Consider atypical infections as cause for wrist extensor tenosynovitis.
Dr. Megan Newsom, Division of Plastic and Reconstructive Surgery, Virginia Commonwealth University, Richmond - 23223, Virginia, United States of America. E-mail: megan.newsom@vcuhealth.org
Introduction: This is the first reported case of Mycobacterium parascrofulaceum extensor tenosynovitis.
Case Report: A 79-year-old male presented with a left dorsal wrist mass that had been present for 8 months. Operative debridement and tenosynovectomy resulted in cultures positive for M. parascrofulaceum. His infection was successfully treated with a four drug anti-mycobacterial regimen.
Conclusion: Clinicians must maintain a high index of suspicion for atypical infection when treating extensor tenosynovitis that does not respond to standard treatment.
Keywords: Atypical mycobacteria, wrist extensor tenosynovitis, Mycobacterium parascrofulaceum.
Determining the cause of extensor tenosynovitis is not always straightforward. It is critical to correctly identify the cause because persistent tenosynovitis can lead to tendon rupture. [1] While extensor tenosynovitis is most commonly seen in patients with inflammatory arthritis, other causes have been reported [2]. Crystal arthropathies, sarcoidosis, amyloidosis, atypical infections, and other causes are documented [3,4,5]. Here, we discuss the first reported case of Mycobacterium parascrofulaceum extensor tenosynovitis and consider other rare infectious causes of extensor tenosynovitis. We identified all published case reports or case series of atypical infectious extensor tenosynovitis using a search in PubMed, PubMedCentral, and Web of Science using keywords and controlled vocabulary for extensor tenosynovitis and viral, parasitic, fungal, or bacterial infections. Studies were eligible if they included cases of infectious extensor tenosynovitis of the upper extremity. Studies were excluded if they were not in English, if they described non-human hosts, involved the lower extremities, or described isolated flexor tenosynovitis.
A 79-year-old male presented to our hand clinic in February 2024 for evaluation of a left dorsal hand mass (Fig. 1). Plain radiographs taken at presentation (Fig. 2 and 3) showed a small subchondral cyst and mild erosions at the distal radio-ulnar joint, along with the dorsal soft tissue swelling consistent with the clinical exam.

Figure 1: (a) Preoperative appearance of the left wrist at presentation shows a large dorsal soft tissue swelling. (b) Postoperative appearance of the left wrist.

Figure 2 & 3: Plain radiographs taken preoperatively show a small subchondral cyst and mild erosions at the distal radio-ulnar joint.
The lesion developed 8 months prior and had grown slowly. He was a retired oral and maxillofacial surgeon with an extensive international travel history of performing surgeries on medical missions. He had been diagnosed with bladder cancer and started chemotherapy just before the development of the mass. He did recall that a few months prior, he was walking on a wooded trail and a dog “nipped” his left wrist, resulting in a very small skin tear. He did not require any medical attention at that time. On physical examination, there was a painless cystic dorsal wrist mass, approximately 3 cm wide and 5 cm long. He was able to fully extend all his fingers. A point-of-care ultrasound was consistent with tenosynovitis involving the fourth dorsal wrist compartment. In March of 2024, he underwent excision of this lesion. A dorsal approach was made in line with the 3rd metacarpal, and a lobular synovial mass was encountered immediately under the skin. There were adhesions and synovitis of the 4th dorsal extensor compartment with fraying of up to 40% of the finger extensors. Multiple rice bodies and copious straw-colored fluid were also present. This fluid was sent for routine bacterial, acid-fast bacillus, and fungal cultures. The synovitis was excised and sent for surgical pathology. Routine bacterial Gram stain and acid-fast bacillus stains were negative. Fungal and routine bacterial cultures were negative for growth after 5 days of incubation. In early April of 2024, he was noted to have recurrent tenosynovitis. An inflammatory workup was negative for antinuclear antibodies, rheumatoid factor, and cyclic citrullinated protein antibodies. By May of 2024, the patient had ongoing tenosynovitis, confirmed with a point-of-care ultrasound. He was taken to the operating room for a tenosynovectomy and tissue culture. Six weeks postoperatively, an acid-fast bacillus culture, taken intraoperatively, grew M. parascrofulaceum. A musculoskeletal infectious disease specialist started the patient on anti-mycobacterial therapy: azithromycin 500 mg daily, rifampin 600 mg daily, and ethambutol 1200 mg daily with a plan to continue for 6 months. He is currently tolerating this antibiotic therapy well. His dorsal wrist swelling has improved, and he retains full extension of his fingers.
