Retrograde intramedullary nailing provides faster fracture healing and earlier mobilization with better functional outcomes compared to antegrade nailing in distal femur fractures, though it may increase the risk of anterior knee pain.
Dr. Ismail Pandor, Department of Orthopedics, Krishna Vishwa Vidhyapeeth, Karad, Maharashtra, India. E-mail: I.pandor07@gmail.com
Background: Distal femur fractures, though uncommon, present treatment challenges due to patient variability and fracture complexity. Various fixation methods exist, but there is no consensus on the optimal approach. This study compares clinical and functional outcomes of antegrade versus retrograde intramedullary nailing in distal femur fractures.
Materials and Methods: A prospective observational study of 60 patients with extra-articular distal femur fractures was conducted. Patients were alternately assigned to antegrade (n = 30) or retrograde (n = 30) nailing groups. Outcomes assessed included operative time, radiological union, knee range of motion (ROM), weight-bearing milestones, complications, and functional outcomes using Neer’s scoring system. Statistical analysis compared results between groups.
Results: Retrograde nailing showed significantly shorter operative times (85 ± 2.15 min vs. 95 ± 1.39 min), faster radiological union (10 ± 0.38 weeks vs. 14 ± 0.44 weeks), earlier partial (9.27 ± 0.37 weeks vs. 10.9 ± 0.49 weeks), and full weight bearing (15 ± 0.47 weeks vs. 18.2 ± 0.67 weeks) and slightly better knee ROM (117.3° ± 2° vs. 114.4° ± 1.8°) compared to antegrade nailing (P < 0.05). Functional outcomes were superior in the retrograde group, with 67.7% excellent scores versus 26.7% in the antegrade group. Retrograde nailing had more cases of anterior knee pain, while antegrade nailing was associated with higher rates of hip pain, infections, and delayed union.
Conclusion: Retrograde intramedullary nailing offers advantages in surgical efficiency, fracture healing, and early mobilization, making it a reliable option for managing distal femur fractures. However, attention to anterior knee pain is warranted. Further large-scale studies are recommended to confirm long-term outcomes.
Keywords: Distal femur fracture, retrograde femur nailing, antegrade femur nailing.
Distal femur fractures are relatively uncommon, with an incidence of 37/100,000 people annually [1], accounting for around 0.4% of all adult fractures [2]. These injuries typically occur through two distinct mechanisms: Low-energy trauma in elderly patients with osteoporotic bone and poor soft tissue quality and high-energy trauma in younger individuals. Approximately 30% of these fractures are associated with polytrauma. Various treatment options exist, including conventional plate osteosynthesis, biological plating, and intramedullary nailing through antegrade or retrograde approaches. While biological plating has reduced complications compared to traditional plating [3], intramedullary nailing, particularly through the antegrade route, has demonstrated high union rates and excellent functional outcomes [4]. Despite advances in surgical techniques, there is still no clear consensus on the optimal fixation method for distal femur fractures, particularly in specific patient populations such as the elderly or polytrauma cases. Each modality has advantages and limitations, and long-term functional outcomes, complication rates, and healing times vary. Furthermore, while retrograde nailing has shown promising results, its comparative effectiveness to other techniques in varied clinical scenarios remains insufficiently studied. These uncertainties highlight a significant gap in the current understanding of how to best manage distal femur fractures for optimal recovery. Given the lack of consensus on the most effective fixation method for distal femur fractures, this study aims to evaluate and compare clinical and functional outcomes of current treatment modalities, with a particular focus on retrograde intramedullary nailing. By addressing the existing knowledge gap, we aim to contribute data that could inform treatment decisions and optimize patient outcomes across different age groups and injury profiles.
