Patients with lumbar radiculopathies due to disc herniation or degenerative disc disease demonstrated significant pain relief, with reduced VAS scores during follow-up compared to baseline.
Satvik Muralidhar, Department of Orthopedics, MM Institute of Medical Sciences and Research, Mullana, Ambala, Haryana, India. E-mail: satuchess@gmail.com
Introduction: Lower back pain, a leading cause of global disability, is commonly attributed to lumbar disc herniation (LDH) and lumbar degenerative disc disease (LDDD). These conditions result in nerve inflammation and compression, causing significant pain and mobility limitations. Epidural steroid injections (ESIs) are a minimally invasive treatment targeting inflammation to provide pain relief and improve functionality.
Objective: This study aimed to evaluate the short-term efficacy of ESIs in patients with LDH and LDDD, analyze Visual Analog Scale (VAS) pain scores over time, and assess factors influencing treatment outcomes.
Methods: A prospective study of 50 patients with lumbar radiculopathy due to LDH or LDDD was conducted between November 2022 and November 2024. Inclusion criteria comprised adults (>18 years) with radicular pain unresponsive to conservative treatments. Demographics, medical history, radiculopathy levels, and VAS scores were recorded at baseline and during follow-ups at 3 and 6 months. Statistical analyses evaluated differences based on diagnosis, gender, body mass index (BMI), and radiculopathy levels.
Results: The cohort (mean age 47 years) included 66% males and 34% females. LDH accounted for 76% of cases, and LDDD for 24%. Significant pain reduction was observed post-injection (VAS scores from ~7 to ~4 at 3 months). However, symptoms partially recurred by 6 months (VAS ~5.5). No significant differences in outcomes were noted across gender, BMI, or radiculopathy levels (P > 0.05).
Conclusion: ESIs effectively reduce pain in LDH and LDDD patients during short-term follow-ups. However, symptom recurrence indicates the need for sustained management strategies. While ESIs offer temporary relief, their integration into a comprehensive treatment plan is essential for optimizing long-term outcomes.
Keywords: lumbar disc herniation, degenerative disc disease, epidural steroid injections, radiculopathy, Visual Analog Scale, pain management.
Lower back pain is a common cause of disability globally, affecting millions and posing significant challenges to individuals’ quality of life. Among the most prevalent sources of chronic back pain are lumbar disc herniation (LDH) and lumbar degenerative disc disease (LDDD). These conditions often involve inflammation and irritation of the spinal nerves, leading to debilitating pain, numbness, or weakness that can radiate into the legs [1]. Epidural steroid injections (ESIs) are a minimally invasive treatment option widely used to manage this type of pain. By delivering corticosteroids directly into the epidural space, ESIs aim to reduce inflammation and relieve symptoms, thereby improving the patient’s functionality and overall well-being [2].
LDH occurs when the inner gel-like portion of an intervertebral disc pushes through its tougher outer layer. This herniation can press against nearby spinal nerves, leading to a range of symptoms, including sharp pain in the lower back and legs, often referred to as sciatica [3]. On the other hand, LDDD is characterized by the gradual breakdown of the intervertebral discs due to aging or wear and tear. This condition can cause chronic lower back pain and nerve irritation as the discs lose their ability to cushion the vertebrae. Both conditions are associated with inflammatory processes and mechanical compression, making them prime candidates for treatments that target inflammation, such as ESIs [4].
The procedure for an ESI involves administering corticosteroids, often combined with a local anesthetic, into the epidural space around the spinal cord and nerve roots. This is done under precise imaging guidance, such as fluoroscopy, to ensure the medication is delivered to the affected area. The injection works by reducing swelling and irritation around the compressed nerves, providing pain relief that can last for weeks or even months. While ESIs do not address the underlying structural issues, they can significantly alleviate symptoms, allowing patients to engage more effectively in other forms of therapy, such as physical rehabilitation [5].
ESIs are typically recommended for patients who experience persistent back or leg pain that has not improved with conservative treatments, such as physical therapy, rest, or medication. They are particularly effective for managing radicular pain caused by nerve root compression due to herniated discs [6]. In addition, they are commonly used for chronic pain resulting from degenerative disc disease (DDD), spinal stenosis, and certain post-surgical pain syndromes. By targeting the site of nerve inflammation, ESIs help break the cycle of pain and inflammation, offering a much-needed reprieve for patients dealing with these debilitating conditions [7].
