Anterior tibial artery pseudoaneurysm, though rare after ankle arthroscopy, requires early recognition and multidisciplinary management to prevent morbidity.
Dr. João Murilo Magalhães, Department of Orthopaedics, Hospital Mater Dei, Belo Horizonte, MG, Brazil. E-mail: joaomurilo@hotmail.com
Introduction: Vascular complications after ankle arthroscopy (AA) are rare but potentially serious. Pseudoaneurysm (PA) formation, especially involving the anterior tibial artery, requires prompt diagnosis and management to avoid severe outcomes.
Case Report: We report a case of a 68-year-old obese, hypertensive male patient with a history of severe acute respiratory syndrome coronavirus 2 infection, who developed a rigid equinus deformity of the left ankle. He underwent Achilles tendon tenotomy and arthroscopic ankle arthrodesis. On post-operative day 23, he presented with a pulsatile mass in the anterolateral ankle region. Duplex Doppler ultrasound confirmed an anterior tibial artery PA. Surgical ligation of the artery proximal and distal to the lesion was successfully performed.
Conclusion: Although rare, PA formation following AA should be considered when patients present with pulsatile swellings postoperatively. Early diagnosis and surgical intervention are crucial to prevent serious complications.
Keywords: Pseudoaneurysm, anterior tibial artery, arthroscopic ankle arthrodesis, vascular complication, case report.
Iatrogenic complications of ankle arthroscopy (AA) occur in approximately 9–17% of cases, with nerve injuries being the most common [1]. Vascular complications during orthopedic surgery, although rare, do occur, with an estimated incidence of 0.008% [1]; however, this figure is likely underestimated due to the difficulty in obtaining an accurate diagnosis [2]. Differential diagnoses include deep vein thrombosis, hematoma, arteriovenous fistula, and soft-tissue tumors [3]. Most vascular complications occur intraoperatively, immediately postoperatively, or during the late post-operative period; they most commonly include lacerations, pseudoaneurysms (PAs), thrombosis, and arteriovenous fistulas. The surgical procedures most frequently associated with vascular injuries are knee arthroplasty, followed by hip arthroplasty, spinal surgery, and knee arthroscopy [4]. A PA or false aneurysm can occur when there is injury to all three layers of an artery, resulting in extravasation of blood and formation of a fibrous capsule containing blood flowing outside the lumen of the damaged vessel [5]. This lesion is characterized by the existence of a direct communication between the vascular lumen and the aneurysmal cavity, allowing blood to flow through the defect in the arterial wall [6]. The ankle is vascularized by three major arteries: Medially by the posterior tibial artery, anteriorly by the anterior tibial artery, and laterally by the fibular (peroneal) artery [2]. The anterior tibial artery is the most commonly affected vessel in vascular injuries and, consequently, in the formation of PAs. Due to its greater anatomical variability and its superficial location at the level of the ankle joint, it is more susceptible to direct trauma, particularly in penetrating injuries, which can result in rupture or damage to the arterial wall [7]. The timing of clinical presentation is variable, and early diagnosis is critical to establish appropriate management. Delayed diagnosis and treatment may lead to compressive neuropathy, hemarthrosis, and compartment syndrome [1]. If not properly addressed, a PA may rupture, causing hemorrhage and, in more severe cases, hemodynamic instability. The aim of this study is to report a case of anterior tibial artery PA following arthroscopic ankle arthrodesis, describing the patient’s clinical condition, diagnostic approach, and therapeutic management.
A 68-year-old male patient, a former smoker, obese with a body mass index of 41, and hypertensive, was diagnosed with severe acute respiratory syndrome coronavirus 2 infection in 2022, requiring prolonged hospitalization (45 days) in an intensive care unit. As an orthopedic sequela, he developed a rigid equinus deformity of the left ankle, resulting in impaired ambulation without the assistance of an ankle-foot orthosis with a heel wedge and a cane. After specialized orthopedic evaluation, surgical treatment consisting of Achilles tendon tenotomy and arthroscopic ankle arthrodesis was indicated. With the patient in the supine position under spinal anesthesia and sedation, the surgical procedure was performed in two stages: First, a posterior approach to the Achilles tendon approximately 4 cm proximal to its insertion was made, and, under direct visualization, the tenotomy was performed. Next, through standard anterolateral and anteromedial arthroscopic portals, anterior synovectomy and removal of the articular cartilage were carried out. Fixation for the ankle arthrodesis was achieved using three 6.5 mm diameter double-compression conical screws, all inserted medially (Fig. 1).