This is a prospective comparative observational study of 60 patients with distal femoral fractures conducted at Krishna Institute of Medical Sciences, Karad, from 2020 to 2022 after acquiring permission from the ethics committee. The sample size of 60 patients was determined based on the number of eligible cases presenting during the study period from 2020 to 2022. All patients meeting the inclusion and exclusion criteria were consecutively enrolled and alternatively assigned to either antegrade or retrograde nailing groups. A formal sample size calculation was not performed due to the observational nature and resource limitations of the study. Patients presenting with extra-articular fractures of the distal 15 cm of femur were selected for the study. Thirty patients were managed with retrograde nailing and other 30 were managed with antegrade nailing. Data were obtained from patients after acquiring consent. After the procedure, the patients were evaluated for weight bearing, fracture union, and knee flexion at 1, 5, 3, and 6 months. Functional outcome was measured using Neer’s scoring system which evaluates pain, walking capacity, joint movements, work capacity, gross anatomy, and radiographic appearance. The system assigns a maximum of 100 points—70 for functional components and 30 for anatomical and radiological findings. Based on the total score, outcomes are categorized as excellent (>85), good (70–85), fair (55–69), or poor (<55) [5] (Table 1).
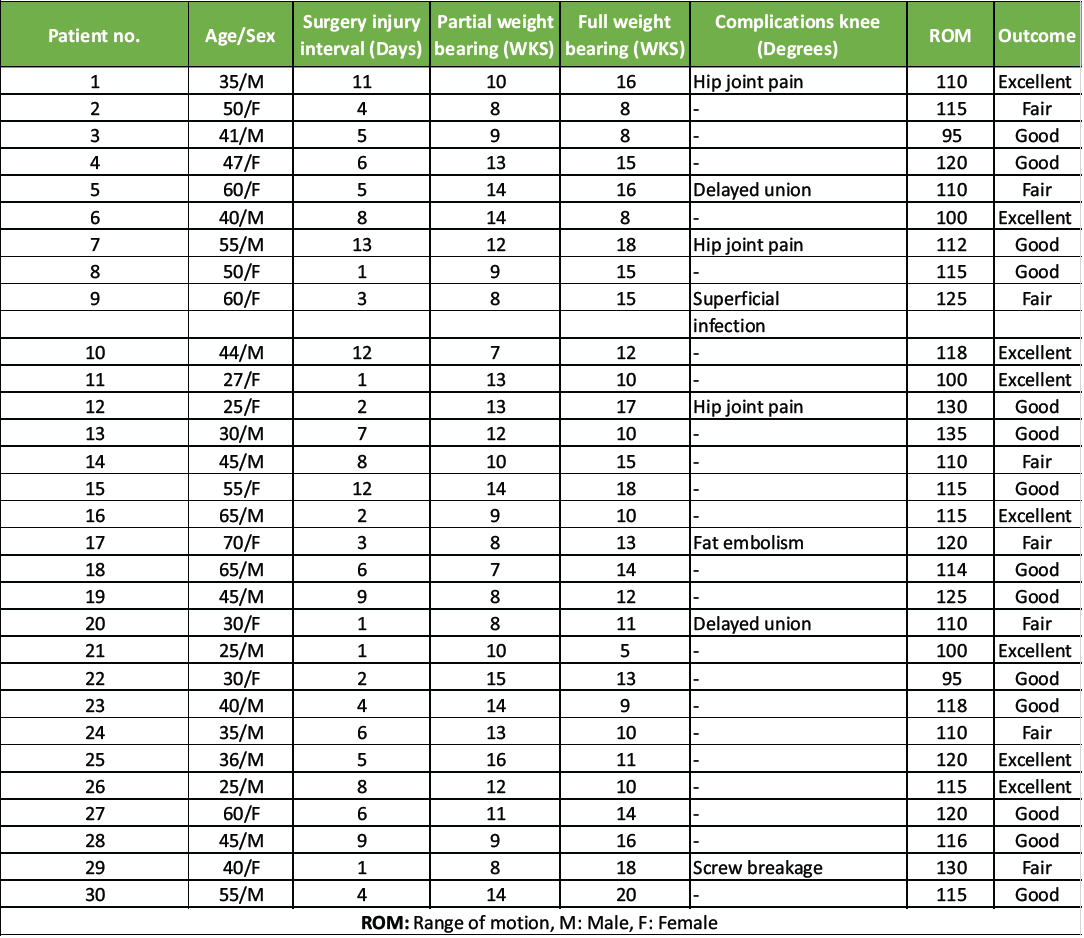
Table 1: Results of antegrade femur nailing
Patients above 18 years of age of any sex presenting with extra-articular distal femur fractures classified as AO Type A, involving the distal 15 cm of the femur, and who were willing to undergo surgical intervention, were included in the study. Patients were excluded if they were below 18 years of age, had intra-articular fractures classified as AO Type B or C, or sustained compound fractures classified as Gustilo-Anderson Type II or III.
