To evaluate the alignment of the lower limb post total knee arthroplasty (TKA) by taking a variable distal femoral cut according to the Femoral Anatomical Mechanical Angle (FAMA) on long leg standing radiograph preoperatively.
Dr. K P Chiranjeevi, Department of Orthopaedics, Apollo Hospital, Navi Mumbai, Maharashtra, India. E-mail: chiranjeevipirabhu@gmail.com
Introduction: In the present study, we had pre-operative determination of the femoral anatomical mechanical angle which was accomplished using anteroposterior weight-bearing hip-to-ankle radiographs. Intraoperative distal femur variable valgus cut was taken depending upon preoperative Femoral Anatomical Mechanical Angle (FAMA). We accessed pre and post-operative mechanical axis of the lower limb on long-length X-ray films and evaluation of functional outcome.
Aims and Objective: To study pre and post-operative FAMA and lower limb alignment in post-operative long leg standing radiograph. Study Duration: 12 months Study Design: Prospective study Sample Size: 52 Patients
Conclusion: The study findings recommended that all patients for the primary total knee arthroplasty should be evaluated with long leg weight-bearing radiograph preoperatively to find lower limb alignment and FAMA. Intraoperatively, distal femur valgus cut should be taken variable depending upon preoperatively evaluated FAMA.
Keywords: FAMA, total knee arthroplasty, knee alignment.
Osteoarthritis (OA) of the knee joint is certainly increasing among elder population as extended longevity [1]. At present, approximately 2% of the population of 55 years age and above are so disabled that they need total knee arthroplasty (TKA) due to OA knee and this rate increases with age. The average incidence is twice in woman than in men [2]. TKA is indicated for pain relief and functional improvement in severe knee joint degeneration and arthritis. The goals of TKA surgery include adequate alignment of the prosthesis components and the limb, stability of the knee for functional outcome [3]. In cemented TKA, longevity ranges from 91% to 99% by 10 years and 91–96% by 15 years [4,5]. Unfortunately, failure after TKA occurs in some patients. Malalignment is one factor that a surgeon can prevent [6]. Restoring the coronal plane mechanical axis of the lower limb to within 3° of normal during TKA is associated with decreased loosening and greater long-term survival of the prosthesis [7,8]. A TKA malalignment of more than 3° can lead to a significantly higher rate of failure [9]. To prevent it, a neutrally aligned lower limb has been one of the primary goals of TKA because it was supposed to be important for successful clinical outcomes and implant survivorship [10].
Aim
To evaluate alignment of lower limb post TKA by taking variable distal femoral cut according to the femoral anatomical mechanical angle (FAMA) on long leg standing radiograph preoperatively.
Objective
- To study the FAMA in patients with arthritis knee in long leg standing radiograph
- To study post-operative FAMA and lower limb alignment in post-operative long leg standing radiograph
- To calculate Oxford Knee Score (OKS) and Knee Society Score (KSS) in patients with arthritis knee pre-operative and post-operative functional outcome.
Study duration
12 months.
Study design
Prospective study.
Sample size
52 Patients.
Sample size calculation
Independent of the surgeon’s experience it was found an alignment of more than ± 3° varus/valgus in 25% of cases after total knee replacement [11]. Considering the same proportion in the present study and 13% marginal error using the proportionate sample size formula calculated sample size was 43. A total of 52 cases were involved in study considering 10% non-response rate.
Formula for sample size
n = z2pq/d2
Where, n = sample size, Z = 1.96, P = proportion of an alignment of more than ±3° varus/valgus (25%), q = 100–p and d = assumed marginal error.
Inclusion criteria
- Only primary TKA
- Patients with arthritis knee
- Patients without neurovascular deficit
- Patients who have varus deformity
- Patients who are medically fit to undergo surgery
- Patients who consented for surgery and study
- Patients who can stand for long leg radiograph (scanogram).
Exclusion criteria
- Patients with fixed flexion deformity more than 30°
- Patients with genu recurvatum more than 20°
- Patients with neurovascular deficit and compartment syndrome
- Patients with pathological fractures
- Patients who are unfit for surgery
- Not able to stand
- All revision surgeries
- Patients who have valgus deformity.
Long leg standing anteroposterior radiograph of both lower limbs (scanogram)
Originally scanogram was believed to be obtained on a single long cassette (35 × 110 cm) visualizing all three joints, namely hip joint, knee joint, and ankle joint in one conventional radiograph. Scanogram was taken as a modification by taking with four separate exposures each one centered over hip, femur, knee, and ankle using a standard-sized cassette (35 × 43 cm) on digital X-ray. The patient-to-tube distance is 101 cm. It is very important to take this radiograph in neutral rotation of the legs to obtain accurate measurements with the patella facing forwards and inspecting the relation between tibia and fibula, distally and proximally. Later, all these films stitch together in a single radiograph. All digital radiographs were processed and measured by research team using picture archiving and communication system (PACS) software Medsynapse 3.1.1., Fujifilm Medical Systems USA, Inc., Stamford, with a minimum detectable change of 1° between two lines drawn on the digital images.
Alignment and measurement on scanogram
All radiographs were obtained with a consistent technique with the patients standing on both legs with medial aspect of their feet parallel to each other, with knees in full extension. Mechanical axis of femur is line joining from femoral head to midpoint of distal femur. The center of the femoral head was identified by locating the center of a close-fit circle generated at the edge of the femoral head. Midpoint of distal femur is taken at the edge of femoral notch (from where the femoral jig entry taken during TKA). Anatomical axis of the femur is line joining center of pyriformis fossa to mid-point of distal femur at knee joint. The angle between the anatomical axis and the mechanical axis of the femur is called femoral anatomical mechanical axis (FAMA) is calculated using eclipse function on PACs (Fig. 1).
