Musculocutaneous neuropathy, though rare, should be considered in athletes with upper extremity symptoms and can be effectively diagnosed through multimodal imaging and treated with targeted interventions such as perineural steroid injection.
Dr. Nareka Trewick, Department of Neurosurgery, University of Miami Miller School of Medicine, Jackson Memorial Hospital, Miami, Florida, US State, E-mail: n.trewick@med.miami.edu
Introduction: Musculocutaneous nerve injury is a rare condition.
Case Report: We present a case of musculocutaneous neuropathy in a previously healthy 24-year-old professional baseball pitcher who began experiencing right arm weakness and forearm paresthesia a week after switching from a starter to a relief pitcher. Ultrasound confirmed entrapment of the coracobrachialis. Magnetic resonance imaging showed a hyperintense T2 fluid signal within the nerve, and electromyography demonstrated prolonged latency of motor and sensory function, along with evidence of active axonal injury. He experienced minimal symptom relief with a course of oral steroids and physical therapy. Subsequent steroid injection around the musculocutaneous nerve at the level of the coracobrachialis resulted in significant symptom improvement.
Conclusion: This case illustrates the importance of clinicians maintaining a high suspicion for rare peripheral neuropathies in elite athletes and remaining knowledgeable about appropriate diagnostic work-up and treatment.
Keywords: Musculocutaneous nerve, coracobrachialis, throwing athlete, musculocutaneous neuropathy.
There is a paucity of literature on musculocutaneous neuropathy, which is characterized by weakness of the elbow flexors and paresthesias along the lateral forearm as a result of surgical procedures, penetrating trauma, or anterior shoulder dislocation, or in rare cases – entrapment, with the most common site being the coracobrachialis [1]. The following case highlights the importance of a thorough history, physical examination, and supplemental imaging when evaluating for the cause of musculocutaneous neuropathy so that the proper treatment can be selected.
A 24-year-old previously healthy right-hand dominant male professional baseball pitcher presented with several weeks of moderate right upper arm and forearm pain with associated numbness/tingling. His symptoms started after pitching when he felt tightness in his biceps, progressing to paresthesia and biceps weakness. He denied antecedent trauma or change in his pitching form or routine. Family history was negative for neurological disorders. He underwent physical therapy with mild symptom relief but experienced fluctuation in pain level and persistent paresthesias in the lateral antebrachial cutaneous nerve distribution. He noted decreased warm-up time after switching from a starter to a relief pitcher, but no other improvement in symptoms. On presentation, vitals were within normal limits. Physical examination showed decreased sensation of the right volar forearm to wrist. He was able to flex, extend, cross fingers, and make a full composite fist without difficulty. There was a positive Tinel’s sign and hypersensitivity along the musculocutaneous nerve at the distal edge of the pectoralis insertion at the humerus. Strength testing showed 4+/5 strength of the right biceps compared to the left, as well as right biceps circumference of 34 cm compared to 32 cm on the left. Magnetic resonance imaging (MRI) and ultrasound of the right upper extremity were obtained (Fig. 1), which showed enlargement and T2 hyperintensity of the musculocutaneous nerve and coracobrachialis hypertrophy on MRI, with corresponding hypoechoic nerve echotexture at the level of the coracobrachialis on ultrasound.
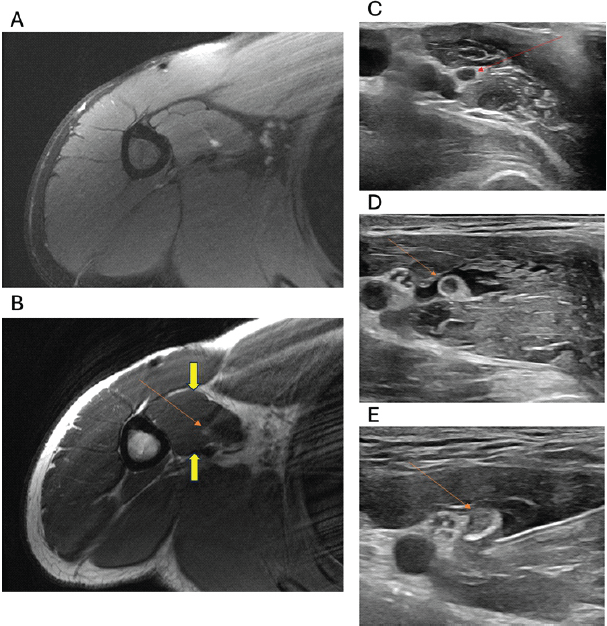
Figure 1: Imaging: Axial proton density fat sat (a) and axial proton density (b) magnetic resonance imaging showing enlargement and T2 hyperintensity of the musculocutaneous nerve (MCN) at the level of the coracobrachialis muscle (red arrows). There is hypertrophy of the coracobrachialis muscle (yellow arrows). Transverse grey scale ultrasound image showing enlargement and hypoechoic echotexture of the MCN at the level of the coracobrachialis muscle (red arrow) (c) US-guided hydrodissection with steroid and anesthetic mixture injection around the MCN at the level of the coracobrachialis muscle (red arrows) (d and e).
