This case highlights that bilateral quadriceps tendon rupture in a young patient, especially after inadequate trauma, can be the first presentation of an underlying systemic endocrine disorder, underscoring the critical link between orthopedics and endocrinology.
Dr. Karim Mustapha Naja, Department of Orthopedics, Trauma and Plastic Surgery, University Hospital Brandenburgan der Havel, Brandenburg, Germany. E-mail: k.naja@uk-brandenburg.de
Introduction: Bilateral quadriceps tendon rupture (BQTR) is rare and typically occurs in older adults or in the presence of systemic disease.
Case Report: A 30-year-old previously healthy male presented with acute inability to extend both knees after missing a step while descending stairs. Clinical examination and ultrasound confirmed complete BQTRs. Initial blood tests revealed hypercalcemia (value: 3.96 mmol/L; ref: 2.15–2.55) with normal renal function. Parathyroid hormone was elevated (1908 pg/mL; ref: 15–65). Neck magnet resonance imaging demonstrated a solitary hypoechoic nodule consistent with a parathyroid adenoma. The patient underwent bilateral tendon repair and parathyroidectomy during the same admission. Biochemical parameters normalized postoperatively, and the patient reported resolution of longstanding musculoskeletal aches.
Conclusion: In young patients with tendon rupture after minimal trauma, clinicians should consider metabolic and endocrine causes. Early identification and treatment of primary hyperparathyroidism can prevent further musculoskeletal injury and improve quality of life.
Keywords: Quadriceps tendon rupture, bilateral, primary hyperparathyroidism, parathyroid adenoma, metabolic bone disease.
Bilateral quadriceps tendon rupture (BQTR) is an uncommon injury, with a recent review identifying approximately 105 cases reported in the English and German literature. Primary hyperparathyroidism (PHPT) is a rare cause, historically accounting for only about 5% of simultaneous BQTR cases described between 1949 and 2002 [1,2]. Quadriceps tendon rupture typically occurs in older adults or individuals with predisposing risk factors such as chronic renal failure, gout, rheumatoid arthritis, prolonged corticosteroid use, or metabolic bone disease [2]. PHPT, most often due to a solitary parathyroid adenoma, results in excessive secretion of parathyroid hormone (PTH), leading to hypercalcemia, increased osteoclastic bone resorption, and compromised osteotendinous integrity [3,4]. Chronic hypercalcemia and altered collagen metabolism may weaken tendon attachment sites, predisposing to rupture even after minimal trauma [3]. This report describes the case of a young adult with no prior comorbidities who sustained BQTR after minimal trauma, which led to the diagnosis of PHPT due to a parathyroid adenoma.
A 30-year-old male of African ancestry, born in France, working as a delivery man, presented to the emergency department with acute bilateral knee pain and inability to extend his legs. The injury occurred while descending stairs; he missed a step with his left foot and avoided falling by a rapid transfer of weight to his right leg. He denied direct trauma, falls, or previous knee problems. On examination, there was suprapatellar swelling bilaterally, palpable defects above both patellae, and inability to perform a straight leg raise. Knee flexion was limited due to pain. Distal neurovascular examination was intact.
Laboratory results
- Serum calcium: 3.96 mmol/L (ref: 2.15–2.55)
- PTH: 1908 pg/mL (ref: 15–65)
- Alkaline phosphatase (ALP): 1388 U/L (ref: 40–129)
- Vitamin D: 15.5 nmol/L (ref: 25–250).
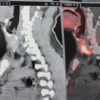
Imaging
Magnet resonance imaging confirmed in sagittal T2-weighted sequences bilateral total distal quadriceps tendon rupture at the patella insertion site (Fig. 1 and 2). A parathyroid adenoma was diagnosed in axial T2-weighted sequence (Fig. 3).
