Transverse humeral shaft fractures in the elderly are rare and biomechanically unstable. Locked intramedullary nailing, when combined with fracture-specific modifications such as careful entry point selection, minimal soft-tissue disruption, and balanced interlocking, ensures reliable fixation and facilitates early functional recovery.
Dr.Jeff Walter Rajadurai OR, Department of Orthopaedics, Madha Medical College and Research Institute, Chennai, Tamil Nadu, India. E-mail: jeffy.walter@gmail.com
Introduction: Humeral shaft fractures in elderly patients typically present as spiral or comminuted patterns due to age-related osteoporosis and low-energy mechanisms. A transverse midshaft fracture in this age group is quite uncommon and poses its own management challenges. Conservative approaches may be insufficient in such atypical cases.
Case Report: We report the case of an 80-year-old female who sustained an isolated transverse mid-diaphyseal humerus fracture following a low-energy fall. Given the instability of the fracture configuration and apprehensions regarding adherence to bracing, we elected for surgical fixation utilising a locked intramedullary nail. A minimally invasive antegrade nail was employed with a deltoid-sparing incision. The nail was aligned flush to prevent shoulder impingement. Proximal and distal interlocking screws were used at both ends to guarantee torsional stability in osteoporotic bone. The patient exhibited remarkable radiological union and achieved nearly full range of motion through early mobilization and physiotherapy.
Conclusion: This case highlights the successful management of an atypical fracture pattern in a geriatric patient through thoughtful surgical planning. Locked antegrade intramedullary nailing with attention to fracture-specific surgical nuances does provide a reliable solution in such uncommon scenarios.
Keywords: Humeral fractures, fracture fixation, intramedullary, treatment outcome, bone nails.
Fractures of the humeral shaft represent 1–3% of all skeletal injuries, with their incidence rising in elderly populations owing to age-related osteopenia and the growing burden of low-energy domestic falls [1,2]. In this demographic, the common radiographic patterns are spiral or comminuted fractures, reflecting both the fragility of cortical bone and the torsional forces typically involved. By contrast, a sharply transverse midshaft fracture in an octogenarian is rare. Its occurrence invites consideration of an atypical mechanism of injury or, less commonly, underlying pathology not apparent on initial imaging. Reports of such fracture configuration in an octogenarian remain sparse in the literature. This case highlights the clinical presentation and management of an 80-year-old woman who sustained an isolated transverse midshaft humeral fracture following a low-energy fall. The report underscores the unusual fracture pattern in a geriatric patient and outlines the surgical strategy adopted to achieve successful functional recovery.
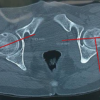
An 80-year-old right-hand dominant woman came to our clinic after a fall at home. She slipped while walking and landed squarely on her left arm. Pain was immediate and severe, and she was unable to raise the limb afterward. There was no loss of consciousness, seizure, or syncopal episode to suggest a systemic cause for the fall. Her medical history included well-controlled hypertension and early osteoarthritis of the knees. She had never sustained a fragility fracture and was not on corticosteroid therapy. On examination, she was comfortable, alert, and hemodynamically stable. The left arm showed diffuse swelling with a hint of angulation at the mid-arm level. The skin was intact, with no abrasions or breach. Palpation elicited marked tenderness over the midshaft of the humerus, with crepitus and abnormal mobility on gentle stress. Importantly, neurovascular assessment was intact – radial, median, and ulnar nerve functions were preserved, and both brachial and radial pulses were palpable. No features suggested a compartment compromise. Radiographs of the left humerus, in anteroposterior and lateral views, confirmed a sharply transverse mid-diaphyseal fracture (Fig. 1).
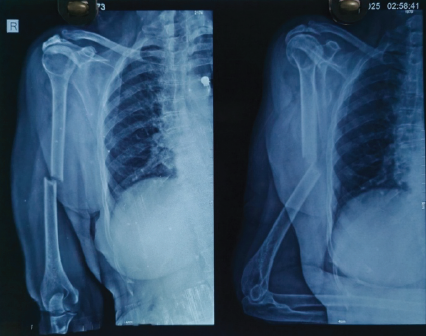
Figure 1: Pre-operative X-ray showing an atypical transverse fracture of midshaft
of humerus.