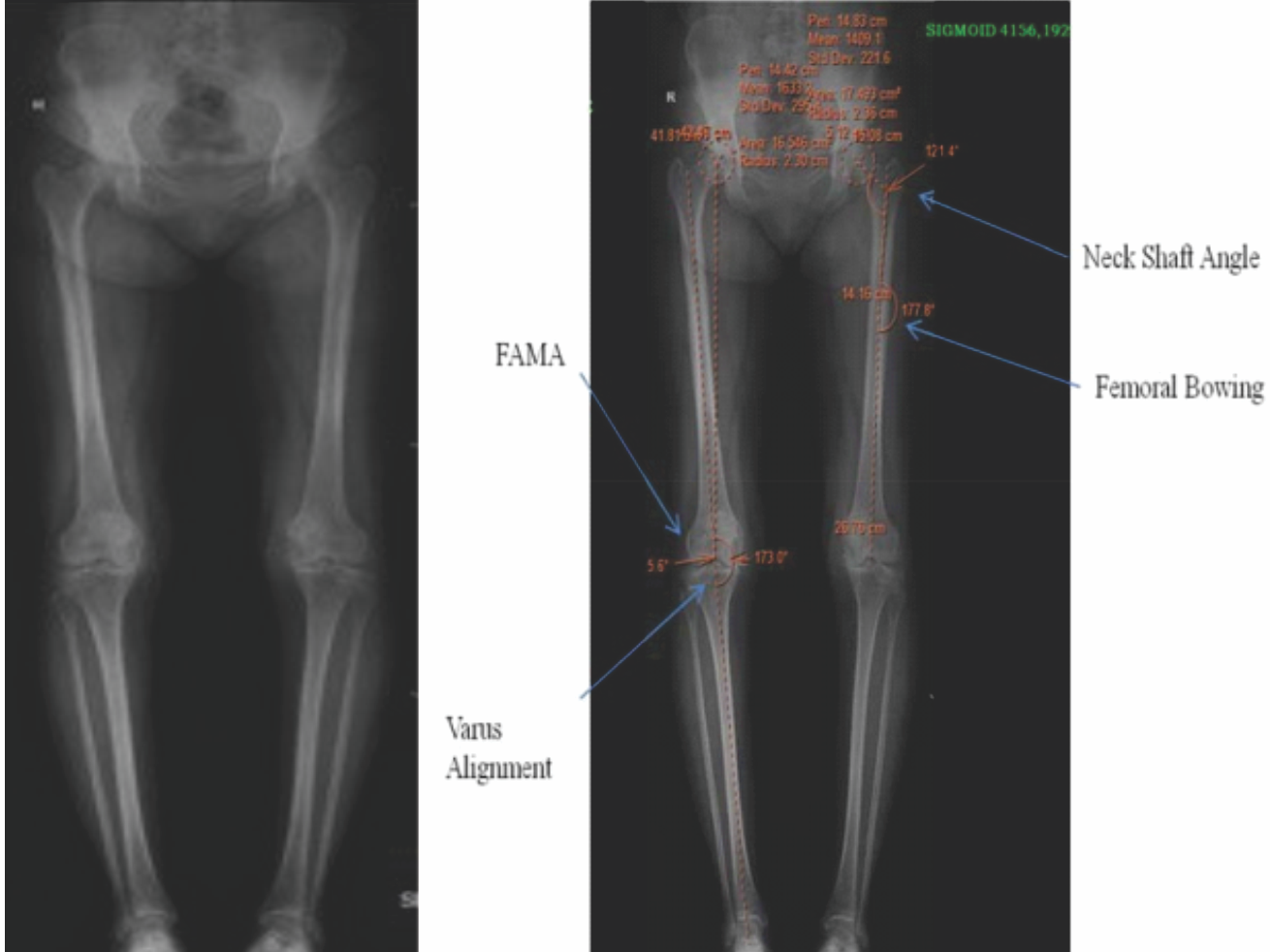
Figure 1: (Long leg radiograph) scanogram.
For post-operative FAMA center of the distal femur is taken at a similar point as pre op. The tibial anatomical and mechanical axes are the same. It is calculated as the line joining center of the tibial spine to the center of the talus. Lower limb alignment was evaluated pre and post-operative scanogram. Mechanical alignment of lower limb is measured by the angle formed by the mechanical axis of femur and tibia. Ideal mechanical axis of lower limb is 180 ± 30. Femoral neck shaft angle is measured by the angle between the longitudinal femoral shaft axis and the femoral head neck axis. The axis of the femoral neck is defined by a line bisecting the femoral neck width through the center of the femoral head. The femoral bowing was the angle between the distal and proximal femoral anatomical axis was obtained by drawing a line between the two femoral shaft centers in the middle upper portion of the femur.
Pre-operative
- Counseling of patient and relatives was done with regard to time of surgery, prognosis and risk factors, and post-operative recovery.
- To check the functional status of patients OKS and KSS were taken pre-operatively.
- All routine investigation required for TKA was done including blood investigations, cardiac investigations, and radiological investigation (like knee radiograph and scanogram).
- If patient is having any comorbidities then treated them according to required cross consultant.
- Patient underwent routine pre-anesthetic checkup.
- Consent regarding surgery and study was taken from patient.
- The surgery was performed under spinal with epidural anesthesia in all cases.
- All surgeries were performed by single surgeon using posterior stabilizing (posterior cruciate ligament sacrificing) prosthesis. In all cases, patella resurfacing was done.
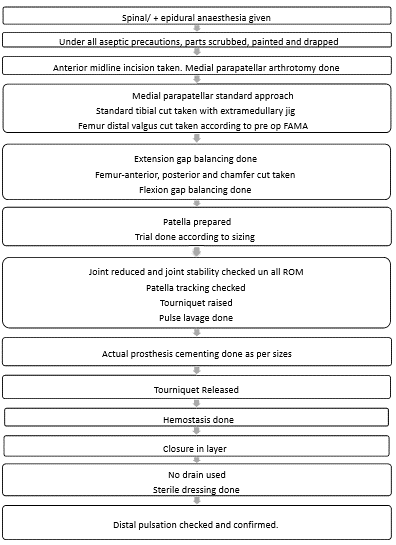
Post-operative
- On day 0, pain management was done using analgesics/epidural, etc. Antibiotics/antacids and deep vein thrombosis prophylaxis were given till admission.
- On day 1, physiotherapy was started. Patient mobilized out of bed.
- Discharge was given at day 3 and 1st follow-up was taken after 14 days from surgery for suture removal and to evaluate patient.
- All the patients were assessed both clinically at regular interval.
- At 6 months, patient was evaluated for functional outcome clinically based on OKS, KSS, and radiologically for mechanical alignment of the lower limb and FAMA using scanogram.
Data analysis
Data were entered into Microsoft Excel and analyzed using the Statistical Package for the Social Sciences Software 20. Categorical variables were expressed in terms of frequency and percentage and continuous variables were expressed in terms of mean and standard deviation. Paired t-test was applied to see any significant difference in continuous variables (FAMA, KSS, and OKS) among study group in pre-operative and post-operative follow-up with P < 0.05 as a significant value.