Infectious extensor tenosynovitis is uncommon and less urgent than infectious flexor tenosynovitis [6]. Infection results from direct inoculation, local spread, or hematogenous seeding [6]. Skin flora, Staphylococcus and Streptococcus species, are responsible for the majority of hand infections. While uncommon, mycobacteria are a reported cause of extensor tenosynovitis [7]. Mycobacterial extensor tenosynovitis is indolent and typically presents with painless dorsal wrist swelling [6]. The fourth dorsal wrist compartment is the most commonly affected area [8]. Inflammatory markers are not usually elevated in these infections, as was the case with our patient. Rice bodies may be seen on imaging and at the time of surgical debridement [9]. Treatment involves extensive tenosynovectomy with multi-drug antimycobacterial treatment for many months, often up to 1 year [6]. Distinguishing mycobacteria species is important because antibiotic susceptibility varies by species [10]. Most cases of mycobacterial extensor tenosynovitis in the literature are secondary to Mycobacterium tuberculosis or Mycobacterium marinum (Table 1).
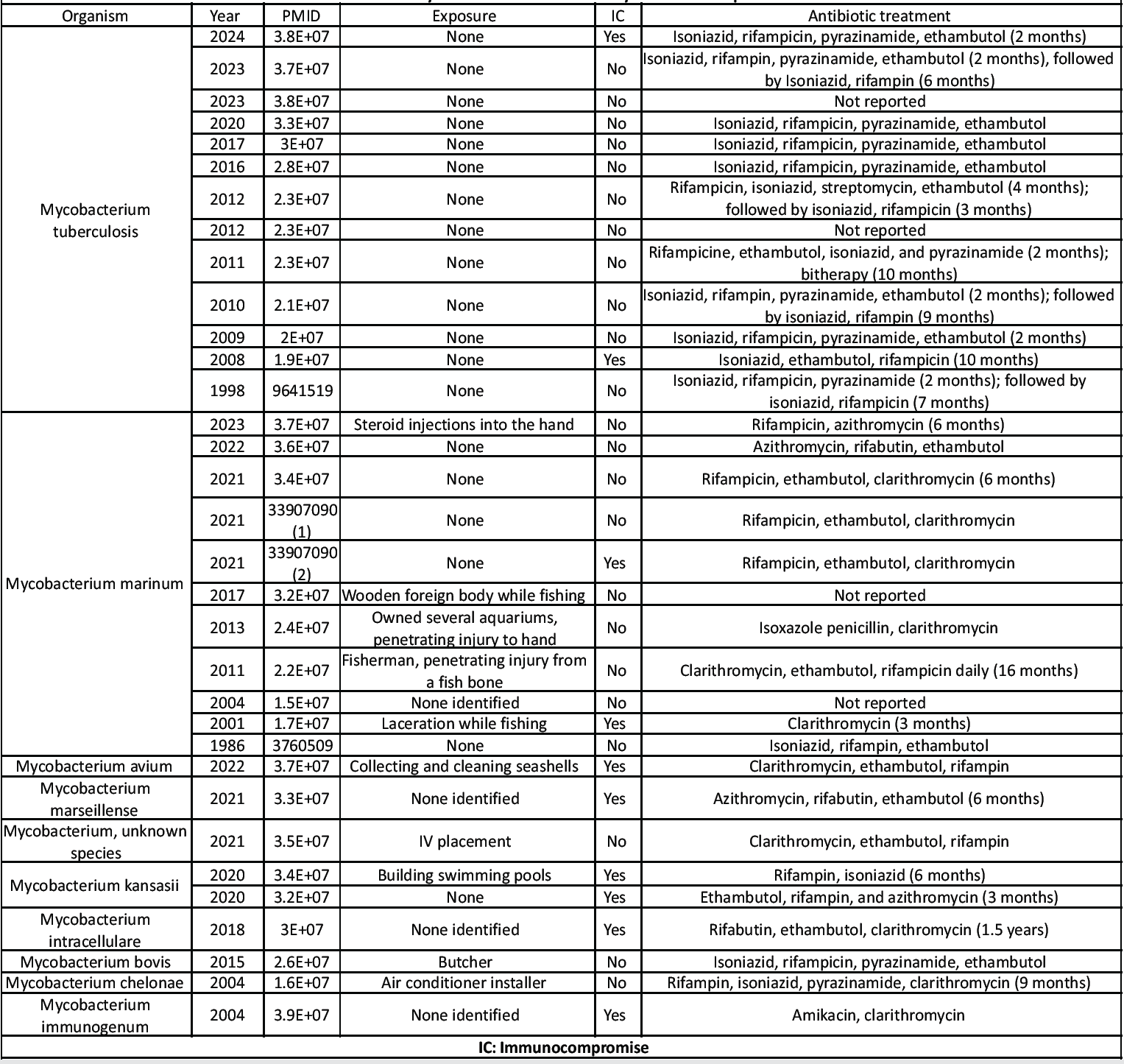
Table 1: Mycobacterial extensor tenosynovitis case reports