Operative procedure
For antegrade nailing, under spinal anesthesia, the patient is placed in the lateral position. A fracture table was used. An extension shoe was used for the traction of the fractured limb; a femoral distractor or Steinmann pin was utilized if it was necessary. C-arm was used to confirm the reduction. An incision was placed 7 cm proximal to the greater trochanter. The greater trochanter was palpated and through piriformis fossa, a guide wire was inserted whose position was confirmed on the C-arm. After preparing the medullary canal, the reamer guide and nail guide were passed across the fracture site. Reaming was done. The canal was over reamed by 0.5–1 mm greater than the nail used. The uniplanar antegrade femur nail was mounted on a targeting device and was inserted. Position of the nail was confirmed by fluoroscopy in anteroposterior (AP) and lateral views. Two distal and two proximal 4.9 mm cortical screws were inserted. A suction drain was inserted and wound was closed in layers.
Above-knee 90–90 slab was given postoperatively. Drains were removed on post-operative day 2. Active and passive movements were begun.
For retrograde nailing, under spinal anesthesia, the patient is placed in the supine position with slight knee flexion (20–50°) with the help of a bump under the knee. Medial parapatellar arthrotomy was done to approach the intercondylar notch. Another approach tried was the patellar tendon splitting approach. The insertion point anterior to Blumensaat’s line was localized using AP and lateral views. Bone awl was inserted at the localized point. Guide wire was inserted and fracture reduction was achieved by traction and manipulation. Minimal reaming was done and a nail of largest possible diameter was introduced in the medullary canal. We used uniplanar supracondylar nails in this study with a maximum length of 30 cm and minimum length of 15 cm. The length of nail used was determined by the distance of fracture line from the articular surface and the fracture pattern. This was followed by distal locking with 6.5 mm fully threaded cancellous screws using a targeting device. Finally, proximal locking using 4.9 mm self-tapping cortical screws was done. Physiotherapy and post-operative mobilization were begun from post-operative day 3. Patients were followed up regularly for radiological and clinical union. Post-operative rehabilitation included initiation of active and passive knee range of motion (ROM) exercises from post-operative day 3. Partial weight bearing was allowed based on radiological signs of union, progressing to full weight bearing by 10–18 weeks. Data were collected prospectively and entered into Microsoft Excel. Statistical analysis was performed using the Statistical Package for the Social Sciences software. Continuous variables (e.g., time to union, ROM) were expressed as mean ± standard deviation and compared using the Student’s t-test. Categorical variables (e.g., complications, outcomes) were analyzed using the Chi-square test. A P < 0.05 was considered statistically significant.
Implants and instruments
In the present study, we used uniplanar antegrade femur nailing system (Fig. 1) and uniplanar retrograde femur nailing system (Fig. 2).

Figure 1: Pre-operative anteroposterior and lateral views showing a distal third fracture of femur.
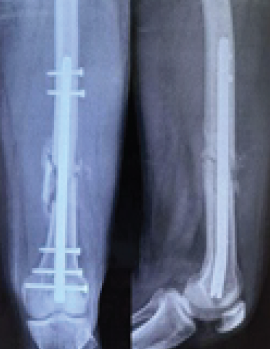
Figure 2: Anteroposterior and lateral views at 1.5 months showing distal third fracture of the femur with retrograde nail.
