Synovial chondromatosis, when presenting without characteristic calcifications, may closely resemble cystic or neoplastic lesions of the posterior knee, underscoring the need for a high index of suspicion, advanced imaging, and histopathological confirmation for accurate diagnosis and appropriate management.
Dr. Nitesh Gahlot, Department of Orthopaedics, All India Institute of Medical Sciences, Marudhar Industrial Area, 2nd Phase, M.I.A. 1st Phase, Basni, Jodhpur, Rajasthan 342005, India. E-mail: doc.nitesh@gmail.com
Introduction: Synovial chondromatosis (SC) is a rare, benign metaplastic disorder of the synovial membrane that typically presents with joint pain, swelling, and mechanical symptoms. Although the knee is the most frequently involved joint, diagnosis can be challenging in early or atypical cases, particularly when classical calcifications are absent on imaging.
Case Report: We present the case of a young adult male with a 1-year history of insidious onset posterior knee pain, without any antecedent trauma. Clinical examination revealed a full range of motion with no joint instability. Radiographs were inconclusive, showing only a faint opacity, while magnetic resonance imaging (MRI) demonstrated a well-defined, encapsulated lesion in the posterior compartment adjacent to the posterior cruciate ligament. A provisional diagnosis of a cystic or neoplastic lesion was considered. The patient underwent open surgical excision via a posterior approach. Intraoperatively, multiple cartilaginous loose bodies were found within the lesion. Histopathological evaluation confirmed the diagnosis of SC. The patient recovered uneventfully with complete resolution of symptoms and full functional restoration at final follow-up.
Conclusion: This case highlights an uncommon presentation of non-calcified SC mimicking a posterior cystic or soft-tissue tumor, emphasizing the importance of MRI and histopathological evaluation in cases with atypical imaging features to avoid misdiagnosis and ensure appropriate treatment.
Keywords: Synovial chondromatosis, knee joint, posterior cyst, magnetic resonance imaging, loose bodies.
Synovial chondromatosis (SC) is a rare, benign disorder affecting the synovial lining of joints, tendon sheaths, and bursae, potentially leading to significant joint dysfunction and disability. The condition was initially documented in the knee by Ambroise Paré in 1558. Later, in 1813, René Laennec provided a description of intra-articular loose bodies arising from the subsynovial layer [1]. Although any joint can be involved, such as metacarpophalangeal joints, temporomandibular joints (TMJs), distal radio-ulnar joints, and the hips, the knee is the most common with an occurrence rate 50–65% [2,3,4]. SC presents as the gradual, insidious onset of mono-articular joint discomfort and stiffness [5]. If the complaints are left untreated, they could lead to a reduction in movement range, effusions, crepitation, and eventually locking of the joint. The differential diagnosis associated with SC should include synovial hemangioma, pigmented villonodular synovitis (PVNS), synovial cyst, lipoma arborescence, and malignancies, such as synovial chondrosarcoma or synovial sarcoma [2]. The diagnosis suspected clinically is confirmed based on imaging modalities such as plain radiographs, ultrasound, computed tomography scans, and magnetic resonance imaging (MRI). The gold standard diagnostic method is MRI due to its superiority in enhancing soft-tissue contrast [6]. This case report describes the first known instance of SC in the knee, manifesting as a well-defined encapsulated lesion, with the patient presenting with pain in the popliteal fossa.
A young adult male in his late 20s presented with a 1-year history of popliteal fossa pain, which began insidiously and gradually worsened in severity. Despite receiving treatment from general practitioners, his symptoms persisted. The patient reported no history of trauma. On clinical examination, the knee exhibited full range of motion, with flexion and extension from 0° to 130°. The collateral and cruciate ligaments were stable, and no varus or valgus deformities were noted. Palpation revealed no localized increase in temperature or tenderness, and the distal neurovascular status was intact.
Investigations
Radiographs demonstrated a subtle radio-opaque circular shadow located just posterior to the tibial slope (Fig. 1). T2-weighted MRI imaging revealed a well-defined lesion with heterogeneous signal intensity, measuring 1.4 × 2.5 × 3 cm. The lesion was situated in the midline posterior compartment, anterior to the knee capsule, and in close proximity to the posterior cruciate ligament (PCL) (Fig. 2). The differential diagnoses included ganglion cyst, Baker’s cyst, parameniscal cyst, PVNS, lipoma arborescens, synovial hemangioma, early-stage SC, and soft-tissue neoplasms such as synovial sarcoma or chondrosarcoma. The patient underwent a computed tomography torso and chest radiograph, which revealed no evidence of primary malignancy or metastasis.