The causative agent in this case, M. parascrofulaceum, is a slow-growing non-tuberculous bacterium [10]. Infections caused by this organism are very rare, with only 10 case reports in the literature since its discovery in 2004 [11]. The majority of these are pulmonary, but cutaneous and genital infections have also been documented [11,12]. Health care workers exposed to the respiratory tract, like our patient, may have a higher risk of infection [13]. There are 15 case reports of non-mycobacterial extensor tenosynovitis in both immunocompromised and immunocompetent hosts [14,15]. This includes Gram-negative and Gram-positive organisms (Table 2, Table 3). A majority, four cases, are due to Neisseria gonorrhoeae. This organism is able to spread to the extensor compartment hematogenously, which may explain why tenosynovitis is seen in up to two-thirds of patients with disseminated gonococcal infections. Tenosynovitis may be the only evidence of disseminated disease in some patients [6]. There are 16 reported cases of fungal extensor tenosynovitis (Table 2). Parasitic and viral infections are much less commonly reported.

Table 2: Non -mycobacterial infectious extensor tenosynovitis case reports
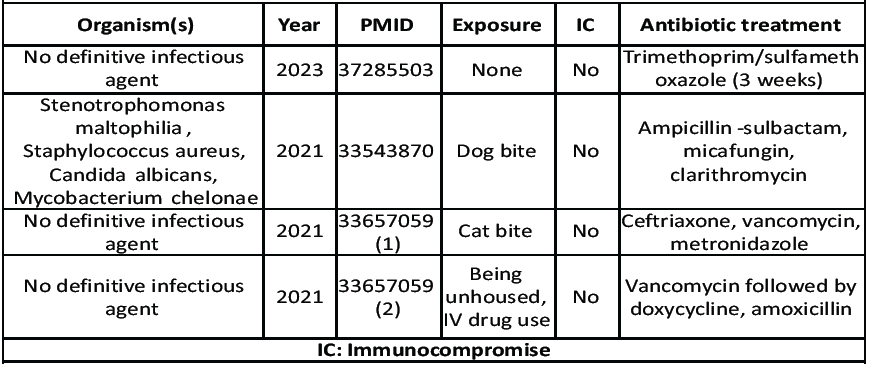
Table 3: Polymicrobial extensor tenosynovitis or no definitive infectious agent
It is critical to maintain a high index of suspicion for atypical infection when treating extensor tenosynovitis that does not respond to standard treatment. If a patient is immunosuppressed or has a high-risk exposure, atypical organisms should be considered.