Out of 60 study subjects in the present study, 15 (25%) patients were in the age group of 21–30 years, 16 (26.7%) were in the age group of 31–40 years, 12 (20%) were in the age group of 41–50 years, 12 (20%) in the age group of 51–60 years, and 5 (8.3%) patients in the age group 61–70. According to gender, 35 (58%) patients were male and 25 (42%) patients were female. In 36 patients of the study had road traffic accident (RTA), making it the leading cause of injury. 36 patients in the study had RTA. 12 patients had fall from height, domestic injury group had 9 patients, and sports-related injuries in 3 patients (Table 2).
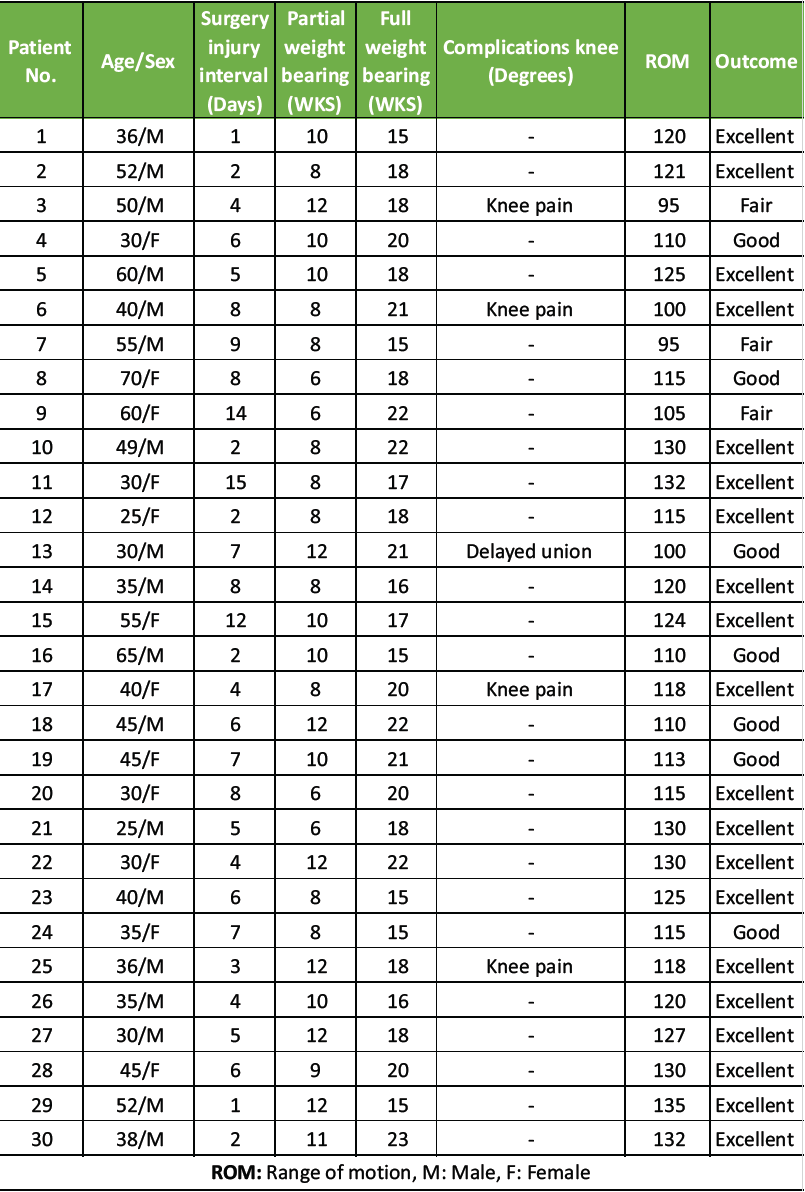
Table 2: Results of retrograde nailing
Out of all study participants, 58 patients had closed fractures and rest 2 patients had compound fractures. The mean operation-injury interval was 5.5 ± 0.67 days for antegrade nailing and 5.8 ± 0.65 days for retrograde nailing. The mean duration of the surgery was 85 ± 2.15 min for retrograde nailing and 95 ± 1.39 min for antegrade nailing. Mean time for radiological union with retrograde nailing was 10 ± 0.38 weeks (Fig. 1, 2, 3, 4) and with antegrade nailing, it was 14 0.44 weeks (Fig. 5, 6).
