Both adductor canal block and local infiltration analgesia significantly decreased VAS scores compared to standard multimodal analgesia. Local infiltration analgesia showed the lowest pain scores and delayed opioid requirements.
Dr. Arnav P Rathod, Department of Orthopedics, Dr. Panjabrao Deshmukh Memorial Medical College Hospital, Amravati, Maharashtra, India. E-mail: rarnav95@yahoo.in
Introduction: Effective post-operative pain management is crucial for early mobilization and improved outcomes following total knee arthroplasty (TKA). Multimodal analgesia (MMA) strategies, such as the adductor canal block (ACB) and local infiltration analgesia (LIA) with liposomal bupivacaine, have been developed to enhance pain relief and minimize opioid consumption.
Objectives: The aim of this study was to compare the efficacy of standard MMA alone with MMA in combination with ACB or LIA in patients undergoing TKA.
Materials and Methods: A prospective comparative study involving 90 patients undergoing unilateral TKA, who were divided equally into three groups: Group A (standard MMA), Group B (MMA + ACB), and Group C (MMA + LIA). Post-operative pain was measured using the visual analog scale (VAS) at 6, 12, 24, and 48 h. Secondary outcomes included opioid consumption and the study of adverse effects.
Results: Both ACB and LIA significantly decreased VAS scores compared to standard MMA (P < 0.001). Group C (LIA) showed the lowest pain scores, delayed opioid requirements. Opioid consumption and the incidence of side effects were significantly lower in Groups B and C, with Group C exhibiting the most favorable profile.
Conclusion: Both ACB and LIA are effective in improving analgesia and reducing opioid use following TKA. LIA with liposomal bupivacaine provided the most sustained pain relief supporting its use in enhanced recovery protocols.
Keywords: Total knee arthroplasty, multimodal analgesia, adductor canal block, local infiltration analgesia, post-operative pain.
Total knee arthroplasty (TKA) is one of the most commonly performed orthopedic surgeries worldwide, primarily recommended for patients with advanced osteoarthritis and various degenerative joint conditions. While TKA significantly improves joint function and quality of life, it often results in considerable post-operative pain. This pain can hinder early movement, delay rehabilitation, and negatively impact patient satisfaction and overall outcomes [1,2].
Effective pain management following surgery is crucial for recovery in TKA. Conventionally, pain relief methods have relied heavily on opioid medications. However, the use of opioids can lead to adverse side effects, such as nausea, vomiting, sedation, constipation, respiratory depression, and even addiction, highlighting the need for safer and more effective alternatives [3,4].
In recent years, multimodal analgesia (MMA) has become the standard of care. This approach involves employing various pharmacological and regional techniques that work together to target different pain pathways. The goal is to reduce opioid use while still providing adequate pain relief. Among the promising methods included in MMA protocols are the adductor canal block (ACB) and local infiltration analgesia (LIA), especially when utilizing long-acting agents such as liposomal bupivacaine. These techniques have demonstrated potential in enhancing pain control and facilitating functional recovery [5,6].
Despite several available techniques, there remains a need to compare the effectiveness of these evolving strategies to find the best pain management approach for TKA. Therefore, this study aims to compare the analgesic efficacy, opioid-sparing potential, and side effects of three different MMA strategies: Standard pharmacologic MMA, MMA with ACB, and MMA with LIA using liposomal bupivacaine [7,8].
The aim of this study is to evaluate and compare the effectiveness of different innovative MMA strategies in managing post-operative pain following TKA.
Objectives
The aim of this study was to assess post-operative pain intensity using the visual analog scale (VAS) at various time intervals in patients receiving:
-
- Standard MMA
- MMA with ACB
- MMA with local LIA using liposomal bupivacaine.
Study design and setting
This prospective comparative study was conducted in the department of orthopedics at a tertiary care hospital.
Study population
Patients aged 50–75 years with American Society of Anesthesiologists physical status I–III undergoing primary unilateral TKA for osteoarthritis under spinal anesthesia were included, as unilateral TKAs are more commonly done at our institute. Exclusion criteria comprised known allergies to study drugs, coagulopathy or anticoagulant use, chronic opioid dependency, neurological deficits in the operative limb, and revision or bilateral TKA.