In current study, patient demographics for 52 patients and 71 knees were determined. In our study, there were 12 males with mean age 69.3 years (min 54 years and max 82 years) and 40 females with mean age 62.01 years (min 48 years and max 75 years). Half of the subjects 49.0% were in age group of 61–70 years (n-25), followed by 32.09% in age group of 51–60 years (n-17) and 19.2% in age of >70 years (n-10). Total mean age of study was 63.56 years. In the operated, 47.88% were left side and 52.11% were right side.
Average height of the subjects was 157.81 cm (minimum 143 cm and maximum 176 cm) and average weight of the subjects was 71.9 kg (minimum 51 kg and maximum 120 kg).
Most common co-morbidity was hypertension (65.4%), followed by diabetes in 19.2% subjects, rheumatoid arthritis 5.7%, and IHD 1.9%.
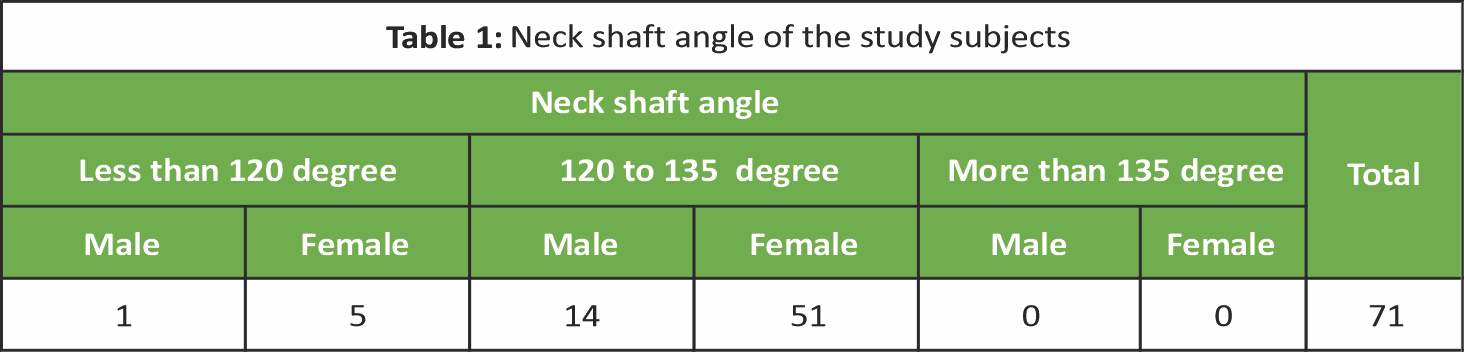
Most of the subjects of the study body mass index (BMI) were overweight 40.4% (n-21), followed by 38.5% were obese (n-20), followed by 21.2% were normal (n-11). Preoperatively lower limb alignment was varus in all cases with mean 10.9 ± 5.4 (min 1.2 and max 26.8) out of which <3° varus was noted in 1 case. 3–10° varus noted in 27 number of cases and 28 cases were having varus more than 10°. The FAMA was varied from mean (6 ± 0.9) (mini 4.2 to max 7.9). Less than 4° was noted in 0 pts. 4–6° was noted in 35 numbers of knees (male 9 knees and female 26 knees). More than 6° FAMA is found in 36 number of knee (male 6 knees and female 30 knees). Femoral neck shaft angle was measured and called coxa vara, i.e., <120° in 6 number of patients. Normal femoral neck shaft angle (120–135°) was noted in 65 numbers of patients. Coxa valga was not noted in any patients (Table 1).
Femoral bowing was measured between 0 and 3° in 4 numbers of cases (Table 2).
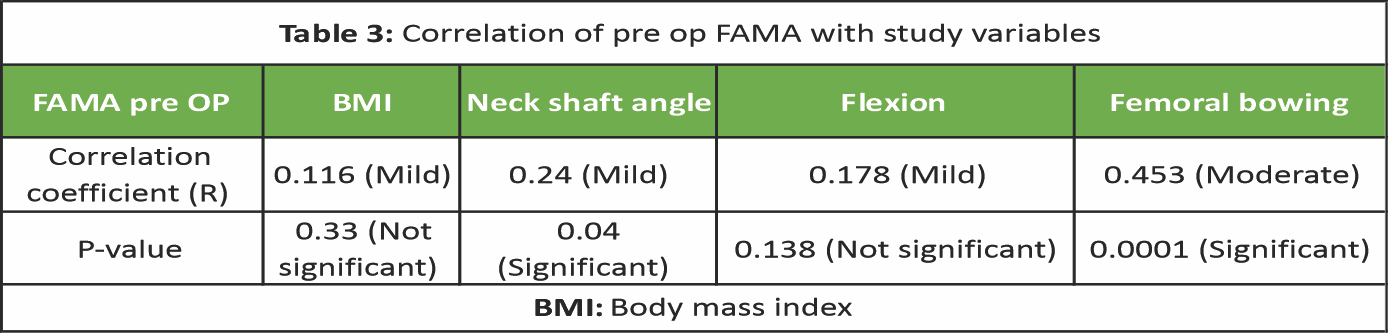
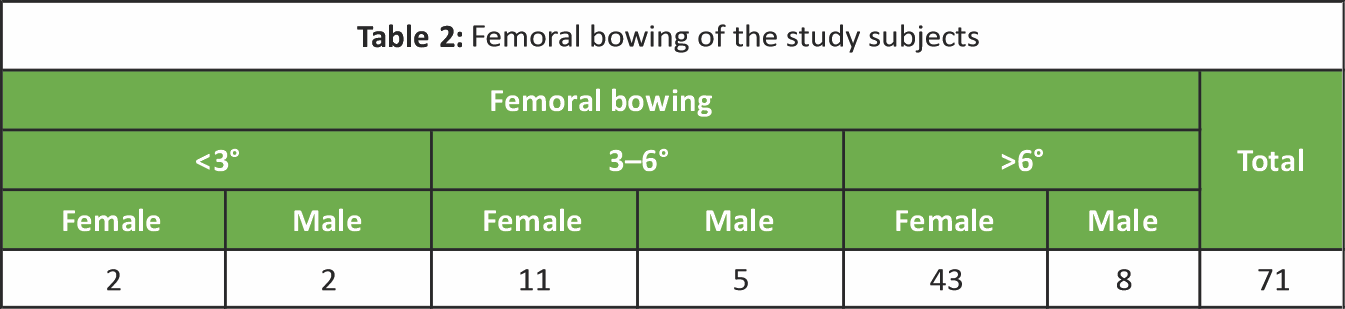 Bowing between 3 and 6° was measured in 16 numbers of cases and more than 6° of bowing was noted in 51 numbers of cases. We have evaluated the factors affecting FAMA and the Pearson correlation coefficient evaluated. FAMA has a significant correlation with neck shaft angle and femoral bowing of lower limb. FAMA has mild significance with pre-operative varus deformity. It has not significant correlation with BMI (Table 3).