Figure 1: Plain radiograph of the knee showing a subtle radio-opaque circular shadow located just posterior to the tibial slope, suggestive of an intra-articular or para-articular lesion.

Figure 2: T2-weighted magnetic resonance image of the knee demonstrating a well-defined lesion with heterogeneous signal intensity. The lesion is located in the midline posterior compartment, anterior to the knee capsule, and closely abutting the posterior cruciate ligament.
Treatment
After detailed counseling regarding the nature of the lesion and treatment options, the patient consented to surgical intervention. A surgical approach was planned, and an open excisional biopsy was performed using a posterior reverse L-shaped incision (Burks-Schaffer approach) [7]. On posterior capsule opening, a 2.5 cm × 2.5 cm encapsulated mass was identified behind the PCL and was excised en bloc. The mass contained multiple white loose bodies, each approximately 5 mm in diameter (Fig. 3). Both the excised loose bodies and synovial tissue were sent for histopathological analysis. Histopathological examination identified nodules of hyaline cartilage with clustered chondrocytes, encased by synovial tissue of varying thickness, thereby confirming the diagnosis of SC (Fig. 4).
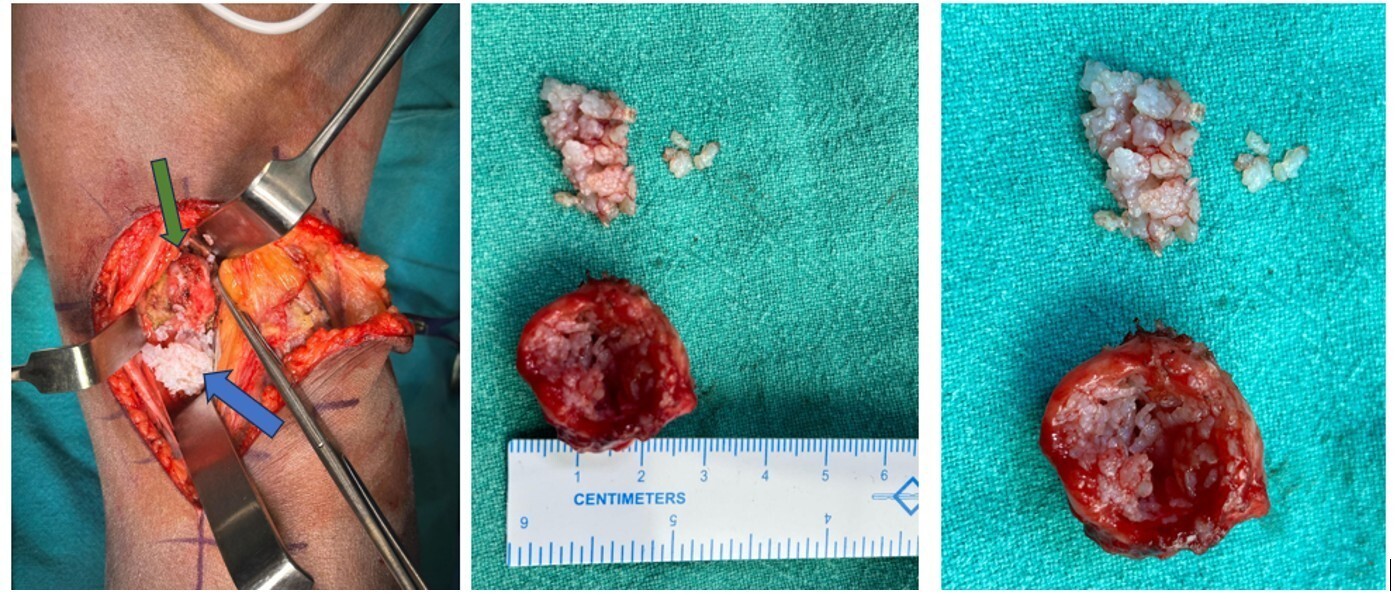
Figure 3: Intraoperative photograph showing a 2.5 cm × 2.5 cm encapsulated mass (green arrow) located behind the posterior cruciate ligament. The excised mass contains multiple white loose bodies (blue arrow).
