timely and appropriate therapy. On conventional radiographs, joint TB is traditionally defined by Phemister’s triad, which comprises peripheral bone erosions, periarticular osteoporosis, and joint space constriction. Due to its excellent resolution and capacity to offer multiplanar imaging, MRI is now regarded as the standard test for suspecting tuberculous arthritis of the knee. In T1-weighted imaging, synovial thickening appears as an intermediate signal, while in T2-weighted imaging, it might appear as an intermediate or hypersignal. The intermediate signal represents caseous necrosis, whereas the hypersignal shows granulomas or synovial inflammation [5,6]. MRI, which is more sensitive than traditional X-rays in diagnosing bone erosions, is used in seventy percent of instances. These erosions, whether central or peripheral, show up as hyposignals in both T1- and T2-weighted imaging. Cartilage breakdown occurs in forty percent of patients, manifesting as localized or widespread thinning. Periarticular abscesses are divided into two parts: The abscess itself, which shows as hyposignal in T1-weighted imaging and hypersignal in T2-weighted imaging, and a peripheral ring, which appears as hypersignal in T1-weighted imaging and hyposignal in T2-weighted imaging. The differential diagnosis mostly includes pyogenic arthritis. MRI can be a useful tool in suggesting a diagnosis of tuberculous arthritis by identifying characteristic features such as mild inflammation, chondral and subchondral erosions, and preserved joint space height. In addition, the presence of an abscess and bone fragments may raise suspicion of TB. However, MRI alone is not definitive, as these findings can also be seen in other infections. The gold standard for diagnosis remains the identification of the pathogen through tissue cultures [7]. Inflammatory indicators such as ESR are frequently elevated in TB with recent onset and normal in the chronic or quiescent stage. In our instance, it was slightly above average levels. Other studies noted that the amount of ESR did not represent TB activity and hence should not impact the scheduling of TKA. Taken together, we urge that TKA be carefully but optimistically undertaken, even if ESR is high [8]. The decision to first debride and then plan TKA helped in evaluating and confirming tubercular knee and taking necessary steps toward further management. There has been controversy over the appropriate use of TKA in patients with TB arthritis. As previous studies suggested, the following:
- Although the rate of post-operative reactivation was rather high at 15%, TKA was successful in treating the majority of patients
- Although the duration of treatment varied, most authors acknowledged that perioperative anti-tubercular medication prevented reactivation, particularly in patients with an increased pre-operative ESR
- In patients with active TB of the knee, immediate TKA was not advised unless complete debridement and consistent treatment were guaranteed
- There was discussion on the best prosthesis choice. The claim that TKA could be used to treat advanced TB arthritis has been the subject of most prior research [8-11].
Studies underlined that TKA should be examined early in recent-onset TB, and other researchers believed that ongoing infection should not be a contraindication to arthroplasty. The danger of reactivation is always present and PJI can be effectively treated with either antitubercular treatment alone, a combination of medication and surgery, revision, or even arthrodesis.
- tuberculosis has biological features distinct from those of pyrogenic bacteria. According to studies, it clings slightly to metal surfaces but can cause local nidus development. These features of M. tuberculosis taught us that arthroplasty did not enhance the risk of TB reactivation, and that full debridement and post-operative antitubercular treatment were critical [10-12].
The incidence of osteoarticular TB is low. However, its atypical clinical manifestations often make it challenging to diagnose. TKA for advanced active TB of the knee can be considered safe therapy that relieves symptoms and improves function. A lengthy infection-free period is not required with TKA. Wide surgical debridement with a complete pathological diagnosis and appropriate post-operative antitubercular chemotherapy are the primary treatments for eradicating the infection and lowering the risk of TB reactivation. Multidisciplinary participation is crucial for optimizing treatment plans for such complicated illnesses, as this instance demonstrates. Long-term monitoring is necessary to evaluate prosthetic joint performance, identify possible recurrences, and assist the patient in returning to an active and satisfying lifestyle.