Figure 1: Fixation for the ankle arthrodesis.
The patient had an uneventful immediate post-operative course. However, on the 23rd post-operative day, he presented with a pulsatile swelling in the anterolateral region of the ankle (Fig. 2).

Figure 2: Pulsatile swelling in the anterolateral region of the ankle.
He was referred to the emergency department for vascular evaluation. Duplex Doppler ultrasound confirmed the diagnosis of a PA of the anterior tibial artery. The patient was admitted for surgical management, which consisted of ligation of the anterior tibial artery proximal and distal to the lesion (Fig. 3).
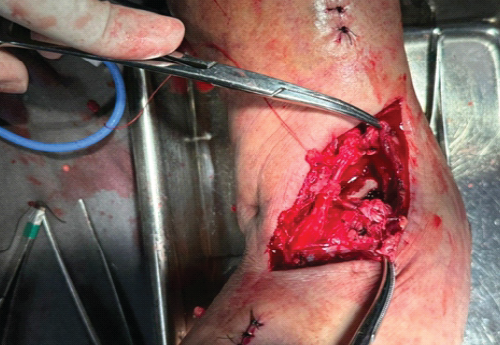
Figure 3: Ligation of the anterior tibial artery proximal and distal to the lesion.
After 3 weeks postoperatively, the patient returned for evaluation of the surgical wound and removal of stitches (Fig. 4).

Figure 4: Clinical image 3 weeks postoperatively.
PA is the most common vascular complication associated with AA. In a systematic review, 23 cases of PA secondary to AA were identified, with the procedures most frequently associated with this complication being anterior synovectomy and the excision of anterior ankle osteophytes [2]. The use of an accessory anterocentral portal is considered a risk factor due to the close anatomical proximity of the portal to the anterior tibial artery [8]. The higher incidence of anterior tibial artery PA can be explained by its anatomical course, characterized by its close relationship with the anterior capsule of the ankle at the level of the talar neck and its path beneath the superior and inferior extensor retinacula [9]. According to Lughi et al., vascular injuries may occur during portal creation, instrumentation through the portal, or joint manipulation [2]. However, in the present case, the exact cause of the PA could not be definitively established. Anatomical variations of the anterior tibial artery are also an important risk factor, with lateral or medial deviations reported in approximately 3.5–5.5% of the population [5]. To minimize the risk of such complications, careful portal placement guided by anatomical landmarks and avoidance of excessive lateral or medial deviation are recommended [10]. When PA develops secondary to AA, it typically does not present with immediate signs of vascular injury. Instead, it manifests days to weeks postoperatively, initially as a painful swelling that evolves into a pulsatile mass [11]. Literature reports indicate that the average time to diagnosis is approximately 50.45 days [6]. Imaging studies are crucial for diagnosis, particularly when physical examination findings are insufficient to exclude differential diagnoses. Imaging also assists in identifying the affected vessel and measuring the size of the lesion. Doppler ultrasonography is the most frequently utilized modality due to its lower cost, non-invasiveness, and lack of need for contrast agents [12]. Other diagnostic options include computed tomography angiography, catheter-based angiography, and magnetic resonance angiography, which may be used individually or in combination [2,12]. Several treatment modalities for PA have been described, with surgical repair remaining the most commonly employed approach [5,12]. Non-invasive treatments include external compression, ultrasound-guided compression, thrombin injection, endovascular embolization, and endovascular stenting. In this case, non-invasive approaches were not utilized due to the presence of a short and wide PA neck, which increases the risk of compression failure and arterial occlusion from thrombin injection or endovascular embolization. Furthermore, complete resection of the PA and adjacent soft tissues was indicated to minimize the risk of local infection due to skin compromise caused by the lesion. Although arterial resection followed by vascular reconstruction would have been the ideal treatment, the extent of longitudinal arterial injury necessitated resection of the PA with ligation of the anterior tibial artery. Distal perfusion of the foot was preserved through the posterior tibial and fibular (peroneal) arteries. In patients with a history of previous surgery, trauma, or atypical vascular pulsation, a pre-operative Doppler ultrasound or angiographic assessment may help identify vascular anomalies and guide safer portal positioning [10].
