Clavicle fractures, though often benign, can be associated with subtle but life-threatening subclavian artery injuries requiring high clinical suspicion and prompt intervention.
Dr. Stef Biesemans, Department of Orthopaedic Surgery, Ziekenhuis Oost-Limburg, Genk, Belgium. E-mail: biesemansstef1@gmail.com
Introduction: Clavicle fractures are common, accounting for approximately 10% of all fractures, with midshaft fractures being the most prevalent. Despite the proximity of the subclavian artery to the clavicle, vascular injuries occur in <1% of cases.
Case Report: We present a case of a 36-year-old male with a midshaft clavicle fracture associated with subclavian artery transection. The subtle clinical signs of this severe injury can lead to delayed diagnosis and subsequent complications. We reviewed the literature of this rare injury, including 79 cases, to evaluate its clinical presentation and to formulate recommendations regarding diagnosis and treatment.
Conclusion: Awareness of this potentially life-threatening injury is important. Clavicle fractures may conceal life-threatening subclavian artery injuries, highlighting the need for careful vascular assessment and timely management.
Keywords: Clavicula, fracture, subclavian artery
Clavicle fractures occur frequently both in adult and pediatric patients, making up about 10% of all fractures. They typically result from direct blunt trauma to the clavicle or lateral shoulder. Most of these fractures occur in the midshaft and are typically managed conservatively with good results. The subclavian artery is in proximity to the midshaft clavicle (artery mean 17.02 mm and vein 12.45 mm) [1] but associated vascular lesions are rare and are estimated to occur in <1%. [2]. The signs of subclavian arterial injury can be subtle, especially in blunt trauma; however, urgent operative treatment is required. This study aims to provide an overview of orthopedic and vascular treatment in these specific conditions, based on a case report from our own trauma center combined with a review of the literature.
A 36-year-old man was admitted to our emergency department after falling with his mountain bike. The patient reported pain in the left clavicle and shoulder girdle region and difficulty to elevate the upper extremity. Mild swelling and local tenderness over the left midshaft clavicle were present. The ipsilateral upper extremity had a normal appearance, no discoloration, and neurological examination was normal. Pulsation of the radial artery at wrist level was weaker compared to the contralateral side. Medical imaging of the left shoulder region is shown in Fig. 1, 2, 3.

Figure 1: Radiographic imaging of the affected left shoulder region: Slightly displaced,
comminuted midshaft clavicle fracture.

Figure 2: Computed tomography – scan of the left shoulder region without contrast:
Visualization of a non definable portion of the left subclavian artery with a length of 36 mm.

Figure 3: Computed tomography – angiography confirms the lesion of the left
subclavian artery.
Urgent surgical exploration under general anesthesia was performed. An oblique incision was made over the clavicle, centered on the fracture site. During exploration of the fracture fragments, massive bleeding from the medial side of the fracture was encountered. The subclavian artery was mobilized proximally and distally from the fracture. Heparin was administered at 300 IU/kg, followed by proximal and distal control of the bleeding with arterial clamps. Complete transection of the anterior arterial wall was observed, with only a small piece of adventitia remaining on the posterior wall. A venous patch, taken from the ipsilateral greater saphenous vein, was sewn in place using 5–0 Prolene (Ethicon, Cornelia, USA) sutures. After proper de-airing, the clamps were removed, and good peripheral pulsations were confirmed. Protamine was administered to reverse the heparin. Second, the clavicle fracture was reduced and stabilized with 2 anteroposterior lag screws and anatomical locking clavicle plate (DePuy Synthes). Postoperatively, acetylsalicylic acid 80 mg was administered daily for 4 weeks. The post-operative course was uneventful with adequate revascularization of the upper extremity and successful bone healing.
Assessment 6 months after surgery demonstrated a full active range of motion of the left shoulder and flow permeability of the left subclavian artery on duplex ultrasound (Fig. 4).
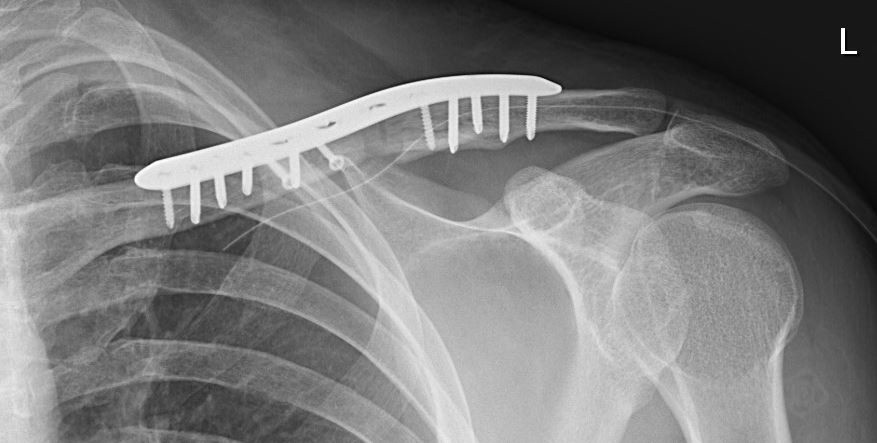
Figure 4: Radiographs 6 months after trauma demonstrate complete bony healing of the clavicle fracture.