The benefits of ESIs extend beyond immediate pain relief. By reducing inflammation, they enable patients to regain mobility and participate in daily activities with greater ease. This can also help patients engage in physical therapy programs that strengthen the spine and improve overall function. Furthermore, ESIs may serve as an alternative to more invasive treatments, such as surgery, for some patients, especially when used as part of a comprehensive treatment plan. However, it is important to note that the duration and extent of relief can vary among individuals. While some may experience long-lasting benefits, others may find only short-term improvement [8].
ESIs, like any medical intervention, are not without risks, though they are generally considered safe when performed by experienced practitioners. Minor complications can include localized infection or bleeding at the injection site, which are rare but manageable [9]. More serious complications, though infrequent, may include nerve damage or accidental puncture of the spinal dura mater, the protective covering of the spinal cord. This puncture can lead to cerebrospinal fluid leakage, potentially causing severe headaches, known as post-dural puncture headaches. Patients with pre-existing medical conditions, such as diabetes, should also be aware that corticosteroids can temporarily elevate blood sugar levels, necessitating close monitoring. Other potential side effects include facial flushing, temporary weight gain, and insomnia, although these are less common [10].
Despite these risks, ESIs remain a valuable option in the management of LDH and DDD. While they do not cure the underlying structural abnormalities, ESIs provide targeted pain relief by reducing inflammation at the nerve root, often offering patients a window of relief that can last weeks or months. This temporary respite is significant, as it allows individuals to engage in complementary treatments such as physical therapy, which strengthens the spine and improves overall functionality. Moreover, ESIs can play a crucial role in behavioral interventions for chronic pain management, helping patients develop coping strategies and improve their mental well-being [11].
The integrative nature of ESIs is central to their effectiveness. They are often combined with pharmacological treatments, such as anti-inflammatory drugs or muscle relaxants, to enhance pain control. When used as part of a multidisciplinary approach, ESIs can optimize patient outcomes by providing immediate relief while supporting longer-term strategies that improve mobility, quality of life, and overall health [12]. Such a holistic approach typically yields better results than relying on any single treatment method. ESIs are a valuable tool in the management of pain associated with LDH and DDD. They provide an effective means of reducing inflammation and alleviating pain, allowing patients to improve their mobility and quality of life. While not a standalone solution, they are a key component of modern non-surgical treatment plans for spine-related disorders. With careful patient selection and a comprehensive approach to care, ESIs can significantly enhance the outcomes for individuals dealing with these challenging conditions [13].
The purpose of this study is to determine the efficacy of ESIs during short-term follow-up for patients with LDH or LDDD, as well as to identify the specific timing and factors that contribute to the progression of these conditions.
This prospective study reviewed 50 patients treated for lumbar radiculopathies with epidural spinal injections and spinal surgery over 2 years (November 2022 to November 2024). Ethical approval has been obtained from the ethical approval committee to conduct the study. Inclusion criteria included patients above 18 years of age experiencing lumbar radicular pain secondary to disc herniation or DDD. Data collected included patient demographics, surgical history, duration of radiculopathy, details of ESIs (type and frequency), spine surgery, and Visual Analog Scale (VAS) scores. Assessments were completed at baseline and followed up for up to 6 months to evaluate treatment efficacy and progression of symptoms.
The average age of participants was 47 years, ranging from 30 to 78 years. The gender distribution showed that 66% were male and 34% were female. Radiculopathy was caused by disc herniation in 76% of the patients, whereas 24% had radiculopathy secondary to DDD (Table 1).