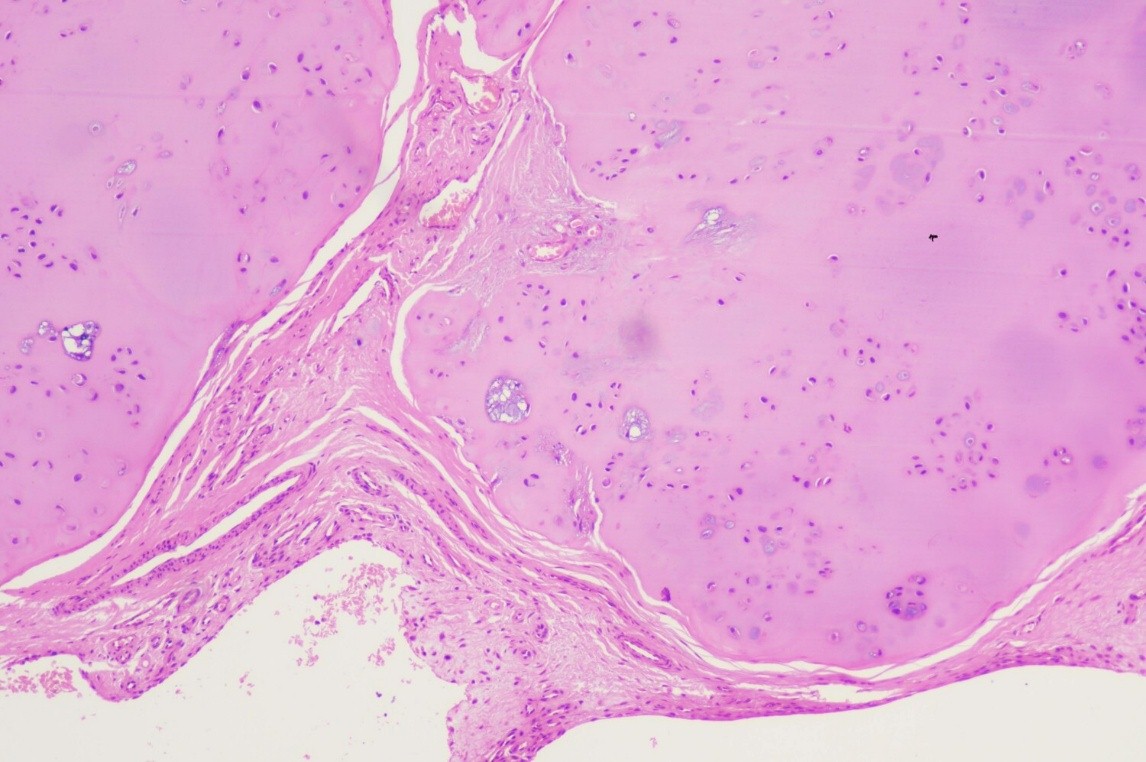
Figure 4: Histological section demonstrating nodules of hyaline cartilage with clustered chondrocytes, surrounded by synovial tissue of variable thickness, consistent with synovial chondromatosis (H&E stain, ×10).
Outcome and follow-up
Post-operative rehabilitation included weight bearing as tolerated, along with knee range-of-motion exercises and isometric quadriceps and hamstrings strengthening. The patient was followed up at 1, 3, and 6 months postoperatively. At the final 1½ year follow-up, the patient demonstrated an active knee flexion-extension range of 0°–130° without discomfort with full weight-bearing gait without support.
The patient achieved a Lysholm knee score of 95/100, an IKDC subjective knee evaluation score of 92/100, and a WOMAC score of 6/96, indicating excellent post-operative recovery with minimal residual symptoms and full functional restoration.