The fracture was clean, without comminution or extension into the joint. Cortical thinning consistent with osteopenia was noted, but there were no lytic lesions or features to suggest a pathological origin. The shoulder and elbow were normal on imaging. Given her age, the rare transverse configuration, and the limited biological potential of osteoporotic bone, surgical fixation was planned. After anesthetic evaluation and informed consent, we proceeded with antegrade locked intramedullary nailing under general anesthesia.
Intraoperative notes
The patient in beach-chair positioned on a radiolucent table with a small bolster beneath the scapula to extend the shoulder. Through a 3 cm anterolateral incision, the deltoid was gently split and the cuff divided in line with its fibers. The entry point was made at the apex of the humeral head just medial to the greater tuberosity, under fluoroscopic control (Fig. 2).
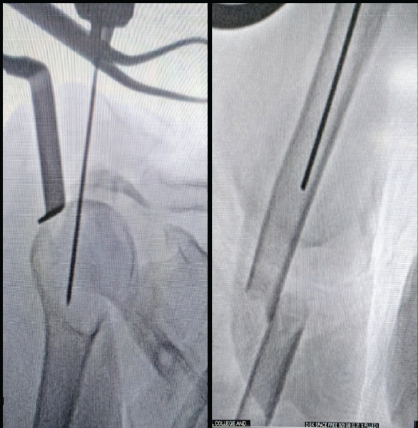
Figure 2: Entry was made at the apex of the humeral head just medial to the
greater tuberosity.
Reaming was carried out slowly and with low torque, to minimize the risk of cortical blowout in fragile bone. A nail of suitable length and diameter was introduced and its proximal end sunk flush with the articular surface, preventing impingement. Proximal fixation was secured with two divergent locking screws (Fig. 3). At the distal end, screws were placed in a single plane, a conscious choice to balance stability against the risk of excessive cortical perforation (Fig. 3).
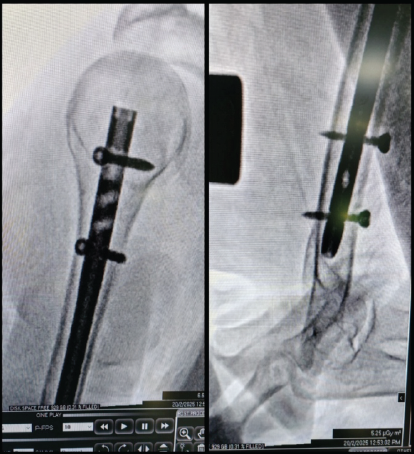
Figure 3: C-arm images showing the proximal and distal locking.
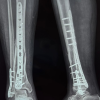
Reduction was confirmed fluoroscopically. Soft-tissue dissection was kept to the minimum required. The wound was thoroughly irrigated, hemostasis achieved, and the rotator cuff repaired carefully. The deltoid interval was closed, and sterile dressings were applied. Post-operative X-ray showed stable fixation (Fig. 4).
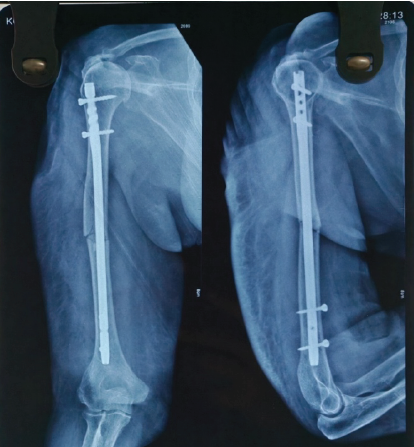
Figure 4: Immediate Post-operative X-ray showing nail in situ.
The patient was supported in a sling, and from the 1st post-operative day, she began elbow, wrist, and hand exercises. Passive shoulder mobilization was initiated on day 2. Regular dressing was done. Staples were removed on POD-14. Patient’s range of motion (ROM) improved progressively and attained nearly full ROM by 6th week postoperatively, and X-ray showed good bony union (Fig. 5).