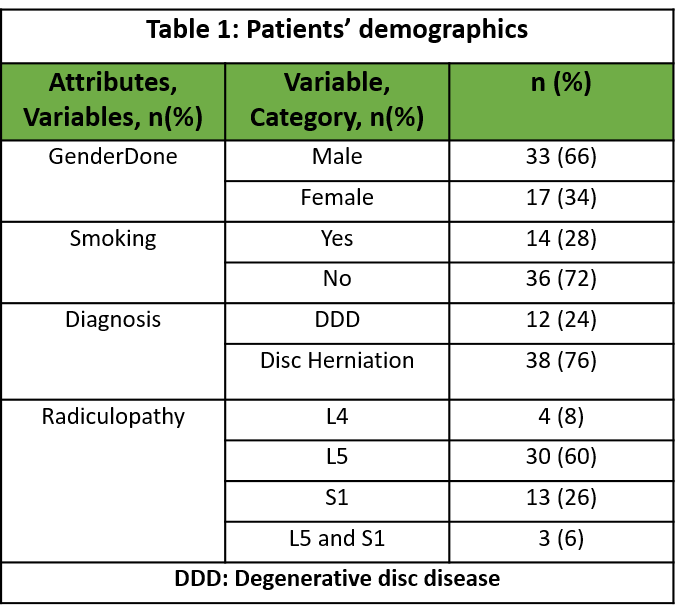
Table 1: Patients’ demographics
The table summarizes demographic and clinical characteristics. Of 50 patients, 66% are male, and 34% are female. Smoking prevalence is 28%. Diagnoses include 24% with DDD and 76% with disc herniation. Radiculopathy affects L4 (8%), L5 (60%), S1 (26%), and L5-S1 combined (6%), highlighting L5 as the most common site (Fig. 1).
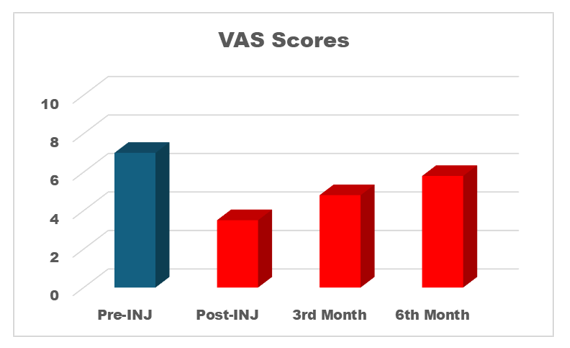
Figure 1: Visual Analog Scale scores.
The VAS scores show a decrease in pain levels following an intervention. Pre-injection (Pre-INJ) scores were the highest at around 7. Post-injection scores dropped significantly to 4. At the 3rd month, scores slightly increased to about 5, and by the 6th month, they stabilized at 6, indicating a gradual return of symptoms over time (Table 2).
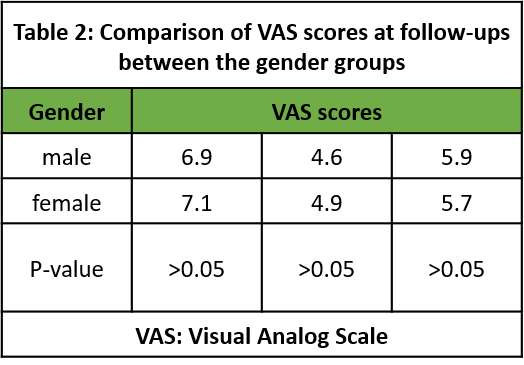
Table 2: Comparison of VAS scores at follow-ups between the gender groups
The table compares VAS scores between males and females at 3 time points: Baseline, post-injection, and follow-up. Males had scores of 6.9, 4.6, and 5.9, whereas females scored 7.1, 4.9, and 5.7. The P-values (>0.05) indicate no statistically significant difference in pain reduction between genders, suggesting similar treatment responses over time (Table 3).
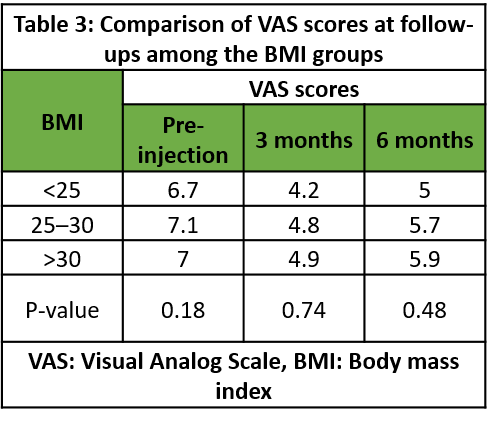
Table 3: Comparison of VAS scores at follow-ups among the BMI groups
The table compares VAS scores across body mass index (BMI) categories at Pre-INJ, 3 months, and 6 months. Patients with BMI <25, 25–30, and >30 showed similar trends, with scores decreasing initially and slightly increasing by 6 months. No statistically significant differences were observed (P > 0.05), suggesting that BMI does not significantly influence pain reduction following the intervention (Table 4).