Bowing between 3 and 6° was measured in 16 numbers of cases and more than 6° of bowing was noted in 51 numbers of cases. We have evaluated the factors affecting FAMA and the Pearson correlation coefficient evaluated. FAMA has a significant correlation with neck shaft angle and femoral bowing of lower limb. FAMA has mild significance with pre-operative varus deformity. It has not significant correlation with BMI (Table 3).
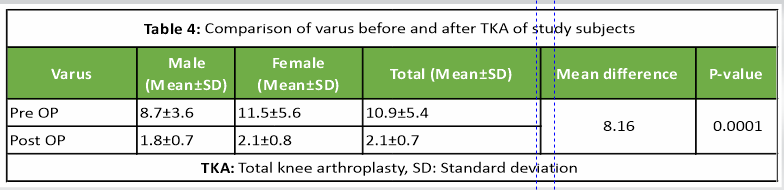
Comparing the pre-operative and post-operative alignment of the lower limb (Fig. 2), there was a decrease in varus measurement before and after TKA and it was statistically significant. In post-operative varus, ≤3° alignment was achieved in 97% (n – 69 knees) and outliers were 3% (n-2 knees). Hence, the neutral alignment was achieved in more number of patients.
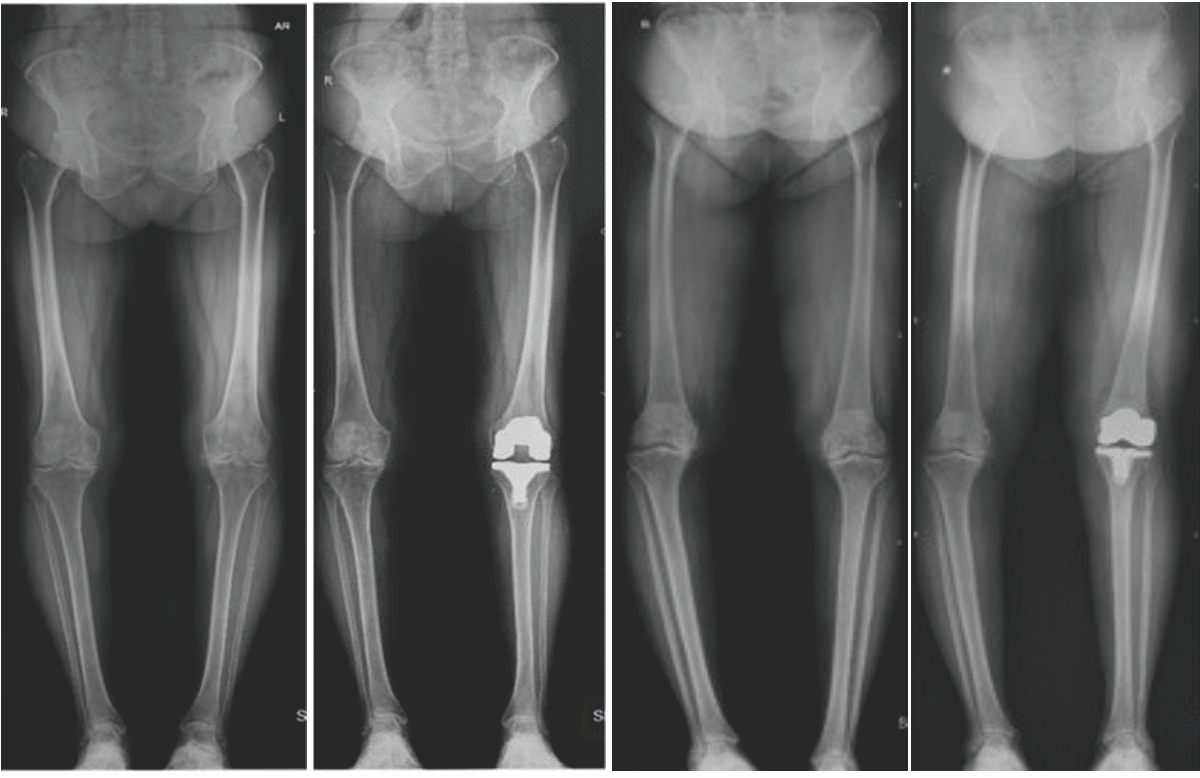
Figure 2: Pre op and post op long leg weight-bearing radiological images of study subjects.