Sample size
A period-based study was conducted for a period of 12 months, where all the patients fitting in the inclusion criteria were enrolled, that is, 90 patients.
Sampling method and technique
All 90 eligible patients were enrolled and equally randomized into three groups (n = 30 each): Group A (standard MMA), Group B (MMA + ACB), and Group C (MMA + LIA) through convenience sampling technique.
Methodology
All patients received spinal anesthesia with 0.5% hyperbaric bupivacaine, and TKA was performed using a standardized technique by anesthetist. Post-operative analgesia protocols were as follows:
- Group A (MMA): Paracetamol 1 g intravenous (IV) every 8 h, diclofenac 75 mg IV every 12 h, and gabapentin 300 mg orally at bedtime.
- Group B (MMA + ACB): MMA plus an ACB with 20 mL of 0.25% bupivacaine.
- Group C (MMA + LIA): MMA plus LIA with liposomal bupivacaine (266 mg in 20 mL saline). Rescue analgesia (IV morphine) was administered if the VAS score was ≥4, with the dose and time recorded.
For group B ultrasound-guided approach was used for ACB
Patient was laid in supine position, thigh slightly externally rotated. High-frequency linear ultrasound placed at mid-thigh, just below the inguinal crease, to visualize the femoral artery within the canal. The femoral artery was identified, surrounded medially by the sartorius muscle and laterally by the vastus medialis. Under sterile conditions, a needle in-plane from lateral to medial was inserted, traversing beneath the sartorius muscle. The needle tip was placed adjacent to the femoral artery region, using hydro-dissection (small saline injection). Aspiration was done to exclude intravascular placement. 20 mL of 0.25% bupivacaine isobaric solution was injected.
Outcome measures
- Primary outcome: Post-operative pain intensity was assessed using the VAS (0–10 scale) at 6, 12, 24, and 48 h.
- Secondary outcomes included total opioid consumption (morphine equivalent dose in mg) within 48 h and incidence of adverse effects (nausea, vomiting, and sedation).
Statistical analysis
Data were analyzed using one-way analysis of variance for continuous variables (VAS scores, opioid consumption) and Chi-square tests for categorical variables (adverse effects). P < 0.05 was considered statistically significant.
A total of 90 patients were enrolled and randomized into three groups (n = 30 each). Baseline demographics, including age (mean: 65.4 ± 6.2 years in Group A, 64.8 ± 5.9 in Group B, 65.1 ± 6.5 in Group C; P = 0.88) and sex distribution (male: female ratio: 0.6:1 in Group A, 0.7:1 in Group B, 0.8:1 in Group C; P = 0.79), showed no significant differences across groups (Table 1).
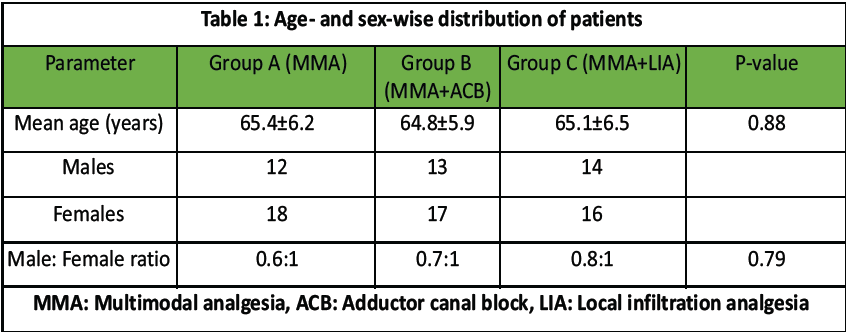
Table 1: Age- and sex-wise distribution of patients
Preoperatively, no statistical significance in the VAS score was seen in three groups. Post-operative pain, assessed through the VAS, was significantly lower in Groups B (MMA + ACB) and C (MMA + LIA) compared to Group A (MMA) at all-time points (P < 0.001). Group C exhibited the lowest VAS scores, with means of 2.9 ± 0.7 at 6 h, 2.3 ± 0.6 at 12 h, 1.6 ± 0.5 at 24 h, and 1.1 ± 0.3 at 48 h, compared to 4.7 ± 1.2, 4.2 ± 1.0, 3.8 ± 0.9, and 3.1 ± 0.7 in Group A, respectively (Table 2).