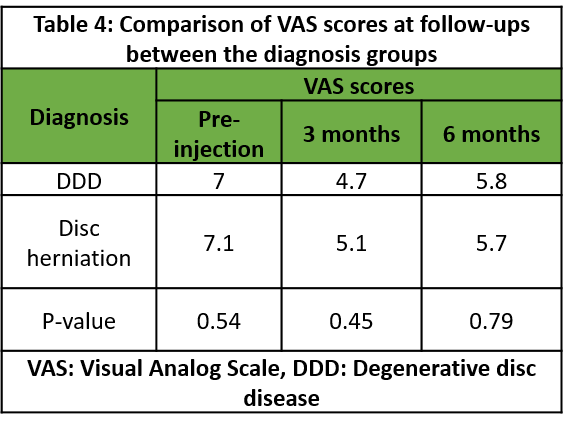
Table 4: Comparison of VAS scores at follow-ups between the diagnosis groups
The table compares VAS scores between patients with DDD and disc herniation at Pre-INJ, 3 months, and 6 months. Both groups showed pain reduction, with scores stabilizing by 6 months. The P-values (>0.05) indicate no statistically significant difference between the groups, suggesting similar treatment responses irrespective of diagnosis (Table 5).
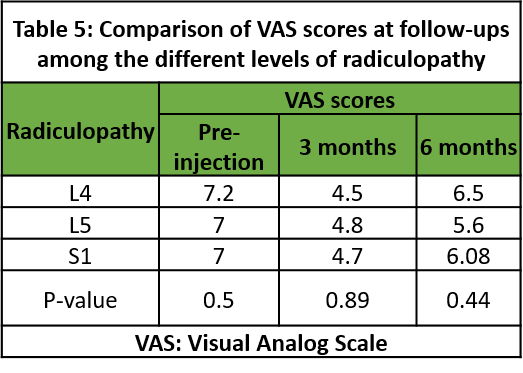
Table 5: Comparison of VAS scores at follow-ups among the different levels of radiculopathy
The table compares VAS scores among L4, L5, and S1 radiculopathy groups. All groups showed pain reduction at 3 months, followed by a slight increase at 6 months. The P-values (>0.05) indicate no statistically significant differences between the groups, suggesting similar treatment outcomes regardless of radiculopathy location (Table 6).
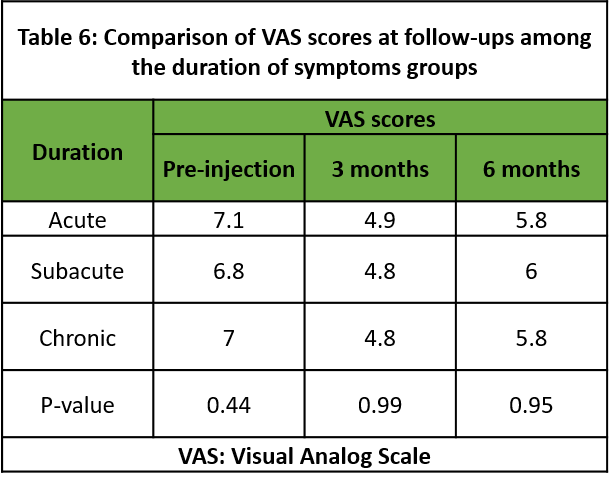
Table 6: Comparison of VAS scores at follow-ups among the duration of symptoms groups
The table compares VAS scores across acute, subacute, and chronic pain durations. All groups show significant pain reduction at 3 months, with a slight increase at 6 months. The P-values (>0.05) indicate no statistically significant differences between groups, suggesting similar responses to treatment regardless of pain duration.