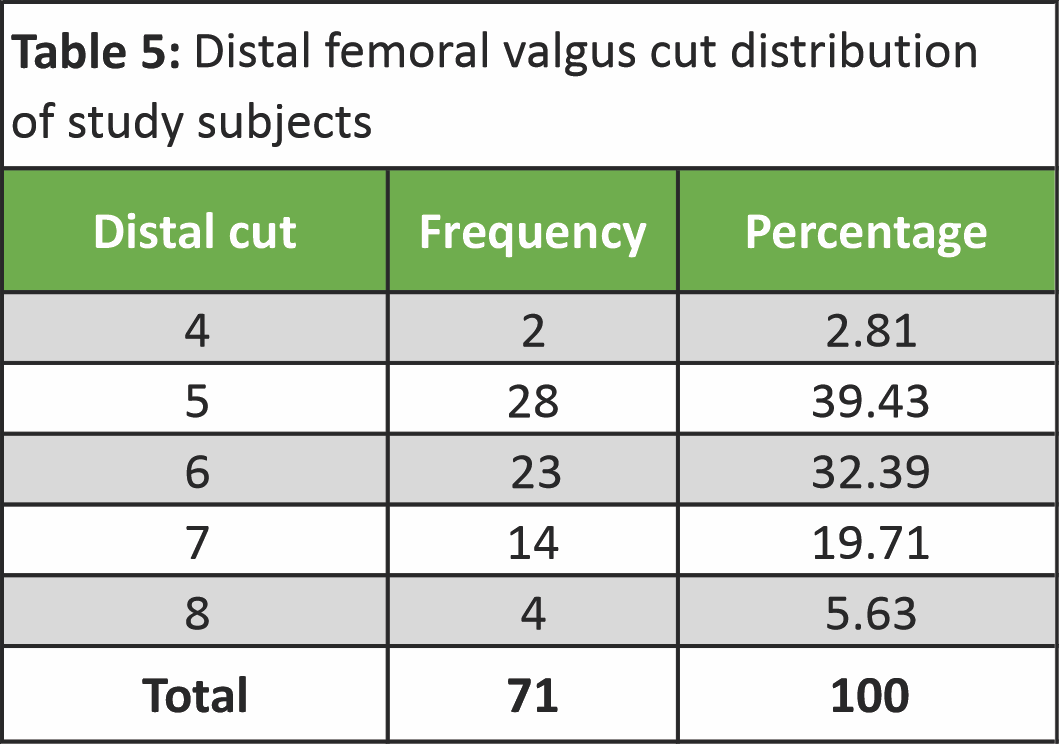
Intra-operative distal femoral valgus cut ranged from 4° to 8° as per pre op FAMA (40–2 knees, 50–28 knees, 60–23 knees, 70–14 knees, and 80–4 knees). Comparing the pre-operative and post-operative FAMA shows that there is no statistically significance in between femoral and mechanical axis of femur. Evaluating OKS before and after TKA, there was increase in OKS after TKA surgery and this difference in OKS before and after TKA was statistically significant (P < 0.05). KSS before and after TKA, there was increase in KSS after TKA surgery and this difference in KSS before and after TKA was statistically significant (P < 0.05).
In TKA, restoration of lower limb alignment is done taking various bone cut in distal femur and proximal tibia. These cut also required for accurate placement of femoral and tibial component. Hence, survivorship of TKA depends on optimal alignment of components to correct restoration of the lower limb mechanical alignment by the accuracy of bone cuts [12,13,14]. In arthritis population, there is a wide variation of deformities. To achieve patient-specific alignment, pre-operative assessment of the axial alignment of the lower extremity is important. This assessment is done on weight bearing full-length radiograph of the lower limb including the hip, knee, and ankle [15]. Axial alignment of lower limb is angle between mechanical axis of femur and tibia. Usually, the mechanical axis of lower limb is 180 ± 3° meaning the line joining center of femur head to center of ankle should pass through center of distal femur at the level of knee joint [16]. On long leg standing radiograph, we can also evaluate other axis which is important for alignment of lower limb like anatomical and mechanical axis of femur and tibia. The anatomical axis of femur is line joining center of pyriformis fossa to mid-point of femur at knee joint. Mechanical axis of femur is line joining center of femoral head to midpoint of femur at knee joint level. The angle between the anatomical axis and the mechanical axis of the femur is known as femoral anatomical mechanical axis (FAMA). It can used to determine the angle of resection of the distal femur in TKA [17]. In conventional TKA, to align the mechanical axis of the lower limb in the neutral position, we should take bone cuts perpendicular to the mechanical axis of tibia and femur. In the tibia mechanical and anatomical axes are equal hence with the help of extra medullary zig, we can accurately take perpendicular cut of tibia. In femur intraoperatively, distal valgus femoral cut is taken to correct mechanical alignment with the help of zig with intramedullary guide. Hence, it will equivalent to the anatomical axis of the femur. The distal cut of the femur should ideally be perpendicular to its mechanical axis of femur. To attain this, the valgus correction angle must be the same as the angle between the mechanical and anatomical axes of the femur [18,19,20].
There are methods described to determine the valgus correction angle: First, taking a fixed cut of 5° and 6° valgus for all cases. Second is determining it preoperatively by measuring the angle between the anatomical and mechanical axes of the femur on long leg radiographs and distal femoral variable valgus cut taken depending on FAMA. There is a wide distribution of the FAMA in the arthritic population ranging from 2° to 9°. Studies have shown that a routine 5° or 6° valgus correction angle may be safe for uncomplicated TKA [19,11,21]. A few studies have, however, shown that a routine choice of fixed 6° valgus cut taken irrespective of pre op deformity restored the alignment to neutral in 85% of cases [22]. In many studies, the distal femoral valgus cut taken as a variable depending on FAMA has shown improved femoral component and axial alignment [23,24]. Understanding these variations in existing literature it is important to determine each patient’s FAMA in the preoperative planning of TKA to prevent malalignment of the femoral component, which may lead to instability, wear, and loosening [16]. In present study, intraoperative distal femur valgus cut was taken as variable depending upon preoperative FAMA, not taken fixed 6° valgus as described by Andrews SN et al., in 2019 [23]. We have studied factors affecting pre-operative FAMA. We assessed pre and post-operative lower limb alignment on long-length X-ray films as well as KSS and OKS during 6-month follow-up for patient satisfactory outcome. In our study, mean age subject was 64.33 ± 7.2 years and range of 51–82 years. Female-to-male ratio was 3:1. In our study, cases were 47.88% of the left side and 52.11% of the right side. It is important to determine each patient’s FAMA in the pre-operative planning of TKA. Lower limb alignment should be neutral and survivorship of TKA depends on the accuracy of bone cuts, optimal alignment of components to the correct restoration of the lower-limb mechanical axis [12,13,14]. In TKA, the valgus or varus deformity is restored by means of femoral and tibial bone cuts perpendicular to the mechanical axis [25]. Tibial cut is usually achieved perpendicular with jig as mechanical and anatomical axis of tibia is same. In femur however intramedullary jig matches to anatomical axis. To take perpendicular cut to mechanical axis, we should consider other factor like femoral bowing, neck shaft angle for take distal femur valgus cut [26]. In our study, FAMA has found a significant correlation with neck shaft angle and femoral bowing and it is not affected by BMI and pre op varus deformity. In a study by Shi et al., [27] Asian population found as more femoral bowing can affect outcome of TKA and suggested variable angle distal cut of femur achieves better radiological alignment and femoral component positioning. Correlation between FAMA and femoral bowing suggests that FAMA is one of the factors affecting lower limb alignment in TKA. There is a wide distribution of the FAMA in the osteoarthritic population [5]. Similar results were found in our study with min 4.2° and max 7.9°. In present study, postoperatively very few 3% of the patient had malalignment >3°. Majority patient (97%) was alignment <3° varus (Table 4).