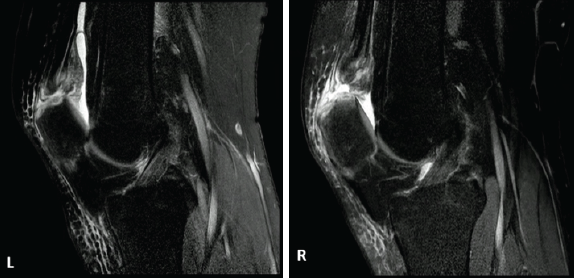
Figure 1, 2: Magnet resonance imaging of both knees showing complete rupture of both distal quadriceps tendons with proximal retraction.
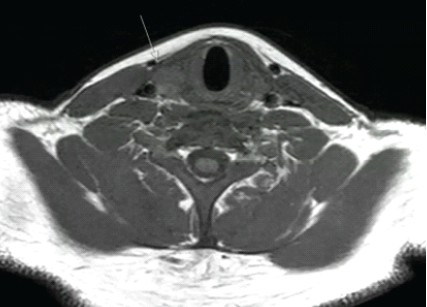
Figure 3: Magnet resonance imaging of the neck demonstrating a solitary hypoechoic nodule consistent with parathyroid adenoma.
Management
Bilateral quadriceps tendon repair was performed using transosseous sutures. During the same admission, a focused parathyroidectomy was performed, with histology confirming a parathyroid adenoma.
Outcome
Postoperatively, serum calcium and PTH levels normalized. At 6-month follow-up, the patient had regained full knee range of motion and strength, with no residual pain. Retrospective questioning revealed several months of generalized musculoskeletal aches prior to injury, which resolved completely after surgery.
BQTR is an uncommon event, with most reported cases occurring in older individuals or those with systemic comorbidities such as chronic renal insufficiency, gout, rheumatoid arthritis, or prolonged corticosteroid therapy [2]. The simultaneous rupture of both tendons in a young, otherwise healthy adult following minimal trauma is exceptionally rare. In the present case, the underlying cause was PHPT due to a solitary parathyroid adenoma. The pathophysiology of tendon rupture in PHPT is multifactorial. Chronically elevated PTH promotes osteoclastic bone resorption, particularly at the osteotendinous junction, where tendon integrity relies on strong mineralized anchorage [3,4]. Experimental and clinical data suggest that sustained PTH excess leads to structural weakening at the tendon–bone interface through several mechanisms. Chronic osteoclastic activity at the enthesis causes cortical bone resorption and subperiosteal thinning, reducing the mineralized anchor for tendon fibers [3]. At the same time, hypercalcemia and altered phosphate metabolism impair collagen synthesis and disrupt extracellular matrix organization, leading to reduced tensile strength of the tendon itself [5,6]. Secondary Vitamin D deficiency, often coexisting in PHPT, further compromises mineralization and muscle–tendon health [7]. The combination of osteotendinous junction fragility and intrinsic tendon degeneration explains why relatively trivial trauma may result in rupture in these patients [5,6]. A review of the literature reveals that fewer than 20 cases of tendon rupture as the first presentation of PHPT have been reported to date [1,2,8,9]. Soler and Giner also reported BQTR linked to PHPT [8], while Di Monaco et al. described a similar case in a relatively young patient [9]. Among reported cases, most occurred in middle-aged or older adults, often with additional comorbidities such as renal failure or parathyroid carcinoma. For example, Farrah et al. described simultaneous BQTR in association with parathyroid carcinoma, a much more aggressive endocrine disorder [1]. Shah, in an earlier series, noted PHPT as a rare but important risk factor for tendon rupture but primarily in patients with systemic disease [2]. Other authors have documented quadriceps tendon rupture in the setting of secondary hyperparathyroidism due to chronic renal failure [10]. In contrast, our patient was only 30 years old, had no other comorbidities, and presented with adenoma-driven PHPT as the sole precipitating factor. To the best of our knowledge, this makes him one of the youngest reported patients in the literature to present with BQTR as the initial manifestation of PHPT. From a clinical standpoint, this case highlights several important considerations. First, bilateral tendon rupture after low-energy trauma should immediately raise suspicion for systemic disease. A simple set of laboratory tests – including serum calcium, phosphate, ALP, and PTH – can rapidly uncover an endocrine or metabolic cause. Early recognition of PHPT is crucial, as delayed diagnosis not only predisposes patients to musculoskeletal complications but may also increase the risk of nephrolithiasis, neurocognitive impairment, and cardiovascular morbidity if untreated [3,4]. Second, management requires a dual approach: Surgical repair of the tendon injury to restore function and definitive treatment of the endocrine disorder to prevent recurrence. Our patient underwent successful bilateral tendon repair followed by parathyroidectomy in the same admission, with normalization of biochemical parameters and excellent functional recovery. Importantly, retrospective history revealed longstanding musculoskeletal aches that completely resolved after parathyroidectomy, reinforcing the systemic impact of PHPT on quality of life. Finally, this case underscores the value of preventive screening. Routine measurement of serum calcium is inexpensive and may allow diagnosis of PHPT at an earlier stage, before catastrophic musculoskeletal injuries occur. For orthopedic surgeons, awareness of this rare but important association is critical, as recognizing the systemic cause can change long-term outcomes [4].