This is the first reported case of a musculoskeletal infection secondary to M. parascrofulaceum.
References
- 1. Trieb K. Treatment of the wrist in rheumatoid arthritis. J Hand Surg Am 2008;33:113-23. [Google Scholar]
- 2. Blood TD, Morrell NT, Weiss AC. Tenosynovitis of the hand and wrist: A critical analysis review. JBJS Rev 2016;4:e7. [Google Scholar]
- 3. Lee DY, Eo S, Lim S, Yoon JS. Gouty tenosynovitis with compartment syndrome in the hand: A case report. World J Clin Cases 2023;11:7492-6. [Google Scholar]
- 4. Abdelshaheed ME, El-Shebly AM. Isolated sarcoid flexor or extensor tenosynovitis of the hand, wrist and distal forearm. Hand Surg Rehabil 2021;40:749-53. [Google Scholar]
- 5. Benito JR, Martinez I, Monner J, Paloma V, Castro V, Serra JM. Primary amyloidosis presenting as extensor tenosynovitis. Plast Reconstr Surg 1999;103:556-8. [Google Scholar]
- 6. Small LN, Ross JJ. Suppurative tenosynovitis and septic bursitis. Infect Dis Clin North Am 2005;19:991-1005, xi. [Google Scholar]
- 7. Newman ED, Harrington TM, Torretti D, Bush DC. Suppurative extensor tenosynovitis caused by Staphylococcus aureus. J Hand Surg Am 1989;14:849-51. [Google Scholar]
- 8. Hirase T, Le JT, Jack RA 2nd, Siff TE, Liberman SR. Extensor tenosynovitis due to Mycobacterium marseillense infection in a renal transplant recipient. J Am Acad Orthop Surg Glob Res Rev 2021;5:e20.00047. [Google Scholar]
- 9. Jeon CH, Kim TW, Park JY, Hwang CS, Lim S. Mycobacterium intracellulare tenosynovitis with rice body formation with literature review. Infect Chemother 2023;55:299-305. [Google Scholar]
- 10. Turenne CY, Cook VJ, Burdz TV, Pauls RJ, Thibert L, Wolfe JN, et al. Mycobacterium parascrofulaceum sp. Nov., Novel slowly growing, scotochromogenic clinical isolates related to Mycobacterium simiae. Int J Syst Evol Microbiol 2004;54:1543-51. [Google Scholar]
- 11. Shi J, Huang J, Yang D, Xiao L, Wang H. Successful application of ALA-PDT in rare cutaneous infection of Mycobacterium parascrofulaceum. Photodiagnosis Photodyn Ther 2023;43:103604. [Google Scholar]
- 12. Shojaei H, Hashemi A, Heidarieh P, Daei-Naser A. Chronic pelvic pain due to Mycobacterium parascrofulaceum in an Iranian patient: First report of isolation and molecular characterization from Asia. Braz J Infect Dis 2011;15:186-7. [Google Scholar]
- 13. Fnini S, Ouarab M, Rafai M, Cohen D, Largab A, Trafeh M. An uncommon occupational accident: Tuberculous tenosynovitis of the extensor tendons of the hand. Chir Main 1999;18:309-12. [Google Scholar]
- 14. Chan E, Bagg M. Atypical hand infections. Orthop Clin North Am 2017;48:229-240. [Google Scholar]
- 15. Osipchuk D, Riddell J. Bilateral infectious extensor tenosynovitis: A case report. Clin Pract Cases Emerg Med 2023;7:73-6. [Google Scholar]