The persistent varus deformity in alignment of post-operative lower limb is due to result from varus in tibia. All subjects had distal femoral cut in the range of 4–8° and few had 6° (32.3%) valgus cut during TKA, as we have taken a variable distal femoral cut depending upon pre-operative FAMA (Table 5).
 Similar results were shown in studies by Nam et al., [23] and Zhou et al., [24]. Furthermore, there is no difference found in pre op and post op FAMA; it means that the femoral anatomy was maintained (P = −0.21) (Table 6); hence, no statistically significant difference in FAMA means that the femur is more aligned with mechanical axis of lower limb. Andrews SN et al., [22] taken fixed distal valgus cut 6° in study and achieved neutral alignment in 85% cases.
Similar results were shown in studies by Nam et al., [23] and Zhou et al., [24]. Furthermore, there is no difference found in pre op and post op FAMA; it means that the femoral anatomy was maintained (P = −0.21) (Table 6); hence, no statistically significant difference in FAMA means that the femur is more aligned with mechanical axis of lower limb. Andrews SN et al., [22] taken fixed distal valgus cut 6° in study and achieved neutral alignment in 85% cases.
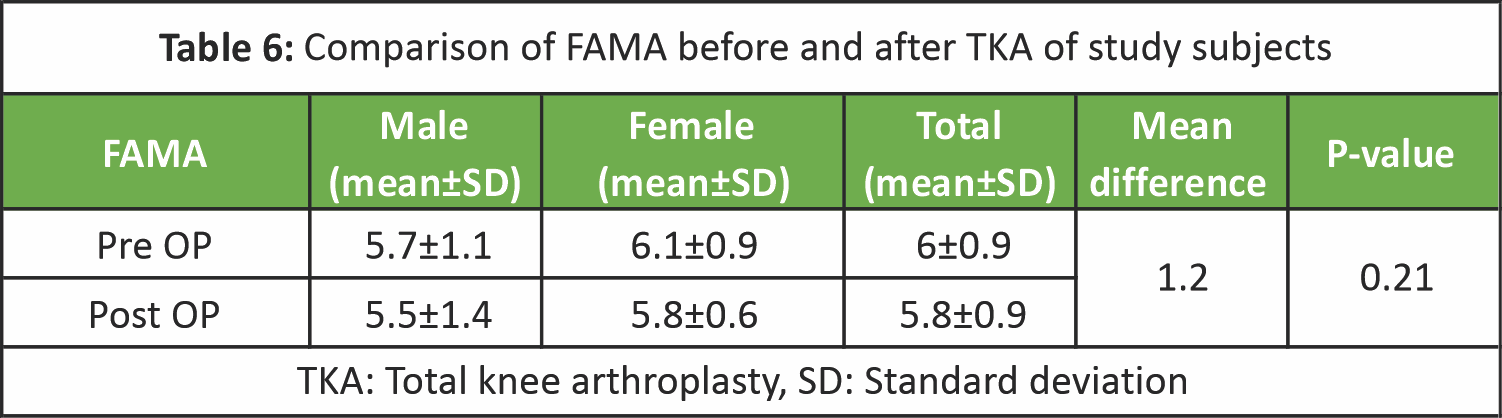 In our study, we had taken variable degree of distal valgus cut according to pre op FAMA and neutral alignment achieved in 97% cases. Femoral component placement is accurate shown by improved femoral mechanical axis postoperatively. Similar result had shown by Lee et al., [26] Nam et al., [23], and Zhou et al., [24]. In general, coronal plane limb alignment within 2–3° around a neutral alignment. Despite clear limitations of the available scientific data, most surgeons believe that a neutral mechanical axis also confers a substantial advantage in terms of TKA implant survivorship [28]. Incorrect alignment can lead to abnormal wear [29,30], early mechanical loosening of the components [7,8], and patella-femoral problems [31]. Deviations of >3° varus or valgus will increase the rate of loosening in the coronal plane [5]. Huang et al., [32] reported that TKAs with a coronal alignment within 3° from the neutral axis had better function and quality of life at 5-year follow-up than TKAs that deviated more than 3° from neutral alignment. Magnussen et al., [33] found KSS to be better in patients with residual varus than in those with neutral alignment. In our study, we used OKS score to measure TKA outcome score in the present study. It was found that there was statistically significant improvement in the mean value of OKS in pre (15.88 ± 2.6) and post-operative (42.27 ± 2.5) follow-up (P < 0.05). It was found that there was statistically significant improvement in mean value of KSS in pre (33.42 ± 4.8) and post-operative (82.38 ± 2.8) follow-up (P < 0.05). Findings of our study though found significant difference in OKS score before and postoperatively but could not compare with existing literature due to short-term follow-up and no comparison group was studied but findings of study will help for long-term period follow-up study in the future. Along with clinical outcomes, patient satisfaction contributes an equal amount to the overall patient and surgical outcome. Therefore, the purpose of this study was to assess short-term patient satisfaction outcomes in TKA using weight-bearing long leg radiograph and OKS and KSS at the end of 6-month follow-up. Due to paucity of time, we could not continue follow-up for long term and did not come to conclusion about any deformity postoperatively but during a follow-up period of 6 months, we did not found any patient complaining of pain and deformity after TKA. our study (48.1) was in age group of 61–70 years, followed by 32.7% in age group of 51–60 years and 19.2% in >70 years of age. Mean age of study subjects was 64.33 ± 7.2 years and range of 5182 years. In our study, three-fourths (77%) were female and one fourth (23%) were male. Female-to-male ratio was 3:1. 52.11% had right side and 47.88% had left-sided TKA surgery. Most of the study (40.4%) subjects were overweight followed by 38.5% were obese and 21.2 were having normal BMI. In only 32.39% cases, distal femur valgus cut was taken as 6° rest of the cases (67.61%) had distal cut in range of 4–8°. Valgus cut 4° cut taken in 2.81%, 5° in 39.43%, 6° in 32.39%, 7° in 19.71%, and 8° in 5.63%. There was decrease in varus of lower limb after TKA surgery and this difference in varus before and after TKA was statistically significant (P < 0.05).There was decrease in FAMA after TKA surgery and this difference in FAMA before and after TKA with pre op 6 ± 0.9 and post op 5.8 ± 0.9 with mean difference of 1.2. Hence it was not statistically significant (P < 0.21). There was increase in OKS after TKA surgery and this difference in OKS before and after TKA was statistically significant (P < 0.05). There was increase in KSS after TKA surgery and this difference in KSS before and after TKA was statistically significant (P < 0.05).
