Simultaneous bilateral posterior elbow dislocations with bilateral distal radius fractures are extremely rare and require early recognition, staged surgical fixation, and structured rehabilitation for optimal functional recovery.
Dr. Bharat Kumar Soni, Department of Orthopaedics, All India Institute of Medical Sciences, Marudhar Industrial Area, 2nd Phase, M.I.A. 1st Phase, Basni, Jodhpur - 342005, Rajasthan, India. E-mail: bsoni9863@gmail.com
Introduction: Distal radius fractures and elbow dislocations are commonly encountered as isolated injuries. However, bilateral simultaneous occurrence is exceedingly rare, typically linked with high-energy trauma. Such injury combinations require prompt diagnosis and an individualized management strategy.
Case Report: We report a case of a 42-year-old male laborer who sustained bilateral distal radius fractures (AO/OTA 23-C2) with simultaneous posterior dislocation of both elbow joints following a fall from approximately 10 feet. The elbow dislocations were managed with immediate closed reduction. Definitive fixation of both distal radius fractures was performed using volar locking plates. At the 12-month follow-up, the patient achieved good functional recovery and returned to manual work with minor limitations.
Conclusion: Bilateral elbow dislocations with simultaneous distal radius fractures are extremely rare. Prompt recognition, appropriate surgical intervention, and structured rehabilitation are essential to restore function and prevent long-term disability.
Keywords: Bilateral distal radius fracture, elbow dislocation, high-energy trauma, volar plate, upper limb injury.
Fractures of the distal radius are the most commonly encountered injuries of the upper limb, particularly in individuals who experience a fall on an outstretched hand (FOOSH) mechanism [1]. Elbow dislocations, which comprise approximately 10–25% of all elbow injuries, are the second most frequent large joint dislocations in adults, following those of the shoulder [2]. While each of these injuries is well documented in isolation, the simultaneous and bilateral occurrence of both distal radius fractures and elbow dislocations is exceptionally rare and scarcely reported in the literature. Such complex injury patterns typically arise from high-energy trauma, including falls from height, high-velocity road traffic accidents, or electrical injuries. The force transmission during these events causes axial loading through the forearm, resulting in fractures and joint disruption. Given their rarity and often atypical presentation, these injuries may be initially overlooked in the context of polytrauma, potentially delaying critical interventions [3,4]. Timely recognition and management require a systematic clinical evaluation, prompt imaging, and coordinated multidisciplinary care. Furthermore, due to the functional complexity of the upper limb, treatment must be tailored to the patient’s functional demands, emphasizing both anatomical reconstruction and early rehabilitation to optimize long-term outcomes.
Patient presentation
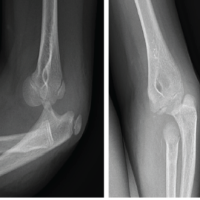
A 42-year-old right-handed male construction worker fell from a scaffold approximately 10 feet high. He landed with both arms outstretched and elbows extended. Upon presentation, the patient had gross deformity, pain, and swelling at both wrists and elbows. Upon inspection, deformities were seen on both wrists and elbows bilaterally. On examination, tenderness was found with a limited range of motion. Neurovascularity was intact in both upper limbs. X-rays revealed bilateral posterior elbow dislocation without associated fracture (Fig. 1a, b, c, d) and bilateral comminuted intra-articular distal radius fractures (AO 23-C2). (Fig. 2a, b, c, d). In the emergency setting, both elbow dislocations were promptly managed with closed reduction under sedation, and concentric reduction was confirmed on post-reduction radiographs (Fig. 3a, b, c, d). Both wrists were also reduced, and stabilization was done with slab application (Fig. 4a, b, c, d). Following initial stabilization and resolution of soft tissue swelling, the patient underwent staged open reduction and internal fixation of the bilateral distal radius fractures using a volar approach (modified Henry technique). Fixation was achieved using volar locking compression plates for both wrists (Fig. 5a, b, c, d).
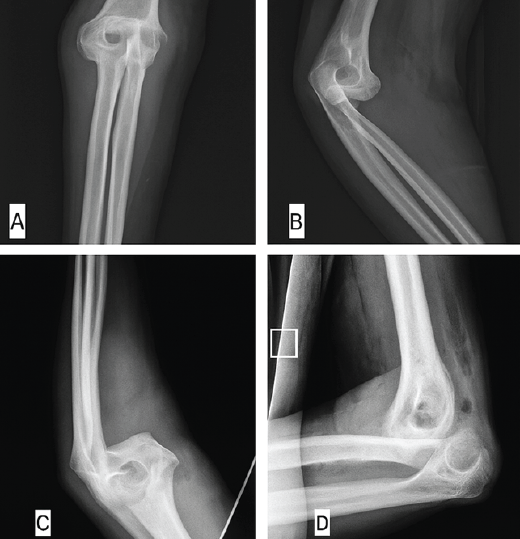
Figure 1: X-rays showing posterior dislocation of the right elbow without any fracture in anteroposterior (a) and lateral (b) view and left elbow showing posterior dislocation of elbow without any fracture in anteroposterior (c) and lateral (d) view.