This study thus reports the case of a 68-year-old patient who developed a PA as a surgical complication following arthroscopic ankle arthrodesis. Although rare, this complication is potentially serious. Its variable time of presentation requires vigilance by the orthopedic surgeon and other healthcare providers involved in post-operative care. Close collaboration with vascular surgery teams is essential for the prompt diagnosis and appropriate management of these injuries. When suspected, PA should be rapidly confirmed and treated to reduce patient morbidity.
Anterior tibial artery pseudoaneurysm, although rare, is a potentially serious complication following AA or arthroscopic ankle arthrodesis. A thorough understanding of the vascular anatomy and careful identification of anatomical landmarks are essential to minimize risk. The safe zone for portal placement lies just medial to the peroneus tertius tendon for the anterolateral portal and just medial to the tibialis anterior tendon for the anteromedial portal. Excessive medial or lateral deviation should be avoided to prevent arterial or neural injury.
References
- 1. Yammine K, Kheir N, Daher J, Naoum J, Assi C. Pseudoaneurysm following ankle arthroscopy: A systematic review of case series. Eur J Orthop Surg Traumatol 2019;29:689-96. [Google Scholar] [PubMed]
- 2. Lughi M, Cevolani M, Testi G, Piraccini E, Lijoi F. Anterior ankle arthroscopy: Advantage of a preoperative ultrasound mapping to prevent neurovascular complications. J Ultrasound 2022;25:831-6. [Google Scholar] [PubMed]
- 3. Nair N, Suhania M. Anterior tibial artery pseudoaneurysm. Med J Malaysia 2021;76:429-31. [Google Scholar] [PubMed]
- 4. Rossi G, Mavrogenis A, Angelini A, Rimondi E, Battaglia M, Ruggieri P. Vascular complications in orthopaedic surgery. J Long Term Eff Med Implants 2011;21:127-37. [Google Scholar] [PubMed]
- 5. Tonogai I, Matsuura T, Iwame T, Wada K, Takasago T, Goto T, et al. Pseudoaneurysm of the anterior tibial artery following ankle arthroscopy in a soccer player. Case Rep Orthop 2017;2017:2865971. [Google Scholar] [PubMed]
- 6. Aimanan K, Lim SY, Mohd Nor MR, Wahi AM, Chew LG. Systemic review of global case reports on ankle pseudo aneurysm: Analysis of epidemiology, clinical presentation, diagnosis and treatment. Med J Malaysia 2020;75:88-93. [Google Scholar] [PubMed]
- 7. Huang H, Yang Z, Wang G, Zhang W. Pseudoaneurysm of the anterior tibial artery: A report of two cases. J Vascul Surg 2021;73:502-5. [Google Scholar] [PubMed]
- 8. Vascellari A, Malaguti C, Bortolami O, Russo A. Complications in ankle arthroscopy: Prevention and management. J Foot Ankle Surg 2019;58:245-50. [Google Scholar] [PubMed]
- 9. Nickisch F, Saltzman CL. Ankle arthroscopy: Anatomy, indications, and portal placement. Foot Ankle Clin 2015;20:499-514. [Google Scholar] [PubMed]
- 10. Son KH, Cho JH, Lee JW, Kwack KS, Han SH. Is the anterior tibial artery safe during ankle arthroscopy? Anatomic analysis of the anterior tibial artery at the ankle joint by magnetic resonance imaging. Am J Sports Med 2011;39:2452-6. [Google Scholar] [PubMed]
- 11. Brimmo OA, Parekh SG. Pseudoaneurysm as a complication of ankle arthroscopy. Indian J Orthop 2010;44:108-11. [Google Scholar] [PubMed]
- 12. Khatri K, Sharma V, Farooque K Pseudoaneurysm after orthopedic procedures: A systematic review. Orthop Traumatol Surg Res 2018;104:785-92. [Google Scholar] [PubMed]