In our study, we had taken variable degree of distal valgus cut according to pre op FAMA and neutral alignment achieved in 97% cases. Femoral component placement is accurate shown by improved femoral mechanical axis postoperatively. Similar result had shown by Lee et al., [26] Nam et al., [23], and Zhou et al., [24]. In general, coronal plane limb alignment within 2–3° around a neutral alignment. Despite clear limitations of the available scientific data, most surgeons believe that a neutral mechanical axis also confers a substantial advantage in terms of TKA implant survivorship [28]. Incorrect alignment can lead to abnormal wear [29,30], early mechanical loosening of the components [7,8], and patella-femoral problems [31]. Deviations of >3° varus or valgus will increase the rate of loosening in the coronal plane [5]. Huang et al., [32] reported that TKAs with a coronal alignment within 3° from the neutral axis had better function and quality of life at 5-year follow-up than TKAs that deviated more than 3° from neutral alignment. Magnussen et al., [33] found KSS to be better in patients with residual varus than in those with neutral alignment. In our study, we used OKS score to measure TKA outcome score in the present study. It was found that there was statistically significant improvement in the mean value of OKS in pre (15.88 ± 2.6) and post-operative (42.27 ± 2.5) follow-up (P < 0.05). It was found that there was statistically significant improvement in mean value of KSS in pre (33.42 ± 4.8) and post-operative (82.38 ± 2.8) follow-up (P < 0.05). Findings of our study though found significant difference in OKS score before and postoperatively but could not compare with existing literature due to short-term follow-up and no comparison group was studied but findings of study will help for long-term period follow-up study in the future. Along with clinical outcomes, patient satisfaction contributes an equal amount to the overall patient and surgical outcome. Therefore, the purpose of this study was to assess short-term patient satisfaction outcomes in TKA using weight-bearing long leg radiograph and OKS and KSS at the end of 6-month follow-up. Due to paucity of time, we could not continue follow-up for long term and did not come to conclusion about any deformity postoperatively but during a follow-up period of 6 months, we did not found any patient complaining of pain and deformity after TKA. our study (48.1) was in age group of 61–70 years, followed by 32.7% in age group of 51–60 years and 19.2% in >70 years of age. Mean age of study subjects was 64.33 ± 7.2 years and range of 5182 years. In our study, three-fourths (77%) were female and one fourth (23%) were male. Female-to-male ratio was 3:1. 52.11% had right side and 47.88% had left-sided TKA surgery. Most of the study (40.4%) subjects were overweight followed by 38.5% were obese and 21.2 were having normal BMI. In only 32.39% cases, distal femur valgus cut was taken as 6° rest of the cases (67.61%) had distal cut in range of 4–8°. Valgus cut 4° cut taken in 2.81%, 5° in 39.43%, 6° in 32.39%, 7° in 19.71%, and 8° in 5.63%. There was decrease in varus of lower limb after TKA surgery and this difference in varus before and after TKA was statistically significant (P < 0.05).There was decrease in FAMA after TKA surgery and this difference in FAMA before and after TKA with pre op 6 ± 0.9 and post op 5.8 ± 0.9 with mean difference of 1.2. Hence it was not statistically significant (P < 0.21). There was increase in OKS after TKA surgery and this difference in OKS before and after TKA was statistically significant (P < 0.05). There was increase in KSS after TKA surgery and this difference in KSS before and after TKA was statistically significant (P < 0.05).
In our study, as per FAMA, we had taken variable distal femoral valgus cut (4° cut in 2.81%, 5° in 39.43%, 6° in 32.39%, 7° in 19.71% and 8° in 5.63%). In majority of patient (97%), post-operative lower limb alignment was <3° varus. Only 3% had post-operative alignment was more than 3° varus. 3% cases that had alignment more than 3° varus were due to varus malalignment at tibia. Mechanical alignment of lower limb is better when distal femoral valgus cut is taken according to FAMA. The persistent varus deformity in the alignment of postoperative lower limb is due to result from varus in tibia. Preoperatively, the factors affecting FAMA are neck shaft angle, femoral bowing, and varus deformity which have significant correlation. In our study, we found that the short-term functional outcome and quality of life are significantly improved with correction of the mechanical axis to neutral as shown by improvement of KSS and OKS postoperatively. Various factors such as surgeon, kinematic alignment, BMI, knee loading, and environmental factors also play a role, but we could not study all those factors due to the short time duration.
Limitation
Small sample size and no comparison group to compare the superiority of alignment versus non-alignment group. Single-center, short-term follow-up study.
Study findings recommended that all patients for the primary TKA should be evaluated with long leg weight-bearing radiograph preoperatively to find lower limb alignment and FAMA. Intraoperatively distal femur valgus cut should be taken variable depending upon preoperatively evaluated FAMA.