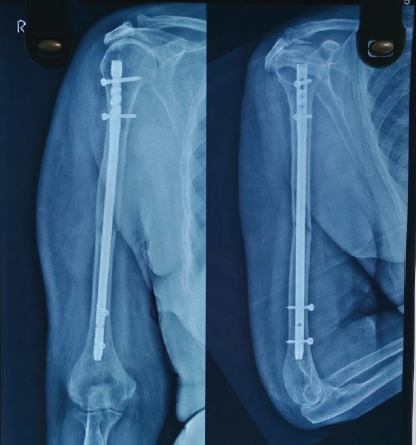
Figure 5: One month old post-operative X-ray showing good bone union.
Fractures of the humeral shaft are common enough, yet the way they present can be very different across age groups. In the younger patient, high-energy trauma is the usual culprit, and the patterns we encounter are often transverse or short oblique. Among the elderly, on the other hand, low-energy falls against a background of osteoporosis usually give rise to spiral or comminuted configurations [2,3]. For that reason, the sharply transverse fracture we observed in this octogenarian stood out as distinctly uncommon and required us to think beyond routine management. Bracing has always been an attractive option for these fractures. The work of Sarmiento established its value, and for many years it remained the default [4]. But while functional bracing can serve well in the right setting, it does not lend itself to every fracture type. Transverse patterns, in particular, are rotationally unstable and have been repeatedly shown to carry higher risks of delayed or non-union when left to conservative care [1]. In addition, the success of bracing relies on muscle tone and patient cooperation, both of which are often compromised in older individuals. Denard et al. [5] noted that surgical fixation generally delivers better outcomes, while the randomized FISH trial reinforced what most practicing surgeons already recognize – bracing may eventually catch up, but surgery restores function earlier, and in the elderly, those months of lost mobility can be devastating [6]. Once the decision is made to operate, the debate typically shifts between plating and nailing. Plates provide excellent stability, but they do so at the cost of a wide exposure, soft-tissue stripping, and a recognized risk of radial nerve palsy [7,8]. Contemporary data also show a steady drift toward intramedullary fixation, reflecting both surgeon preference and broader evidence [9]. Several reviews [10,3] suggest that unstable configurations, especially transverse fractures in older patients, are more reliably managed with surgical fixation rather than prolonged immobilization. Locked antegrade intramedullary nailing has gained ground because it preserves biology, reduces operative blood loss, and lowers the risk of infection [11,12,13]. Meta-analyses confirm that union rates are at least comparable to plating and, in many cases, superior [12,13]. Yet the technique is not without its pitfalls. Furuhata et al. [14] reminded us that poor cuff handling or a prominent nail can leave the patient with lasting shoulder dysfunction. For that reason, we were meticulous: The deltoid was spared, the cuff was split in line with its fibers and repaired carefully, and the nail was buried flush with the articular surface to prevent impingement. Osteoporotic bone always tests the surgeon’s judgment. In this case, reaming was performed with a deliberate, low-torque technique to avoid cortical blowout. Proximally, divergent screws were selected to maximize hold, while distally, we chose single-plane interlocking. Although biomechanical studies favor multiplanar locking, in fragile cortices, it can do more harm than good by creating stress risers. By limiting perforations, we struck a balance between stability and biological preservation [3,10]. This construct gave us the confidence to mobilize the patient early, a step that in itself may be as important as the fixation. Early movement prevented the cascade of pulmonary decline, deconditioning, and loss of independence that prolonged immobilization so often triggers [3,7]. Retrograde nailing was considered but set aside. Its value is clear in distal third fractures, but for a mid-diaphyseal pattern, it offers no distinct advantage. In fact, antegrade nails provide more predictable alignment and stability, and allow the procedure to be performed in the supine position – a safer and more practical choice for an elderly patient [11,15]. This case, then, is not simply about the rarity of a fracture pattern. It is about tailoring decisions to the individual in front of us. By selecting antegrade nailing over bracing or plating, avoiding retrograde entry, and applying a series of small but deliberate technical refinements, we achieved not just fracture union but meaningful restoration of function in an octogenarian who might otherwise have faced prolonged disability.