Most clavicular fractures are isolated injuries, but associated lesions of the subclavian artery are possible due to its proximity to the fracture site. Subclavian and axillary artery injuries account for 5–10% of arterial trauma in civilians [3]. This potentially life-threatening injury could easily be missed, as symptoms can be very subtle. Posttraumatic subclavian artery lesions can present acutely as lacerations, dissections, pseudoaneurysms, or occlusion. Delayed presentation is also possible due to compression caused by callus formation.
The first case of subclavian artery lesion combined with clavicle fracture was reported in 1873 by Erichsen after initial conservative treatment and subsequent decompression incisions and even shoulder disarticulation, the patient ultimately died [4]. Since then, 78 more cases of subclavian vessel injury combined with clavicular fractures after blunt trauma have been reported. An overview of the literature is presented in Table 1.
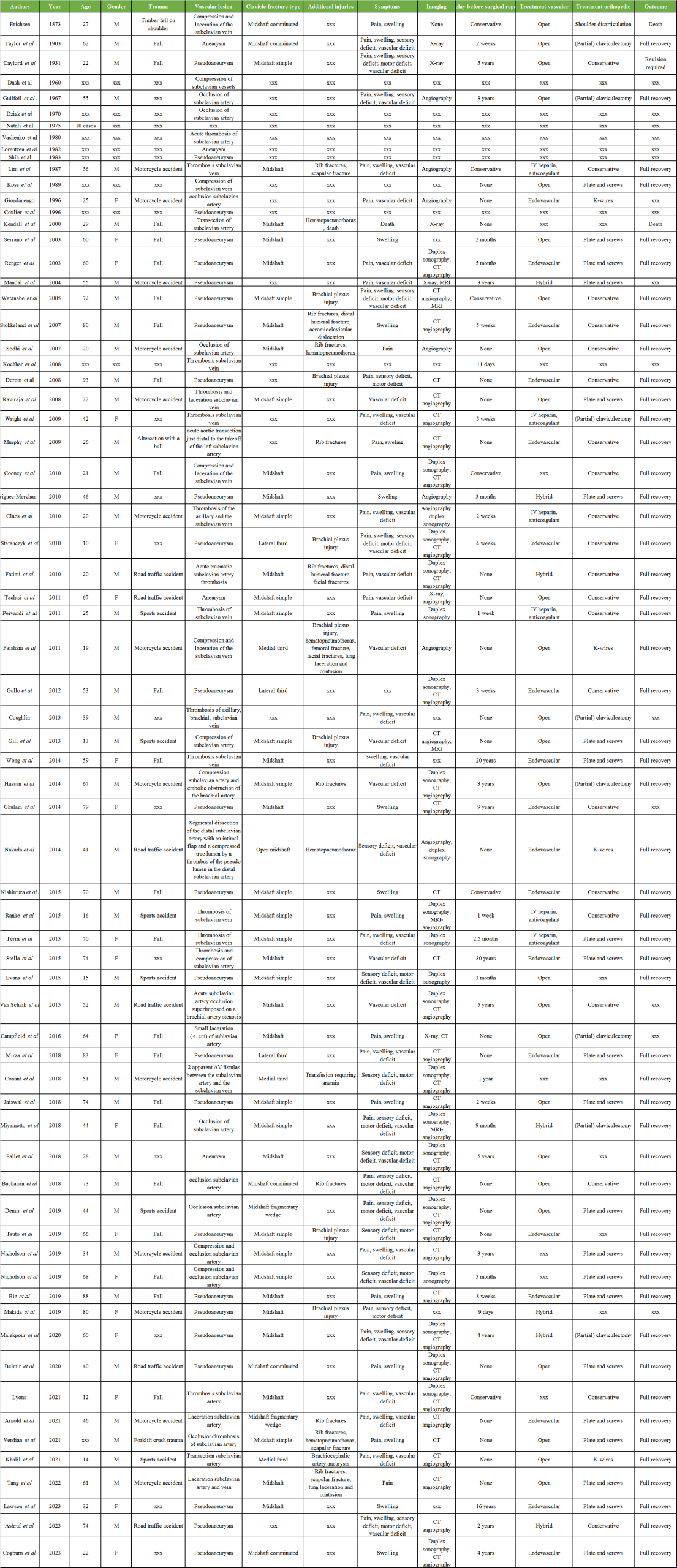
Table 1: Clavicular fracture with subclavian artery lesion.