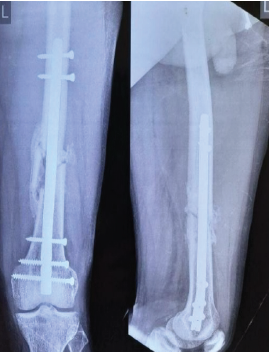
Figure 3: Anteroposterior and lateral views at 3 months showing distal third fracture of femur with retrograde nail.
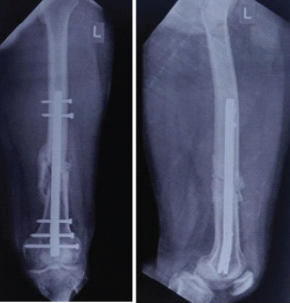
Figure 4: Anteroposterior and lateral views at 6 months showing distal third fracture of the femur with retrograde nail.
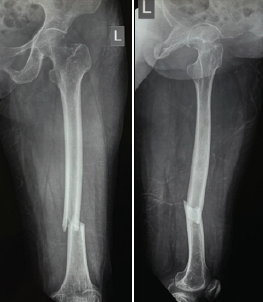
Figure 5: Pre-operative anteroposterior and lateral views showing a distal third fracture of the femur.

Figure 6: Anteroposterior and lateral views at 1.5 months showing distal third fracture of femur with an antegrade nail.

Figure 7: Anteroposterior and lateral views at 3 months showing distal third fracture of femur with an antegrade nail.

Figure 8: Anteroposterior and lateral views at 6 months showing distal third fracture of the femur with antegrade nail.