While rare, PHPT should be considered in the differential diagnosis of tendon rupture in young patients, particularly when bilateral or associated with minimal trauma. Prompt diagnosis and surgical management of both the tendon injury and the underlying parathyroid pathology can result in excellent functional recovery and resolution of systemic symptoms.
Young patients presenting with tendon rupture after trivial trauma should prompt clinicians to search for systemic causes. Simple laboratory tests such as serum calcium and PTH can uncover PHPT. Timely diagnosis and combined surgical management of both the tendon injury and the endocrine disorder ensure excellent recovery and prevent recurrence.
References
- 1. Farrah JP, Zirgibel BJ, Zapata CA, Wong AM. Simultaneous bilateral quadriceps tendon rupture secondary to parathyroid carcinoma: A case report. J Am Acad Orthop Surg Glob Res Rev 2023;7:e23. [Google Scholar] [PubMed]
- 2. Shah MK. Simultaneous bilateral rupture of quadriceps tendons: Analysis of risk factors and associations. South Med J 2002;95:860-6. [Google Scholar] [PubMed]
- 3. Silverberg SJ, Shane E, Jacobs TP, Siris E, Gartenberg F, Bilezikian JP. A 10-year prospective study of primary hyperparathyroidism with or without parathyroid surgery. N Engl J Med 1999;341:1249-55. [Google Scholar] [PubMed]
- 4. Bilezikian JP, Brandi ML, Eastell R, Silverberg SJ, Udelsman R, Marcocci C, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: Summary statement from the fourth international workshop. J Clin Endocrinol Metab 2014;99:3561-9. [Google Scholar] [PubMed]
- 5. Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am 1991;73:1507-25. [Google Scholar] [PubMed]
- 6. McDonald HM, Nordin BE. Spontaneous tendon ruptures in hyperparathyroidism. Br Med J 1965;1:1034-6. [Google Scholar] [PubMed]
- 7. Dzik KP, Kaczor JJ. Mechanisms of vitamin D on skeletal muscle function: Oxidative stress, energy metabolism, and anabolic State. Eur J Appl Physiol 2019;119:825-39. [Google Scholar] [PubMed]
- 8. Soler R, Giner J. Bilateral spontaneous quadriceps tendon rupture associated with primary hyperparathyroidism. Clin Imaging 1998;22:422-5. [Google Scholar] [PubMed]
- 9. Di Monaco M, Vallero F, Tappero R, Cavanna A. Primary hyperparathyroidism presenting as simultaneous bilateral rupture of the quadriceps tendon: A case report and review of the literature. J Orthop Traumatol 2006;7:103-6. [Google Scholar] [PubMed]
- 10. Lotem M, Bernheim J, Conforty B. Simultaneous rupture of both quadriceps tendons in a patient with chronic renal failure and secondary hyperparathyroidism. Ann Rheum Dis 1978;37:174-6. [Google Scholar] [PubMed]