Nerve conduction studies and electromyography (EMG) were also completed, which corroborated right musculocutaneous nerve injury (Fig. 2).
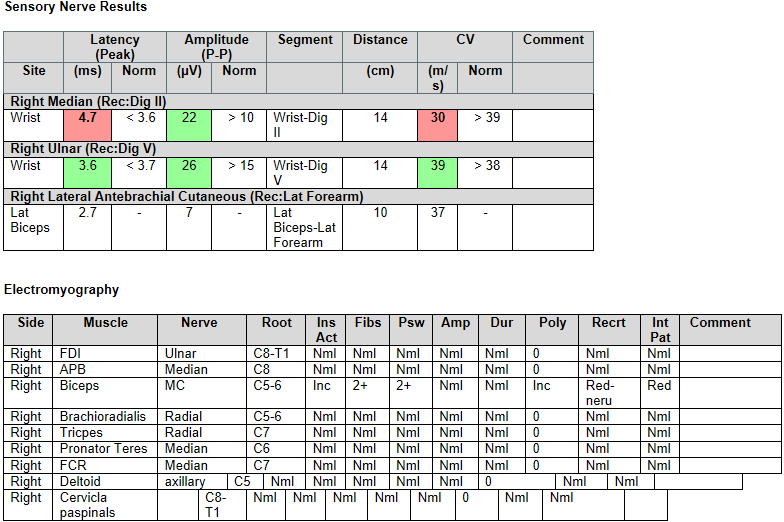
Figure 2: Sensory nerve results and electromyography: Nerve conduction studies showed evidence of right musculocutaneous nerve injury, with prolonged distal onset latency and reduced amplitude compared to the left. All remaining nerves were within normal limits. There was an incidentally prolonged median motor and sensory distal latencies. Needle electromyography of the right upper extremity revealed 2+ positive waves and fibrillations limited to the biceps only, with polyphasic recruitment suggestive of spontaneous reinnervation. There was no evidence of cervical radiculopathy. Bilateral incidental carpal tunnel syndrome was noted.
The patient was diagnosed with right musculocutaneous neuropathy with active denervation. He was advised to refrain from pitching for at least 1 month. He received occupational therapy, celecoxib, and an oral methylprednisolone course with mild symptom improvement, but significant symptom improvement after ultrasound-guided steroid injection. Ultrasound-guided hydrodissection with a steroid and anesthetic mixture was performed around the musculocutaneous nerve at the level of the coracobrachialis.
This case describes an isolated unilateral musculocutaneous neuropathy. The musculocutaneous nerve, from C5 to C7 roots, innervates the coracobrachialis and biceps brachialis and terminates as the lateral antebrachial cutaneous nerve, often entrapped at the coracobrachialis. Injury mechanisms include repetitive upper extremity activity or nerve compression. A thorough history, physical exam, ultrasound, MRI, and electrodiagnostic studies are critical for diagnosis and treatment planning. Ultrasound confirmed entrapment at the coracobrachialis with hypoechoic echotexture. Ultrasound findings in musculocutaneous neuropraxia typically include a musculocutaneous nerve that appears enlarged secondary to edema or inflammation, presenting as more hypoechoic than normal due to increased water content within the nerve fibers. The normal fascicular pattern of the nerve may be disrupted or less distinct, losing the appearance of small, parallel hypoechoic areas within the hyperechoic epineurium. Perineural fluid, indicating edema, is visualized as hypoechoic or anechoic areas surrounding the nerve. Changes in the muscles innervated by the nerve, such as the biceps brachii and brachialis, may include muscle atrophy or increased echogenicity due to fatty infiltration over time. Ultrasound can also be used dynamically to assess the nerve during movement, identifying areas of entrapment or compression that may not be visible in a static examination. MRI showed T2 hyperintensity and nerve enlargement. MRI findings in neuropraxia, particularly involving the musculocutaneous nerve, include several indicative features. Increased T2 signal intensity is often observed within the affected nerve, reflecting edema or inflammation [2], and this appears as a bright signal on fat-suppressed sequences. Perineural edema, or fluid around the nerve, also presents as increased signal intensity on T2-weighted and short tau inversion recovery sequences. Secondary changes in the muscles innervated by the affected nerve, such as muscle edema or fatty infiltration, indicate chronic denervation, while acute denervation might show muscle swelling and increased signal intensity [2]. Severe cases may reveal a disruption or loss of the normal fascicular architecture of the nerve, visible as a loss of the typical “honeycomb” appearance on high-resolution imaging. Electrodiagnostic studies revealed prolonged latency and axonal injury, with fibrillations on EMG indicating active denervation [3,4]. Needle EMG also showed polyphasic recruitment suggestive of spontaneous reinnervation. The mechanism of injury for musculocutaneous neuropraxia in a professional baseball pitcher likely involves several interrelated factors. The repetitive overuse inherent in pitching, characterized by rapid and forceful shoulder and elbow flexion, can lead to repeated microtrauma to the musculocutaneous nerve as it passes through the coracobrachialis muscle. Muscle hypertrophy due to repetitive use can further exacerbate nerve compression. Anatomical variations, such as a hypertrophied or accessory coracobrachialis longus muscle, increase the risk of nerve entrapment. Studies highlight anatomical variants, nerve courses through the coracobrachialis, and entrapment in active individuals, endorsing imaging and EMG for diagnosis [5,6,7]. In addition, the transition from a starter to a relief pitcher reduces warm-up time, leading to sudden overuse of the arm muscles without adequate preparation. Improper pitching mechanics or sudden changes in technique can place abnormal stress on the shoulder and upper arm, contributing to nerve compression or traction injuries [3]. The shoulder’s positioning during pitching, often abducted and externally rotated, can stretch and compress the musculocutaneous nerve [8]. While less common, direct trauma to the upper arm during play could also contribute to nerve injury. These factors collectively lead to nerve irritation, compression, or traction injuries, resulting in neuropraxia [9,10].