The mean post-operative knee ROM achieved with retrograde nailing was 117.3 ±2° and with antegrade nailing, it was 114.4 ± 1.8°. Mean time for partial weight bearing was 9.27 ± 0.37 weeks with retrograde nailing, an 10.9 ± 0.49 weeks in antegrade nailing. Mean time for full weight bearing was 15 ± 0.47 weeks in retrograde nailing and 18.2 ± 0.67 weeks in antegrade nailing (Tables 3, 4, 5).
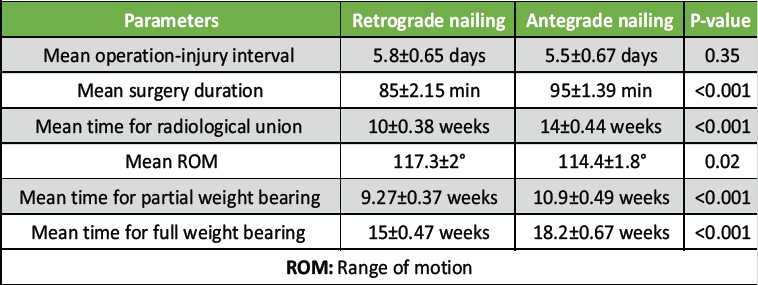
Table 3: Comparison of results of antegrade and retrograde nailing
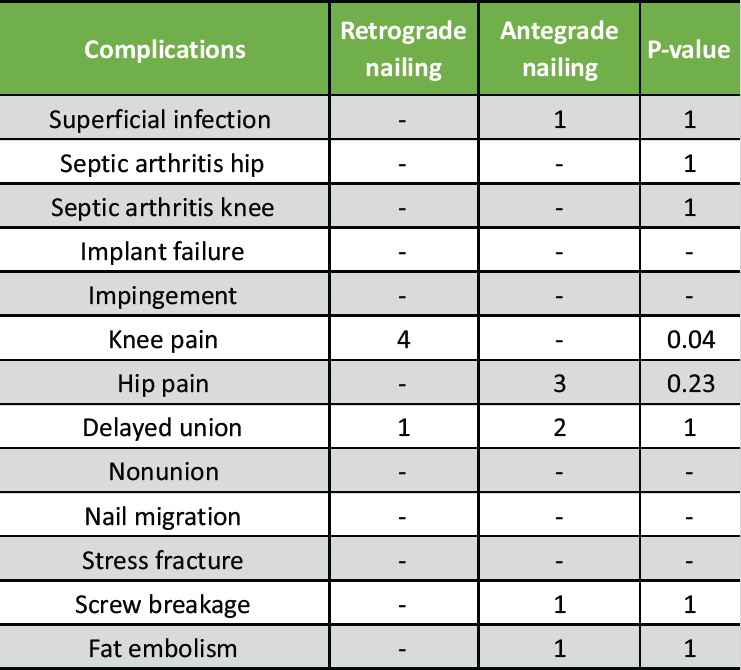
Table 4: Comparison of complications between antegrade and retrograde nailing
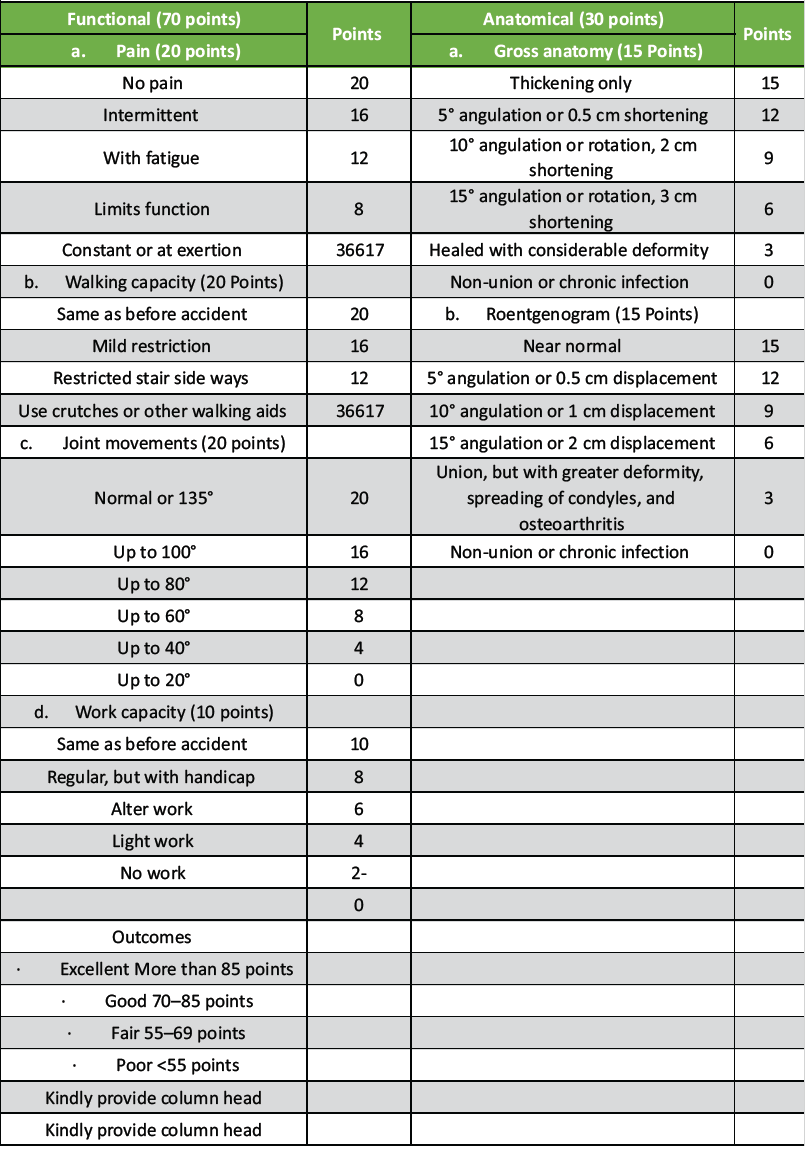
Table 5: Neer’s scoring system
As per Neers’ scoring system in the retrograde nailing group, 20 (67.7%) had excellent outcome, 7 (23.3%) had good outcome, and 3 (10%) had fair outcome. In antegrade nailing group, 8 (26.7%) had excellent outcomes, 15 (50%) had good outcome, and 7 (23.3%) had fair outcome.