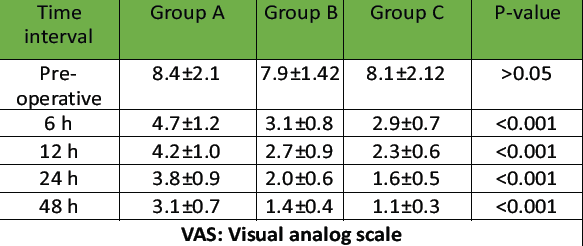
Table 2: Pain assessment by VAS scores
In our study, no statistically significant differences with respect to age, sex, and other sociodemographic profiles were observed. Opioid consumption (morphine equivalent dose) within 48 h was highest in Group A (29.5 ± 5.8 mg), followed by Group B (18.1 ± 4.3 mg), and lowest in Group C (12.3 ± 3.0 mg; P < 0.001) (Table 3). Adverse effects were more frequent in Group A, with nausea in 8 patients (26.7%), vomiting in 5 (16.7%), and sedation in 4 (13.3%), compared to Group C, which had nausea in 2 (6.7%), vomiting in 1 (3.3%), and no sedation (P < 0.05 for all) (Table 4).
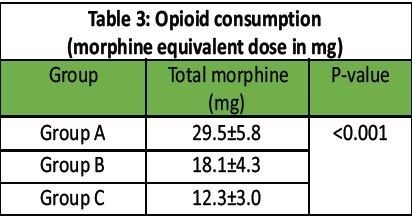
Table 3: Opioid consumption (morphine equivalent dose in mg)
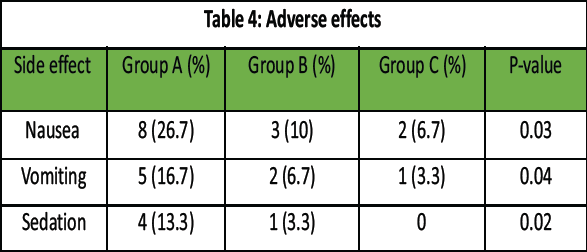
Table 4: Adverse effects
In this study, both ACB and LIA using liposomal bupivacaine significantly outperformed standard MMA alone in controlling post-operative pain, reducing opioid requirements, and improving patient satisfaction after TKA. Group C (LIA) exhibited the lowest VAS scores (e.g., 1.1 ± 0.3 at 48 h) and opioid consumption (12.3 ± 3.0 mg morphine equivalents), alongside the fewest side effects (Table 4).
These results align with findings from Koh et al., who reported that ACB provides effective analgesia while preserving quadriceps motor strength, facilitating early ambulation and rehabilitation [9]. Similarly, Jaeger et al., emphasized the benefit of ACB over femoral nerve block, noting its selective sensory blockade and reduced motor impairment [10].
Regarding LIA, our results support previous evidence from Kerr and Kohan, who introduced the concept of local infiltration using a mixture of local anesthetics, opioids, and anti-inflammatories, showing improved pain scores and faster recovery [11]. More recently, Mont et al., conducted a multicenter trial demonstrating that LIA with liposomal bupivacaine reduced opioid use and pain scores significantly reduced as compared to conventional bupivacaine [12].
Opioid consumption was markedly reduced in both ACB and LIA groups, with the lowest use in the LIA group. This is particularly significant in light of the opioid epidemic, reinforcing findings from Gandhi et al., who highlighted the role of regional techniques in minimizing opioid-related complications [13]. The lower incidence of nausea, vomiting, and sedation in our intervention groups further supports a shift toward opioid-sparing protocols.
While the reduction in opioid consumption in the ACB and LIA groups (18.1 mg and 12.3 mg morphine equivalents, respectively, compared to 29.5 mg in the MMA group) is promising, opioid use still poses risks such as dependency and side effects such as nausea and sedation, as observed in our study (Table 4). These findings underscore the need for vigilant drug monitoring in the post-operative period. Safer alternatives, such as extended-release non-opioid analgesics (e.g., acetaminophen or non-steroidal anti-inflammatory drugs) or adjuvant therapies such as cryotherapy and transcutaneous electrical nerve stimulation, could further reduce opioid reliance.