SC is the metaplastic process of synovium, which converts it into the cartilage and gets detached to become a loose body [8]. SC is typically classified according to its usual progression through three stages as described by Milgram in 1977. In phase I, metaplasia of the synovial intima occurs. Active synovitis and nodule formation are present, but no calcifications can be identified. In Phase II, these nodules detach from the synovium to become loose bodies within the joint. The loose bodies are primarily still cartilaginous. In the first two stages, plain radiographs will show no gross abnormalities of the affected joint. Phase III is characterized by multiple loose bodies within the joint space, with none remaining within the synovial tissue lining. Synovitis has typically resolved at this phase of the disease. It is at this stage that multiple intra- or extra-articular opaque loose bodies of various sizes are typically demonstrated as the loose bodies have calcified [9]. Earlier Jang et al., in their case series on SC of the TMJ, noted that over 80% of the patients’ exhibited calcifications [10]. Imaging plays a crucial role in the diagnosis of SC, with calcifications being present in standard radiographic examination in 70–95% of cases. Thus, in cases where plain radiography cannot demonstrate calcification or ossification, MRI is particularly useful [11]. Our case also did not present with any noticeable calcifications in radiographs; hence, the exclusion of differential diagnoses rested on MRI. Posterior knee lesions encompass a wide spectrum of benign and malignant entities – including Baker’s cysts, ganglion or parameniscal cysts, PVNS, lipoma arborescens, and synovial sarcoma – that can mimic non-calcified SC. These lesions often share overlapping clinical and radiological presentations, typically presenting as well-defined cystic or lobulated masses in the popliteal fossa. However, MRI may offer diagnostic clues: lipoma arborescens characteristically follows fat signal on all sequences and suppresses on fat-saturated imaging [12]; PVNS displays hemosiderin-related blooming artifacts on gradient echo or susceptibility-weighted sequences due to hemoglobin breakdown products [13]; and synovial sarcoma often presents with aggressive margins and solid enhancement – features that aid differentiation [14]. Nevertheless, histopathology remains the definitive diagnostic modality, confirming SC and excluding malignancy. This case report describes SC of the knee presenting as a non-calcified, well-defined encapsulated mass on MRI. The lesion exhibited features that closely resemble those of a sarcoma or a complex cyst, thus highlighting the diagnostic challenge posed by this rare presentation. The imaging characteristics of the mass make this case an important contribution to the understanding of SC in the knee. To contextualize our findings, we reviewed previously published case reports of non-calcified or atypically presenting SC around the knee. A comparative analysis of these reports (Table 1) highlights that such cases often mimic cystic or neoplastic lesions, reinforcing the diagnostic challenge and the pivotal role of MRI and histopathology in establishing a definitive diagnosis.
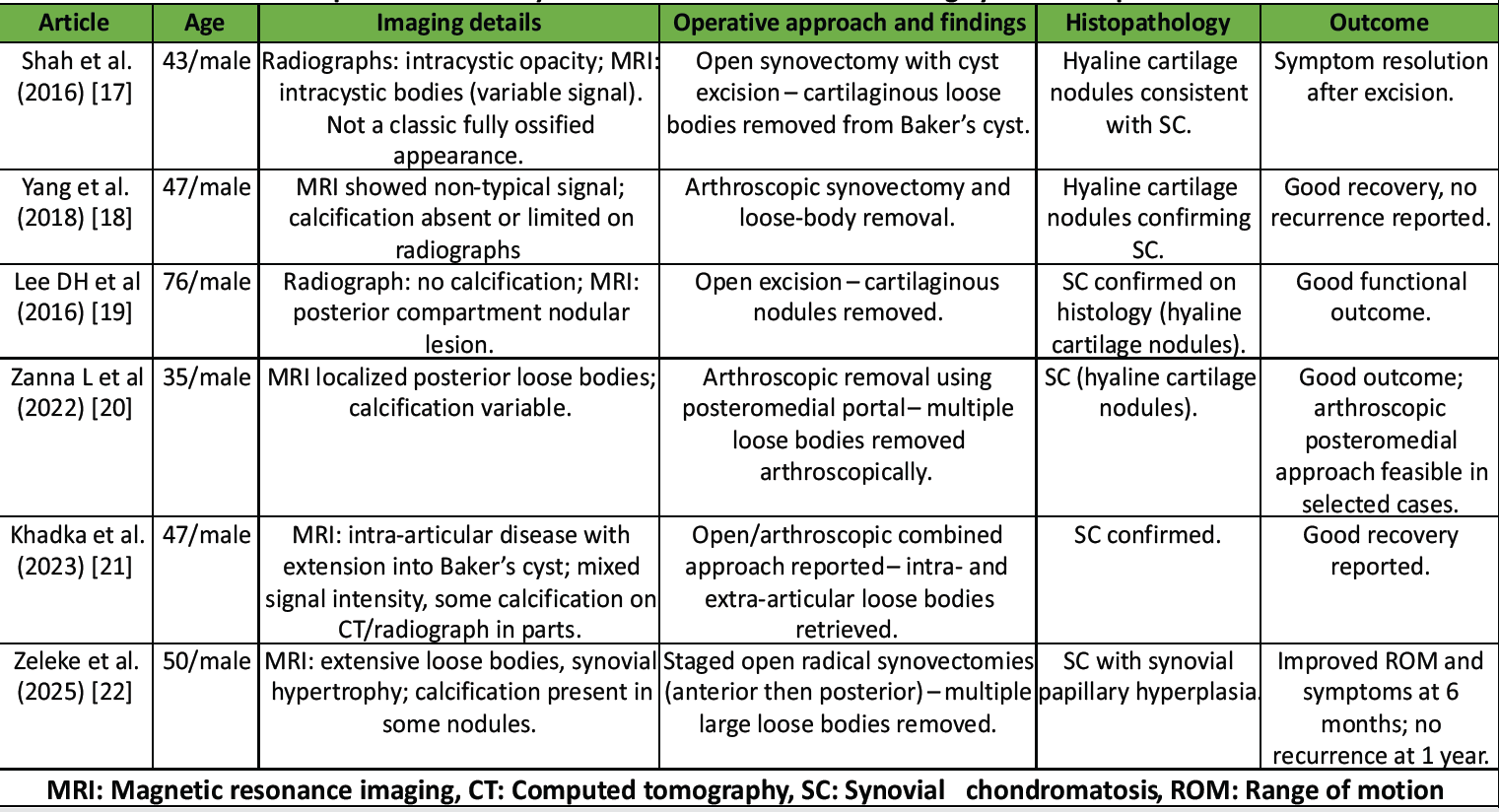
Table 1: Reported cases of synovial chondromatosis mimicking cystic or neoplastic lesions.
The goal for the treatment of SC is to remove the loose bodies, improve pain symptoms, regain movement in the joint, and limit the development of early osteoarthritis [15]. The treatment of choice is either open or arthroscopic surgical excision. Close long-term follow-up is recommended, because although rare, there is a chance of malignant change [3]. Recurrence after surgical excision of SC has been reported in 3–23% of cases, with the rate largely dependent on the completeness of synovectomy and removal of loose bodies [16]. Our patient successfully underwent an open excision of the lesion, and at the final follow-up, there was no recurrence of symptoms, demonstrating a favorable outcome following complete surgical excision.
SC is an uncommon etiology of knee pain and may present with atypical cystic formation. Awareness of this condition is essential for accurate diagnosis and effective management, as its presentation can be easily confused with other more common, aggressive pathologies.
Unusual presentations of SC – such as non-calcified, encapsulated posterior knee lesions – can be easily mistaken for benign or malignant masses. Recognizing these rare imaging variants and selecting an appropriate surgical approach are key to achieving accurate diagnosis and optimal patient outcomes.