This case report emphasizes the critical importance of thorough diagnostic evaluation, including radiological and histopathological assessments, for patients presenting with atypical knee pain and swelling. Such an approach is essential to identify rare conditions like tuberculous arthritis, which can be easily misdiagnosed as other joint pathologies. The report demonstrates that TKA can be a safe and effective treatment option for advanced tuberculous arthritis when combined with staged debridement and post-operative antitubercular therapy. This method not only controls the infection but also ensures optimal functional recovery and long-term prosthesis stability. The case highlights the value of a multidisciplinary approach in managing complex conditions like osteoarticular TB, stressing the need for collaboration between orthopedic surgeons, infectious disease specialists, and radiologists. Long-term monitoring remains crucial to evaluate prosthesis performance and detect any recurrence of infection. This case is particularly relevant for clinicians managing patients with atypical joint presentations, demonstrating how a well-coordinated treatment strategy can achieve excellent outcomes even in challenging and uncommon scenarios. By documenting this approach, the report adds valuable insights to the orthopedic literature, providing guidance for the successful management of similar cases in the future.
References
- 1. WHO. WHO Global Tuberculosis Report. Geneva: WHO; 2023. [Google Scholar] [PubMed]
- 2. Desdiani D, Rizal H, Basuki A, Fadilah F. Case report: Delayed treatment of tuberculosis of the elbow joint. F1000Res 2022;10:486. [Google Scholar] [PubMed]
- 3. Vyravan PR, Choudhary BM, Kumar MM. Total knee replacement in tuberculous arthritis-reporting an unsuspected case. J Dent Med Sci (IOSR-JDMS) 2014;13:11-3. [Google Scholar] [PubMed]
- 4. Soeroso NN, Ananda FR, Rahmadhany H, Putra DD. Tuberculosis of the knee: A pitfalls in clinical settings (a case report and literature review). Int J Surg Case Rep 2020;71:14-8. [Google Scholar] [PubMed]
- 5. Nizar A, Misbah I, Purushothaman R, Rajabalaji V, Ashraf M, Balasubramanian N. A systematic review and qualitative analysis of studies performing total knee arthroplasty (TKA) in tuberculosis (TB) of the knee. Cureus 2024;16:e57964. [Google Scholar] [PubMed]
- 6. Bhattacharjee S, Prasad A, Ahlawat A, Pavan RB. The outcomes of total knee arthroplasty following the incidental finding of tuberculosis and its treatment: A prospective study. Indian J Tuberc 2023;71:460-64. [Google Scholar] [PubMed]
- 7. Samade R, Voskuil RT, Scharschmidt TJ. Two-stage TKA for tuberculosis septic arthritis of the knee masquerading as pigmented villonodular synovitis: A case report. The Knee 2022;38:30-5. [Google Scholar] [PubMed]
- 8. Ren B, Bai X, Zhang H, Sun L, Fang L, Liu B, et al. Need for anti-tuberculosis treatment in patients with latent tuberculosis infection who undergo arthroplasty: A case report. Ann Transl Med 2022;10:1410. [Google Scholar] [PubMed]
- 9. Wafiuddin M, Roslan AF, Zulkifly AH. Knee tuberculosis: A challenge in diagnosis and treatment. Borneo J Med Sci (BJMS) 2021;15:37. [Google Scholar] [PubMed]
- 10. Wang D, Sun XT, Zhang CF, Fang XY, Huang ZD, Zheng QC, et al. Total knee arthroplasty in patients with unsuspected tuberculosis of the joint: A report of four cases and a systematic review of the literature. Orthop Surg 2020;12:1900-12. [Google Scholar] [PubMed]
- 11. Habaxi KK, Wang L, Miao XG, Alimasi WQ, Zhao XB, Su JG, et al. Total knee arthroplasty treatment of active tuberculosis of the knee: A review of 10 cases. Eur Rev Med Pharmacol Sci 2014;18:3587-92. [Google Scholar] [PubMed]
- 12. Leclere LE, Franklin Sechriest V 2nd, Holley KG, Tsukayama DT. Tuberculous arthritis of the knee treated with two-stage total knee arthroplasty. A case report. J Bone Joint Surg Am 2009;91:186-91. [Google Scholar] [PubMed]
References
- 1.[Google Scholar | PubMed]