References
- 1. Felson DT. Epidemiology of hip and knee osteoarthritis. Epidemiol Rev 1998;10:1-28. [Google Scholar] [PubMed]
- 2. Tennant A, Fear J, Pickering A, Hillman M, Cutts A, Chamberlain MA. Prevalence of knee problems in the population aged 55 years and over: Identifying the need for knee arthroplasty. BMJ 1995;310:1291-3. [Google Scholar] [PubMed]
- 3. Dorr LD, Boiardo RA. Technical considerations in total knee arthroplasty. Clin Orthop Relat Res 1986;205:5-11. [Google Scholar] [PubMed]
- 4. Scuderi GR, Insall JN, Windsor RE, Moran MC. Survivorship of cemented knee replacements. J Bone Joint Surg Br 1989;71B:798-803. [Google Scholar] [PubMed]
- 5. Ritter MA, Herbst SA, Keating EM, Faris PM, Meding JB. Long-term survival analysis of a posterior cruciate-retaining total condylar total knee arthroplasty. Clin Orthop 1994;309:136-45. [Google Scholar] [PubMed]
- 6. Callaghan JJ, O’rourke MR, Saleh KJ. Why knees fail: Lessons learned. J Arthroplasty 2004;19:31-4. [Google Scholar] [PubMed]
- 7. Tew M, Waugh W. Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg Br 1985;67:551. [Google Scholar] [PubMed]
- 8. Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br 1991;73:709-14. [Google Scholar] [PubMed]
- 9. Rivière C, Iranpour F, Auvinet E, Howell S, Vendittoli PA, Cobb J, et al. Alignment options for total knee arthroplasty: A systematic review. Orthop Traumatol Surg Res 2017;103:1047-56. [Google Scholar] [PubMed]
- 10. Whiteside A. Principles of ligament balancing and alignment in total knee. Arthroplasty. In: Javad Parvizi MF, editor. The Knee Reconstruction, Replace-Ment, and Revision, 1-2. United States: Data Trace Publishing Company; 2013. p. 2349-444. [Google Scholar] [PubMed]
- 11. Mahaluxmivala J, Bankes MJ, Nicolai P, Aldam CH, Allen PW. The effect of surgeon experience on component positioning in 673 press fit condylar posterior cruciate-sacrificing total knee arthroplasties. J Arthroplasty 2001;16:635-40. [Google Scholar] [PubMed]
- 12. Yau WP, Chiu KY, Tang WM, Ng TP. Coronal bowing of the femur and tibia in Chinese: Its incidence and effects on total knee arthroplasty planning. J Orthop Surg (Hong Kong) 2007;15:32-6. [Google Scholar] [PubMed]
- 13. Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 2002;404:7-13. [Google Scholar] [PubMed]
- 14. Gioe TJ, Killeen KK, Grimm K, Mehle S, Scheltema K. Why are total knee replacements revised?: Analysis of early revision in a community knee implant registry. Clin Orthop Relat Res 2004;428:100-6. [Google Scholar] [PubMed]
- 15. Subramanian SS, MoongilpattiSengodan M. Role of full length weight bearing radiograph in assessing the alignment in total knee arthroplasty. IOSR J Dent Med Sci 2016;15:55-63. [Google Scholar] [PubMed]
- 16. Deakin AH, Basanagoudar PL, Nunag P, Johnston AT, Sarungi M. Natural distribution of the femoral mechanical-anatomical angle in an osteoarthritic population and its relevance to total knee arthroplasty. Knee 2012;19:120-3. [Google Scholar] [PubMed]
- 17. Dunn HK, Goldberg VM, Krackow KA. Instructional course lectures. Primary total knee arthroplasty: Surgical technique and principles. In: American Academy of Orthopaedic Surgeons 68th Annual Meeting. San Francisco: American Academy of Orthopaedic Surgeons; p. 1-4. [Google Scholar] [PubMed]
- 18. Jiang CC, Insall JN. Effect of rotation on the axial alignment of the femur. Pitfalls in the use of femoral intramedullary guides in total knee arthroplasty. Clin Orthop Relat Res 1989;248:50-6. [Google Scholar] [PubMed]
- 19. Kharwadkar N, Kent RE, Sharara KH, Naique S. 5 degrees to 6 degrees of distal femoral cut for uncomplicated primary total knee arthroplasty: Is it safe? Knee 2006;13:57-60. [Google Scholar] [PubMed]
- 20. Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am 1987;69:745-9. [Google Scholar] [PubMed]
- 21. McGrory JE, Trousdale RT, Pagnano MW, Nigbur M. Preoperative hip to ankle radiographs in total knee arthroplasty. Clin Orthop Relat Res 2002;404:196-202. [Google Scholar] [PubMed]
- 22. Andrews SN, Beeler DM, Parke EA, Nakasone CK, Stickley CD. Fixed distal femoral cut of 6° valgus in total knee arthroplasty: A radiographic review of 788 consecutive cases. J Arthroplasty 2019;34:755-9. [Google Scholar] [PubMed]
- 23. Nam D, Vajapey S, Haynes JA, Barrack RL, Nunley RM. Does use of a variable distal femur resection angle improve radiographic alignment in primary total knee arthroplasty. J Arthroplasty 2016;9:91-6. [Google Scholar] [PubMed]
- 24. Zhou K, Ling T, Xu Y, Li J, Yu H, Wang H, et al. Effect of individualized distal femoral valgus resection angle in primary total knee arthroplasty: A systematic review and meta-analysis involving 1300 subjects. Int J Surg 2018;50:87-93. [Google Scholar] [PubMed]
- 25. Matsuda S, Miura H, Nagamine R, Urabe K, Harimaya K, Matsunobu T, et al. Changes in knee alignment after total knee arthroplasty. J Arthroplasty 1999;14:566-70. [Google Scholar] [PubMed]
- 26. Lee CY, Huang TW, Peng KT, Lee MS, Hsu RW, Shen WJ. Variability of distal femoral valgus resection angle in patients with end-stage osteoarthritis and genu varum deformity: Radiographic study in an ethnic Asian population. Biomed J 2015;38;350-5. [Google Scholar] [PubMed]
- 27. Shi X, Li H, Zhou Z, Shen B, Yang J, Pei F. Comparison of postoperative alignment using fixed vs individual valgus correction angle in primary total knee arthroplasty with lateral bowing femur. J Arthroplasty 2015;31:976-83. [Google Scholar] [PubMed]
- 28. Abdel MP, Oliver M, Parratte S, Trousdale RT, Berry DJ, Pagnano MW. Effect of postoperative mechanical axis alignment on survival and functional outcomes of modern total knee arthroplasties with cement: A concise follow-up at 20 years. J Bone Joint Surg Am 2018;100:472-8. [Google Scholar] [PubMed]
- 29. Laskin RS. The classic: Total condylar knee replacement in patients who have rheumatoid arthritis. A ten-year follow-up study. 1990. Clin Orthop Relat Res 2008;466:2589-96. [Google Scholar] [PubMed]
- 30. Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG. Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res 1994;299:31-43. [Google Scholar] [PubMed]
- 31. Figgie HE 3rd, Goldberg VM, Heiple KG, Moller HS 3rd, Gordon NH. The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Joint Surg Am 1986;68:1035-40. [Google Scholar] [PubMed]
- 32. Huang NF, Dowsey MM, Ee E, Stoney JD, Babazadeh S, Choong PF. Coronal alignment correlates with outcome after total knee arthroplasty: Five-year follow-up of a randomized controlled trial. J Arthroplasty 2012;27:1737-41. [Google Scholar] [PubMed]
- 33. Magnussen RA, Weppe F, Demey G, Servien E, Lustig S. Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clin Orthop Relat Res 2011;469:3443-50. [Google Scholar] [PubMed]