Lower back pain is a leading cause of disability worldwide, significantly impacting quality of life. LDH and LDDD are common causes, involving nerve irritation and inflammation. ESIs offer a minimally invasive treatment option by delivering corticosteroids to reduce inflammation and provide targeted pain relief. LDH results from the inner disc material protruding through its outer layer, compressing nearby spinal nerves and causing radiating pain. DDD, caused by aging or wear and tear, results in chronic back pain due to loss of disc cushioning. Though ESIs do not address structural abnormalities, they provide temporary relief, enabling participation in rehabilitation therapies. This study aims to evaluate the short-term efficacy of ESIs for managing LDH and LDDD and identify factors influencing condition progression. [14]
Our findings align with Çetin Sr et al. and Radcliff et al. in highlighting demographic and clinical characteristics. Both studies report a male predominance in disc conditions, with pain duration often exceeding three months. Neurological deficits and Lasegue positivity are consistent findings, whereas BMI and comorbidities show no significant variation. Radcliff et al. additionally emphasized differences in treatment preferences and depression rates. These shared insights validate the relevance of our results within the broader clinical context [15,16].
Our findings correlate with Lee et al. (2018) and Carassiti et al. (2021), showing significant short-term pain relief post-ESIs (VAS decrease from 7 to 4). Similar to these studies, pain reduction was most effective within 1 month but diminished over time, with scores rising at 3 and 6 months, reflecting symptom recurrence. Both studies highlight steroids’ efficacy for short-term relief, with diminishing long-term benefits influenced by patient-specific factors and pathology, consistent with our observed trends [17,18].
Our findings align with Gautschi et al. and Triebel et al., showing no significant gender differences in VAS scores post-intervention (P > 0.05). Similar to Gautschi’s study, gender-based differences in pre-treatment pain levels did not translate into differing post-operative outcomes. Triebel’s study further supports comparable long-term improvements, despite initial slower progress in women. These findings collectively highlight that gender does not significantly impact pain reduction or recovery trajectories following interventions, consistent with our observed treatment responses [19,20].
Our findings align with Çetin Sr et al. and Stienen et al. (2016), showing significant VAS score reductions across follow-up periods regardless of BMI categories. Çetin’s study highlights greater pain reduction in disc protrusion cases, whereas BMI-specific data were not analyzed. Stienen observed a positive correlation between BMI and baseline back pain, yet our study and these findings suggest BMI does not significantly influence long-term pain reduction trends, underscoring comparable treatment responses across BMI groups [15,21].
Both Buttermann (2018) and Chang et al. (2015) found that surgical interventions for cervical spine disorders, whether via ACDF or arthroplasty, yield significant improvements in neck and arm pain regardless of underlying pathology. Buttermann’s study showed equivalent reductions in VAS scores for patients with HNP, stenosis, and DDD after ACDF, whereas Chang’s work demonstrated similarly favorable outcomes in cervical arthroplasty for traumatic herniation and DDD. Neither author observed significant differences between diagnostic groups, suggesting comparable clinical benefits across various cervical spine conditions [22,23].
Our study correlates with findings by Khan et al. and Cyteval et al., emphasizing the effectiveness of treatment in reducing pain across radiculopathy levels. Initial VAS (8.01 ± 0.90) reduced significantly at 6 weeks (2.80 ± 0.40) but increased slightly at 3 months (3.50 ± 0.70), stabilizing by 6 months (3.97 ± 0.40). Khan et al. reported varying responses across radiculopathy levels, with the highest “Excellent” outcomes at L3 and L4 levels, whereas Cyteval et al. observed similar trends across S1 levels. These findings collectively suggest consistent treatment outcomes with variations based on radiculopathy location and follow-up timing [24,25].
Our study correlates with findings by Karabis et al. and Breivika et al. (2016), highlighting the effectiveness of VAS in assessing pain relief over time. In rheumatoid arthritis and osteoarthritis patients, early VAS pain reductions strongly predicted long-term outcomes, demonstrating significant relief by 2 and 6 weeks of treatment, as noted by Karabis et al. Breivika et al. emphasized VAS’s utility in acute pain scenarios while advocating for multidimensional approaches to better evaluate chronic pain’s complexity. Together, these studies underscore the importance of VAS in tracking treatment efficacy and the need for comprehensive assessments in chronic pain cases [26,27].