Limitations and future direction
- The sample size of 90 patients, while sufficient for detecting significant differences in VAS scores and opioid consumption, may limit the generalizability of our findings. Future studies with larger cohorts are warranted to confirm these results.
- The assessment period was limited to 48 h post-surgery, which may not fully capture the pain trajectory leading up to discharge (typically day 3–5). Future studies should extend the evaluation period to better assess the impact of these analgesia techniques on the entire perioperative recovery phase.
LIA with liposomal bupivacaine and ACB significantly improve post-operative pain control and reduce opioid use compared to standard MMA in TKA. LIA offers the most sustained relief and fewest side effects, supporting its integration into enhanced recovery protocols. Future research should focus on larger sample sizes, extended assessment periods, and safer opioid-sparing strategies to optimize outcomes.
ACB and LIA both markedly enhance pain control compared to MMA alone. It preserves motor strength while providing effective sensory analgesia. Intra-articular with liposomal bupivacaine delivers sustained analgesia and opioid-sparing benefit.
References
- 1. Bromley PA, Williams DM. Multimodal analgesia in total knee arthroplasty: An overview of current practices. Orthop Clin North Am 2018;49:563-73. [Google Scholar] [PubMed]
- 2. Chaudhuri S, Richards SH. Efficacy of adductor canal block in total knee arthroplasty: A systematic review and meta-analysis. Br J Anaesth 2020;124:206-15. [Google Scholar] [PubMed]
- 3. Grob M, Ackermann P. Comparing the effects of liposomal bupivacaine in local infiltration analgesia for knee surgery: A randomized controlled trial. J Arthroplasty 2022;37:1122-30. [Google Scholar] [PubMed]
- 4. Kurtz SM, Lau E. Multimodal pain management in orthopedic surgery: The role of nerve blocks and local anesthetics. Clin Orthop Relat Res 2019;477:1751-63. [Google Scholar] [PubMed]
- 5. Kehlet H, Jensen TS. The role of multimodal analgesia in improving recovery after TKA: A review of current literature. Pain Med 2021;22:267-76. [Google Scholar] [PubMed]
- 6. Marlowe DS, Brown KM. Innovations in regional anesthesia: The future of postoperative pain control in TKA. J Clin Anesth 2020;63:110-7. [Google Scholar] [PubMed]
- 7. Sarton E, Dahan A. The impact of opioid-sparing techniques in orthopedic surgery: A focus on multimodal analgesia in TKA. Pain Manage Nurs 2019;20:268-75. [Google Scholar] [PubMed]
- 8. Tighe CB, Smith ME. Opioid reduction in total knee arthroplasty through innovative pain management strategies: A comparison of efficacy and safety. J Bone Joint Surg 2020;102:1051-9. [Google Scholar] [PubMed]
- 9. Koh IJ, Chang CB, Lee JH, Jeon YT, Kim TK. Preemptive adductor canal block for ambulatory total knee arthroplasty: A randomized, double-blind, placebo-controlled study. J Arthroplasty 2014;29:2348-53. [Google Scholar] [PubMed]
- 10. Jaeger P, Zaric D, Fomsgaard JS, Hilsted KL, Bjerregaard J, Gyrn J, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: A randomized, double-blind study. Anesth Analg 2013;116:1373-80. [Google Scholar] [PubMed]
- 11. Kerr DR, Kohan L. Local infiltration analgesia: A technique for the control of acute postoperative pain following knee and hip surgery. Clin Orthop Relat Res 2008;466:1443-52. [Google Scholar] [PubMed]
- 12. Mont MA, Beaver WB, Dysart SH, Barrington JW, Del Gaizo DJ. Local infiltration analgesia with liposomal bupivacaine improves pain scores and reduces opioid use after total knee arthroplasty: Results of a randomized controlled trial. J Arthroplasty 2018;33:90-6. [Google Scholar] [PubMed]
- 13. Gandhi K, Viscusi ER, Schwenk ES, Buvanendran A. Reducing opioid use for patients undergoing total knee arthroplasty. Reg Anesth Pain Med 2017;42:527-36. [Google Scholar] [PubMed]