References
- 1. Habusta SF, Mabrouk A, Tuck JA. Synovial Chondromatosis. 2023 Apr 22. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 29262110. [Google Scholar] [PubMed]
- 2. Serbest S, Tiftikçi U, Karaaslan F, Tosun HB, Sevinç HF, Balci M. A neglected case of giant synovial chondromatosis in knee joint. Pan Afr Med J 2015;22:5. [Google Scholar] [PubMed]
- 3. Hallam P, Ashwood N, Cobb J, Fazal A, Heatley W. Malignant transformation in synovial chondromatosis of the knee? Knee 2001;8:239-42. [Google Scholar] [PubMed]
- 4. Pimentel CQ, Hoff LS, de Sousa LF, Cordeiro RA, Pereira RM. Primary synovial osteochondromatosis of the knee. Rheumatology (Oxford) 2015;54:1815. [Google Scholar] [PubMed]
- 5. Paraschau S, Anastasopoulos H, Flegas P, Karanikolas A. Synovial chondromatosis: A case report of 9 patients. EEXOT 2008;59:165-9. [Google Scholar] [PubMed]
- 6. Frick MA, Wenger DE, Adkins M. MR imaging of synovial disorders of the knee: An update. Radiol Clin North Am 2007;45:1017-31. [Google Scholar] [PubMed]
- 7. Burks RT, Schaffer JJ. A simplified approach to the tibial attachment of the posterior cruciate ligament. Clin Orthop Relat Res 1990;254:216-9. [Google Scholar] [PubMed]
- 8. Jeffreys TE. Synovial chondromatosis. J Bone Joint Surg Br 1967;49:530-4. [Google Scholar] [PubMed]
- 9. Milgram JW. Synovial osteochondromatosis: A histopathological study of thirty cases. J Bone Joint Surg Am 1977;59:792-801. [Google Scholar] [PubMed]
- 10. Jang BG, Huh KH, Kang JH, Kim JE, Yi WJ, Heo MS, et al. Imaging features of synovial chondromatosis of the temporomandibular joint: A report of 34 cases. Clin Radiol 2021;76:627.e1-11. [Google Scholar] [PubMed]
- 11. Adelani MA, Wupperman RM, Holt GE. Benign synovial disorders. J Am Acad Orthop Surg 2008;16:268-75. [Google Scholar] [PubMed]
- 12. Narváez JA, Narváez J, Ortega R, Aguilera C, Sánchez A, Andía E. MR imaging of synovial tumors and tumor-like lesions. Eur Radiol 2001;11:2549-60. [Google Scholar] [PubMed]
- 13. Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA. Pigmented villonodular synovitis: Radiologic-pathologic correlation. Radiographics 2008;28:1493-518. [Google Scholar] [PubMed]
- 14. Rangheard AS, Vanel D, Viala J, Tardivon A, Couturier J, Cottias P, et al. Synovial sarcoma of the extremities: MRI and clinical characteristics of 34 cases. Skeletal Radiol 2003;32:701-9. [Google Scholar] [PubMed]
- 15. Sedeek SM, Choudry Q, Garg S. Synovial chondromatosis of the ankle joint: Clinical, radiological, and intraoperative findings. Case Rep Orthop 2015;2015:359024. [Google Scholar] [PubMed]
- 16. Vasudevan R, Jayakaran H, Ashraf M, Balasubramanian N. Synovial Chondromatosis of the Knee Joint: Management With Arthroscopy-Assisted “Sac of Pebbles” Extraction and Synovectomy. Cureus. 2024 Sep 13;16(9):e69378. doi: 10.7759/cureus.69378. PMID: 39411591; PMCID: PMC11473246. [Google Scholar] [PubMed] [CrossRef]
- 17. Shah DP, Diwakar M, Dargar N. Baker’s cyst with synovial chondromatosis of knee – a rare case report. J Orthop Case Rep 2016;6:17-19. [Google Scholar] [PubMed]
- 18. Yang YP, Wang JJ, Li HY. Atypical synovial chondromatosis of the right knee: A case report. Exp Ther Med 2018;15:4503-7. [Google Scholar] [PubMed]
- 19. Lee DH, Jeong TW. Uncommon primary synovial chondromatosis involving only the infrapatellar fat pad in an elderly patient. Knee Surg Relat Res 2016;28:79-82. [Google Scholar] [PubMed]
- 20. Zanna L, Secci G, Innocenti M, Giabbani N, Civinini R, Matassi F, et al. The use of posteromedial portal for arthroscopic treatment of synovial chondromatosis of the knee: A case report. J Med Case Rep 2022;16:457. [Google Scholar] [PubMed]
- 21. Khadka S, Chaudhary A, Acharya S, Maharjan S, Shrestha R. Baker’s cyst with extra- and intra-articular synovial chondromatosis of knee: A case report. Clin Case Rep 2023;11:e7068. [Google Scholar] [PubMed]
- 22. Zeleke SS, Nigussie KA, Mesfin YM, Fentie WM, Stein M, Molla DK. Disseminated synovial chondromatosis of the knee treated by open radical synovectomy using staged combined anterior and posterior approaches: A case report. J Med Case Rep 2025;19:152. [Google Scholar] [PubMed]