Patients with lumbar radiculopathies due to disc herniation or DDD demonstrated significant pain relief, with reduced VAS scores during follow-up compared to baseline. However, a trend of increasing VAS scores over time was observed, indicating a partial recurrence of symptoms. This suggests that while initial treatment effectively alleviates pain, the benefits may diminish during the follow-up period. The findings highlight the need for ongoing evaluation and tailored strategies to sustain long-term pain relief and improve patient outcomes. Continuous monitoring remains crucial to address the recurrence of symptoms and optimize treatment efficacy over time.
Patients with lumbar radiculopathies due to disc herniation or degenerative disc disease demonstrated significant pain relief, with reduced VAS scores during follow-up compared to baseline. However, a trend of increasing VAS scores over time was observed, indicating a partial recurrence of symptoms. This suggests that while initial treatment effectively alleviates pain, the benefits may diminish during the follow-up period. The findings highlight the need for ongoing evaluation and tailored strategies to sustain long-term pain relief and improve patient outcomes. Continuous monitoring remains crucial to address the recurrence of symptoms and optimize treatment efficacy over time.
References
- 1. Froud R, Patterson S, Eldridge S, Seale C, Pincus T, Rajendran D, et al. A systematic review and meta-synthesis of the impact of low back pain on people’s lives. BMC Musculoskelet Disord 2014;15:50. [Google Scholar] [PubMed]
- 2. Bicket MC, Chakravarthy K, Chang D, Cohen SP. Epidural steroid injections: An updated review on recent trends in safety and complications. Pain Manag 2015;5:129-46. [Google Scholar] [PubMed]
- 3. Patel S, Kumar S, Soni A, Acharya S, Acharya N. Lumbar disc disease: An overview. In: Mechanism and Genetic Susceptibility of Neurological Disorders. New York: Springer; 2024. p. 391-417. [Google Scholar] [PubMed]
- 4. Elsaka O, Noureldean MA, Gamil MA, Ghazali MT, Abd Al-Razik AH, Hisham D. Pathophysiology, investigations and operative management in cases of lumbar degenerative disc disease. Asian Basic Appl Res J 2022;4:44-65. [Google Scholar] [PubMed]
- 5. Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: A comprehensive, evidence-based review. Reg Anesth Pain Med 2013;38:175-200. [Google Scholar] [PubMed]
- 6. Chou R, Hashimoto R, Friedly J, Fu R, Bougatsos C, Dana T, et al. Epidural corticosteroid injections for radiculopathy and spinal stenosis: A systematic review and meta-analysis. Ann Intern Med 2015;163:373-81. [Google Scholar] [PubMed]
- 7. Alshammari HS, Alshammari AS, Alshammari SA, Ahamed SS. Prevalence of chronic pain after spinal surgery: A systematic review and meta-analysis. Cureus 2023;15:e41841. [Google Scholar] [PubMed]
- 8. Epstein NE. The risks of epidural and transforaminal steroid injections in the spine: Commentary and a comprehensive review of the literature. Surg Neurol Int 2013;4(Suppl 2):S74-93. [Google Scholar] [PubMed]
- 9. Delaney FT, MacMahon PJ. An update on epidural steroid injections: Is there still a role for particulate corticosteroids? Skeletal Radiol 2023;52:1863-71. [Google Scholar] [PubMed]
- 10. Doelakeh ES, Chandak A. Risk factors in administering spinal anesthesia: A comprehensive review. Cureus 2023;15:e49886. [Google Scholar] [PubMed]
- 11. Beall DP, Kim KD, Macadaeg K, Donboli K, Chauhan K, Sowlay M, et al. Treatment gaps and emerging therapies in lumbar disc herniation. Pain Physician 2024;27:401-3. [Google Scholar] [PubMed]
- 12. Natera D, Romero KJ, Curcio JC, Montalvo VV, Navarro FM, Imran M, et al. Interventional management of low back pain: A comprehensive review of epidural steroid injections and related techniques. J Anest Inten Care Med 2024;13:555864. [Google Scholar] [PubMed]