Of these cases, 41 (51.9%) were male, 20 (25.3%) were female, and in 18 (22.8%) cases, gender was not specified. Trauma mechanisms were road traffic accidents (24.1%) cases resulted from road traffic accidents, sports injuries (8.9%), fall from height (27.8%), crush trauma at work (2.5%), or not specified (36.7%). Open clavicular fracture was present in 1.2%.
Conservative treatment of the lesion of the subclavian artery was initiated in 46 cases (58.9%), but later conversion to medical treatment of the vascular lesion was necessary in 34 (43.0%) cases due to secondary thrombosis, occlusion, (pseudo)aneurysm, or arterial compression from fracture callus formation.
Typically, the subclavian artery lesion is treated first, and different approaches are possible.
Endovascular repair is preferred as it is a minimally invasive treatment. The brachial artery offers a direct and short route to the injury site. Alternatively, the femoral approach can be used [5]. Endovascular repair is only indicated if the vessel is partially damaged, allowing a guide wire to pass beyond the injury, followed by a covered stent to seal the defect. Up to 80% of subclavian and axillary artery injuries can be treated endovascularly, resulting in reduced blood loss, shorter operating times, lower in-hospital mortality, and decreased hospital stays [5,6]. Five-year patency rates for covered stents in the subclavian artery exceed 80% [7]. However, there is a risk of intimal hyperplasia and later occlusion, which can be managed postoperatively, where long-term results of endovascular therapy for subclavian artery lesions are excellent [8,9]. A potential drawback is the risk of occluding the vertebral artery, which can be challenging to identify in an acute setting.
A hybrid approach has been described, with balloon occlusion for proximal control bleeding, followed by open repair [10]. The indication for a hybrid endovascular and open approach is to establish proximal bleeding control with an occlusive balloon, followed by open inspection of the vessel wall. This is usually done in cases when imaging indicates a partially or fully transected vessel, which might compromise the success of an endovascular-only approach. The hybrid technique allows for controlled dissection in a non-actively bleeding field, minimizing trauma to adjacent structures and facilitating detailed inspection and reconstruction of the vessel wall [10].
An open approach is necessary when dealing with a complete subclavian artery transection [11]. Furthermore, associated neurological or vascular lesion is typically an indication for surgical exploration and stabilization of the clavicular fracture [12]. In these cases, the clavicle fracture can be used as a window to expose the underlying subclavian vessels. Younger patients may also benefit from the open approach, where long-term patency is a primary concern.
Full recovery without any complications was reported in 52 cases (65.8%). Revision surgery was required in 1 (1.2%) case. 2 (2.5%) patients lost their affected upper limb and died shortly after.
Clavicle fractures can be treated conservatively depending on the location, displacement, and comminution of the fracture. Open fractures or fractures with compromised skin are strict indications for surgery.
Plate and screw osteosynthesis is most commonly used because it allows anatomical reconstruction of the fracture and solid fixation. This is probably preferable to minimize motion and possible compression at the vascular repair site. The availability of pre-contoured anatomical plates that fit the clavicle’s natural curve allows precise fracture reduction. Dynamic compression plates apply pressure at the fracture site to encourage faster healing, while locking plates are particularly useful in osteoporotic and comminuted fractures, providing extra stability. Both superior and anteroinferior placement of the plate and screw osteosynthesis have been described. Superior plating has traditionally been favored because it provides fixation on the tension side of the fracture. However, complications such as hardware prominence and concerns about screw trajectory angles, which could risk the subclavian artery, have led to increased interest in anteroinferior plating. Interfragmentary screws and cerclage wires can augment the stability of the construct [13-16].
Alternatively, clavicle fractures can be stabilized by inserting a rod or pin into the bone’s medullary canal. This is a less invasive option with minimal soft tissue disruption and is especially effective for simple, displaced midshaft fractures. However, intramedullary nailing allows some motion at the fracture and the vascular repair site and has specific possible complications, including pin extrusion and skin irritation [13-16].
Healthcare workers that are involved in the treatment of clavicle fractures must be aware that these can be associated with a lesion of the subclavian artery. Clinical symptoms can be subtle, and in case of doubt, computed tomography angiography is advised to make a correct diagnosis. An open surgical approach for these combined lesions has several advantages: The clavicle fracture provides a window to the subclavian artery for repair. Surgical stabilization of the fracture with plate and screws prevents inadvertent motion or compression of the fracture fragments on the vascular repair and allows early mobilization. Plate designs for anteroinferior placement on the clavicle have a lower chance of iatrogenic laceration of the vascular repair. According to the literature, a good outcome in our case can be expected.
Clinicians should maintain a high index of suspicion for subclavian artery injury in patients with clavicle fractures, especially when vascular signs are subtle, as early diagnosis and combined surgical management of both the fracture and vascular lesion are crucial for optimal outcomes.