Clinicians should suspect rare peripheral neuropathies such as musculocutaneous neuropathy, particularly in the case of athletes undergoing intense training. Diagnosis relies on ultrasound, MRI, and electrodiagnostic studies. Treatment includes rest, activity modification, anti-inflammatories, and steroids. If symptoms persist, surgical options such as epineurotomy, decompression, nerve graft, and nerve transfer may be considered.
This case highlights the importance of recognizing musculocutaneous neuropathy as a potential source of upper extremity pain and weakness, particularly in athletes exposed to repetitive overhead activity. The combination of detailed clinical examination, high-resolution ultrasound, MRI, and electrodiagnostic studies was essential in identifying the entrapment and characterizing the extent of nerve injury. Unique anatomical factors, training load, and mechanical stress, especially in high-performance sports like baseball, can predispose individuals to this rare condition. Early diagnosis is critical to avoid progression to chronic denervation and functional impairment. Ultrasound proved especially valuable in localizing entrapment dynamically, reinforcing its role in real-time evaluation. Clinicians should maintain a high index of suspicion for this condition in overhead athletes and consider a multimodal imaging and electrodiagnostic approach to guide effective treatment.
References
- 1. O’Gorman CM, Kassardjian C, Sorenson EJ. Musculocutaneous neuropathy. Muscle Nerve 2018;58:726-9. [Google Scholar] [PubMed]
- 2. Sneag DB, Zochowski KC, Tan ET. MR neurography of peripheral nerve injury in the presence of orthopedic hardware: Technical considerations. Radiology 2021;300:246-59. [Google Scholar] [PubMed]
- 3. Jung JW, Park YC, Lee JY, Park JH, Jang SH. Bilateral musculocutaneous neuropathy: A case report. World J Clin Cases 2021;9:1237-46. [Google Scholar] [PubMed]
- 4. Alanazy MH, Muayqil T, Aldraihem MO, Alkhawajah NM. Electrodiagnostic reference data for sensory nerve conduction studies in Saudi Arabia. Neurosciences (Riyadh) 2020;25:112-7. [Google Scholar] [PubMed]
- 5. Olewnik L, Paulsen F, Tubbs RS, Zielińska N, Szewczyk B, Karauda P, et al. Potential compression of the musculocutaneous, median and ulnar nerves by a very rare variant of the coracobrachialis longus muscle. Folia Morphol (Warsz) 2021;80:707-13. [Google Scholar] [PubMed]
- 6. Pecina M, Bojanic I. Musculocutaneous nerve entrapment in the upper arm. Int Orthop 1993;17:232-4. [Google Scholar] [PubMed]
- 7. Pantekidis I, Piagkou M, Koutserimpas C, Samolis A, Tsakotos G, Kostares M, et al. A review of the typical course of the musculocutaneous nerve into the coracobrachialis muscle: Its variability and possible clinical implications. Acta Med Acad 2023;52:95-104. [Google Scholar] [PubMed]
- 8. Vineyard AP, Gallucci AR, Imbus SR, Garrison JC, Conway JE. Residents case report: Musculocutaneous nerve injury in a collegiate baseball pitcher. Int J Sports Phys Ther 2020;15:804-13. [Google Scholar] [PubMed]
- 9. Campbell WW. Evaluation and management of peripheral nerve injury. Clin Neurophysiol 2008;119:1951-65. [Google Scholar] [PubMed]
- 10. Durner G, Gerst A, Ulrich I, Mayer B, Wirtz CR, König R, et al. Restoring musculocutaneous nerve function in 146 brachial plexus operations – a retrospective analysis. Clin Neurol Neurosurg 2023;228:107677. [Google Scholar] [PubMed]