Complications were observed in 8 patients with antegrade nailing. Three patients had hip joint pain, for which two were re-operated on for implant removal after fracture had healed. One patient had a superficial infection during the treatment and one patient had fat embolism. Two patients managed with antegrade nailing had delayed union. With retrograde femoral nailing, four patients complained of knee pain postoperatively and one patient had delayed union of the fracture. Delayed union was defined as failure to reach bony union by 6-month post-injury (Table 6).
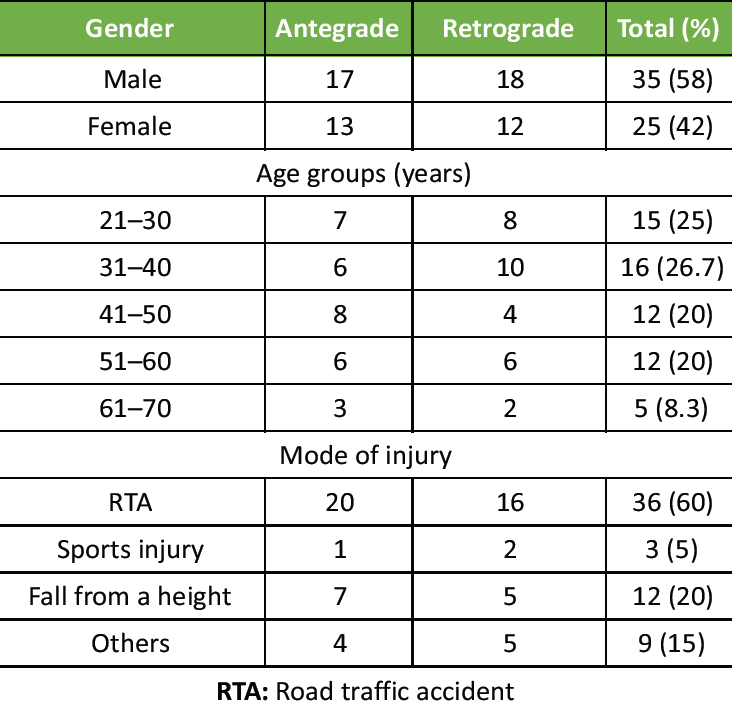
Table 6: Patient demographics
This study compared antegrade and retrograde femoral nailing techniques for femoral fractures, focusing on clinical outcomes and complications. Our results showed that retrograde nailing had shorter operative time, faster fracture healing, and earlier weight-bearing compared to antegrade nailing. These findings correspond with recent literature indicating that retrograde nailing can be more efficient due to easier surgical access and reduced soft tissue disruption [6,5].
The significantly shorter radiological union time in the retrograde group aligns with studies demonstrating enhanced biological preservation around the fracture site, which promotes faster healing [7]. However, antegrade nailing remains preferred for certain fracture locations, especially proximal femoral fractures, because of better mechanical alignment and stability [8]. Our results regarding ROM suggest a slight functional advantage in the retrograde group, echoing findings by Park et al., who reported improved knee joint mobility following retrograde nailing [9].
Early partial and full weight-bearing in the retrograde group further supports its role in accelerated rehabilitation, consistent with protocols highlighted by Chen et al. [6]. However, the retrograde approach was also associated with a higher incidence of anterior knee pain, a known complication linked to the distal entry point and potential cartilage irritation [10]. Antegrade nailing showed higher rates of superficial infection and implant-related complications, potentially due to more extensive soft tissue manipulation near the hip region [11].