This case illustrates that atypical transverse humeral shaft fractures in the elderly can be successfully managed with locked intramedullary nailing when meticulous surgical technique is observed. Attention to key technical details, such as avoiding proximal nail prominence, employing a deltoid-sparing approach, and achieving dual interlocking fixation, significantly contributes to optimal outcomes in osteoporotic bone. Early mobilization further enhances recovery, making this approach both safe and effective in appropriately selected geriatric patients.
In osteoporotic elderly patients with atypical transverse humerus fractures, conservative treatment may be inadequate due to poor healing potential and fracture instability. Meticulous surgical technique using locked antegrade intramedullary nailing not only restores alignment but also preserves biology, reduces morbidity, and enables early mobilization thus paving the way for geriatric independency.
References
- 1. 1 Ekholm R, Tidermark J, Törnkvist H, Adami J, Ponzer S. Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma 2006;20:591-6. [Google Scholar] [PubMed]
- 2. 2 Tytherleigh-Strong G, Walls N, McQueen MM. The epidemiology of humeral shaft fractures. J Bone Joint Surg Br 1998;80:249-53. [Google Scholar] [PubMed]
- 3. 3 Gallusser N, Barimani B, Vauclair F. Humeral shaft fractures. EFORT Open Rev 2021;6:24-34. [Google Scholar] [PubMed]
- 4. 4 Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am 2000;82:478-86. [Google Scholar] [PubMed]
- 5. 5 Denard A Jr., Richards JE, Obremskey WT, Tucker MC, Floyd M, Herzog GA. Outcome of nonoperative vs operative treatment of humeral shaft fractures: A retrospective study of 213 patients. Orthopedics 2010;33(8):552 [Google Scholar] [PubMed]
- 6. 6 Rämö L, Sumrein BO, Lepola V, Lähdeoja T, Ranstam J, Paavola M, et al. Effect of surgery vs functional bracing on functional outcome among patients with closed displaced humeral shaft fractures: The FISH randomized clinical trial. JAMA 2020;323:1792-801. [Google Scholar] [PubMed]
- 7. 7 Carroll EA, Schweppe M, Langfitt M, Miller AN, Halvorson JJ. Management of humeral shaft fractures. J Am Acad Orthop Surg 2012;20:423-33. [Google Scholar] [PubMed]
- 8. 8 Shah JJ, Bhatti NA. Radial nerve paralysis associated with fractures of the humerus: A review of 62 cases. Clin Orthop Relat Res 1983;172:171-6. [Google Scholar] [PubMed]
- 9. 9 Schoch BS, Padegimas EM, Maltenfort M, Krieg J, Namdari S. Humeral shaft fractures: National trends in management. J Orthop Traumatol 2017;18:259-63. [Google Scholar] [PubMed]
- 10. 10 Daoub A, Oliveira Ferreira PM, Cheruvu S, Walker M, Gibson W, et al. Humeral shaft fractures: A literature review on current treatment methods. Open Orthop J 2022;16:1-10. [Google Scholar] [PubMed]
- 11. 11 Sharma GM, Bhardwaj AR, Shah S. Antegrade versus retrograde nailing in humeral shaft fractures: A prospective study. J Clin Orthop Trauma 2020;11(Suppl 1):S37-41. [Google Scholar] [PubMed]
- 12. 12 Wen H, Zhu S, Li C, Chen Z, Yang H, Xu Y. Antegrade intramedullary nail versus plate fixation in the treatment of humeral shaft fractures: An update meta-analysis. Medicine (Baltimore) 2019;98:e17952. [Google Scholar] [PubMed]
- 13. 13 Derbas J, Miclau T, Füchtmeier B. Outcomes of intramedullary nailing versus plate fixation for humeral shaft fractures: A systematic review and meta-analysis. Int Orthop 2025;49:351-63. [Google Scholar] [PubMed]
- 14. 14 Furuhata R, Tanji A, Nakamura S. Proximal nail protrusion is a risk factor for poor shoulder functional outcomes following antegrade intramedullary nailing of humeral shaft fractures. BMC Musculoskelet Disord 2024;25:102. [Google Scholar] [PubMed]
- 15. 15 Kumar D, Rajnish RK, Ranjan R. Antegrade vs retrograde intramedullary nailing in humeral shaft fractures: A comparative study. J Clin Orthop Trauma 2021;17:88-93. [Google Scholar] [PubMed]