- 13. Boisen ML, Fernando RJ, Alfaras-Melainis K, Hoffmann PJ, Kolarczyk LM, Teeter E, et al. The year in thoracic anesthesia: Selected highlights from 2021. J Cardiothorac Vasc Anesth 2022;36:4252-65. [Google Scholar] [PubMed]
- 14. Li W, Djuric N, Vleggeert-Lankamp CL. A systematic review evaluating the association of atherosclerosis and lumbar degenerative disc disease. Brain Spine 2024;4:103901. [Google Scholar] [PubMed]
- 15. Çetin E Sr., Şah V, Zengin I, Arabacı Ö, Akyol ME, Yücel M. Comparative effectiveness of epidural steroid injections in patients with disc bulging and disc protrusion. Cureus 2023;15:e45334. [Google Scholar] [PubMed]
- 16. Radcliff K, Hilibrand A, Lurie JD, Tosteson TD, Delasotta L, Rihn J, et al. The impact of epidural steroid injections on the outcomes of patients treated for lumbar disc herniation: A subgroup analysis of the SPORT trial. J Bone Joint Surg Am 2012;94:1353-8. [Google Scholar] [PubMed]
- 17. Lee JH, Kim DH, Kim DH, Shin KH, Park SJ, Lee GJ, et al. Comparison of clinical efficacy of epidural injection with or without steroid in lumbosacral disc herniation: A systematic review and meta-analysis. Pain Physician 2018;21:449-68. [Google Scholar] [PubMed]
- 18. Carassiti M, Pascarella G, Strumia A, Russo F, Papalia GF, Cataldo R, et al. Epidural steroid injections for low back pain: A narrative review. Int J Environ Res Public Health 2021;19:231. [Google Scholar] [PubMed]
- 19. Gautschi OP, Corniola MV, Smoll NR, Joswig H, Schaller K, Hildebrandt G, et al. Sex differences in subjective and objective measures of pain, functional impairment, and health-related quality of life in patients with lumbar degenerative disc disease. Pain 2016;157:1065-71. [Google Scholar] [PubMed]
- 20. Triebel J, Snellman G, Sandén B, Strömqvist F, Robinson Y. Women do not fare worse than men after lumbar fusion surgery: Two-year follow-up results from 4,780 prospectively collected patients in the Swedish National Spine Register with lumbar degenerative disc disease and chronic low back pain. Spine J 2017;17:656-62. [Google Scholar] [PubMed]
- 21. Stienen MN, Joswig H, Smoll NR, Corniola MV, Schaller K, Hildebrandt G, et al. Influence of body mass index on subjective and objective measures of pain, functional impairment, and health-related quality of life in lumbar degenerative disc disease. World Neurosurg 2016;96:570-7.e1. [Google Scholar] [PubMed]
- 22. Buttermann GR. Anterior cervical discectomy and fusion outcomes over 10 years: A prospective study. Spine (Phila Pa 1976) 2018;43:207-14. [Google Scholar] [PubMed]
- 23. Chang HK, Huang WC, Wu JC, Tu TH, Fay LY, Chang PY, et al. Cervical arthroplasty for traumatic disc herniation: An age- and sex-matched comparison with anterior cervical discectomy and fusion. BMC Musculoskelet Disord 2015;16:228. [Google Scholar] [PubMed]
- 24. Khan JM, Singh O, Muzaffar J. Outcome of transforaminal nerve root block injection for lumbar radiculopathy. Int J Orthop 2023;9:205-8. [Google Scholar] [PubMed]
- 25. Cyteval C, Fescquet N, Thomas E, Decoux E, Blotman F, Taourel P. Predictive factors of efficacy of periradicular corticosteroid injections for lumbar radiculopathy. AJNR Am J Neuroradiol 2006;27:978-82. [Google Scholar] [PubMed]
- 26. Karabis A, Nikolakopoulos S, Pandhi S, Papadimitropoulou K, Nixon R, Chaves RL, et al. High correlation of VAS pain scores after 2 and 6 weeks of treatment with VAS pain scores at 12 weeks in randomised controlled trials in rheumatoid arthritis and osteoarthritis: Meta-analysis and implications. Arthritis Res Ther 2016;18:73. [Google Scholar] [PubMed]
- 27. Breivika H. Fifty years on the Visual Analogue Scale (VAS) for pain-intensity is still good for acute pain. But multidimensional assessment is needed for chronic pain. Scand J Pain 2016;11:150-2. [Google Scholar] [PubMed]