Comparing these results with international studies, the benefits of retrograde nailing in terms of operative efficiency and fracture healing are well-supported [6,5]. However, variations in patient demographics, surgical techniques, and implant types may explain differences in complication rates reported across studies. National studies focusing on specific fracture patterns also recommend tailoring the approach based on fracture location and patient factors [8].
The study’s limitations include a relatively small sample size and short follow-up duration, limiting assessment of long-term functional outcomes and complications. Moreover, patient-reported outcome measures such as pain scores and quality of life were not captured, which future prospective studies should incorporate. Further randomized controlled trials with larger cohorts and longer follow-up are essential to confirm these findings and optimize surgical strategies, particularly in reducing anterior knee pain after retrograde nailing.
This study demonstrates that retrograde intramedullary nailing is an effective treatment for distal femur fractures, providing good clinical and functional outcomes. Our results support its use as a reliable option across different patient groups. However, further large-scale studies are needed to confirm long-term benefits and optimize treatment guidelines.
Retrograde intramedullary nailing is a safe and effective method for managing distal femur fractures, offering favorable functional outcomes and reliable fracture healing. It should be considered a viable treatment option, especially in patients where biological fixation and early mobilization are priorities.
References
- 1. Arneson TJ, Melton LJ 3rd, Lewallen DG, O’Fallon WM. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965-1984. Clin Orthop Relat Res 1988;234:188-94. [Google Scholar] [PubMed]
- 2. Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury 2006;37:691-7. [Google Scholar] [PubMed]
- 3. Della Torre P, Aglietti P, Altissimi M. Results of rigid fixation in 54 supracondylar fractures of the femur. Arch Orthop Trauma Surg (1978) 1980;97:177-83. [Google Scholar] [PubMed]
- 4. Winquist R, Hansen S Jr., Clawson DK. Closed intramedullary nailing of femoral fractures. J Bone Joint Surg Am 1984;66:529-39. [Google Scholar] [PubMed]
- 5. Daher M, Tarchichi J, Zalaquett Z, Casey JC, Ghanimeh J, Mansour J. Antegrade vs Retrograde Intra-Medullary Nailing in Femoral Shaft Fractures: A Systematic Review and Meta-Analysis. Arch Bone Jt Surg. 2024;12(8):535-545.. [Google Scholar] [PubMed]
- 6. Chen L, Yuanhe Fan, Jie Chen and Hongliang Tu et al. Early weight-bearing after retrograde femoral nailing: A prospective cohort study. J Orthop Surg 2023;31:215-22. [Google Scholar] [PubMed]
- 7. Zhao H, Deng X, Liu W, Chen W, Wang L, Zhang Y et al. Biological factors influencing femoral fracture healing: A review. Bone Joint Res 2020;9:870-9. [Google Scholar] [PubMed]
- 8. Martinez RS, Konda SR,Gales J,Leucht P, Egol KA et al. Fracture location dictates approach: Antegrade vs retrograde nailing in femoral fractures. Eur J Trauma Emerg Surg 2022;48:1447-54. [Google Scholar] [PubMed]
- 9. Park SJ, Kim JH ,Lee SW ,Choi YJ, Han CW et al. Functional outcomes following retrograde femoral nailing: A systematic review. J Clin Orthop 2021;45:30-7. [Google Scholar] [PubMed]
- 10. Singh D, Kumar A, Sharma V ,Gupta R,Mehta N et al. Anterior knee pain after retrograde femoral nailing: Pathophysiology and prevention. Int Orthop 2020;44:2617-24. [Google Scholar] [PubMed]
- 11. Thakur M, Patel R,Singh A,Verma S, Choudhary A. et al. Complication rates in antegrade femoral nailing: A retrospective analysis. Trauma Surg Acute Care Open 2019;4:e000253. [Google Scholar] [PubMed]