Figure 2: Wrist X-rays showing comminuted intra-articular distal radius fractures (AO 23-C2) right side in anteroposterior (a) and lateral (b) and left side anteroposterior (c) and lateral (d) view.
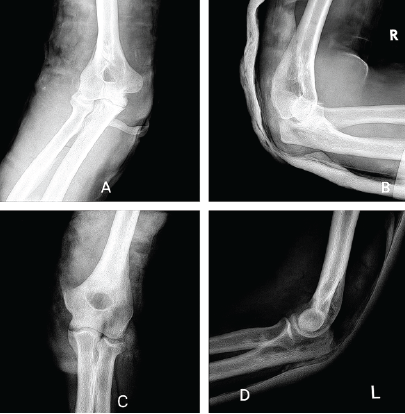
Figure 3: Post-reduction X-rays of the right elbow in anteroposterior (a) and lateral (b) view and left elbow in anteroposterior (c) and lateral (d) view.
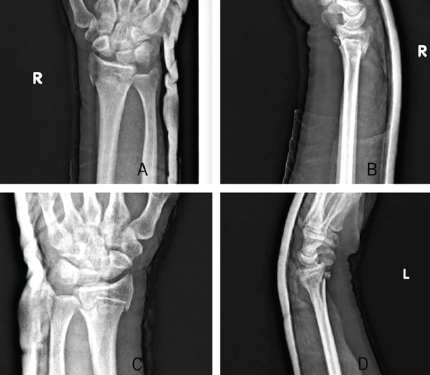
Figure 4: `-reduction X-rays of right wrist in anteroposterior (a) and lateral (b) view and left wrist in anteroposterior (c) and lateral (d) view.

Figure 5: Post-op X-rays showing appropriate reduction and fixation of the right wrist in anteroposterior (a) and lateral (b) view and left wrist in anteroposterior (c) and lateral (d) view.
Postoperatively, bilateral below-elbow slabs were applied for 10 days. Sutures were removed on the 14th post-operative day, and a structured rehabilitation protocol was initiated with early wrist and elbow mobilization from the 2nd week, followed by progressive strengthening under supervised physiotherapy beginning at 6 weeks. At the 12-month follow-up, the patient demonstrated excellent radiological and functional outcomes. (Table1).
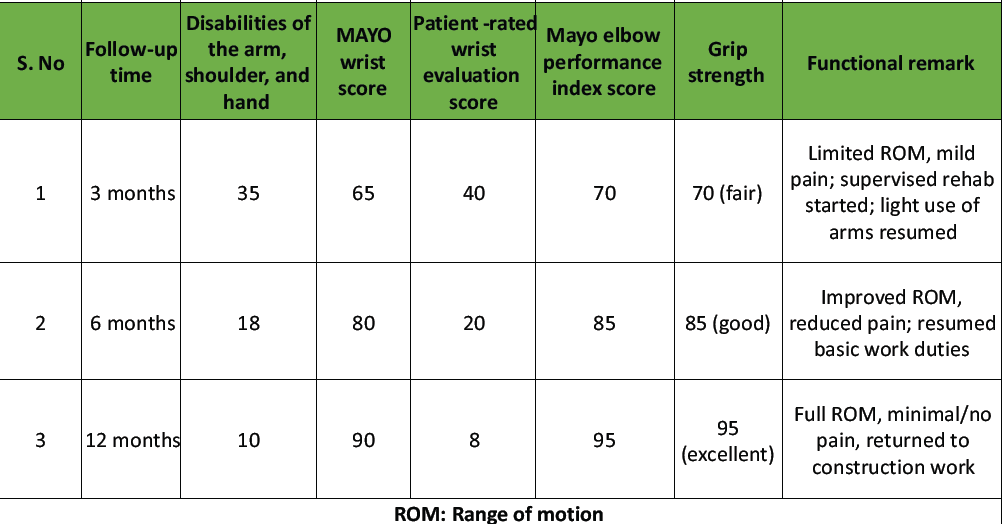
Table 1: Functional outcome scores at 3, 6, and 12 months
Radiographs confirmed complete bony union with proper implant positioning and anatomical alignment in both wrists (Fig. 6a, b, c, d). Functionally, the patient achieved elbow flexion from 0° to 130°, wrist flexion and extension of 60° and 60°, respectively, and full pronation and supination of 80° each (Fig. 7). He had successfully returned to his occupation as a laborer.

Figure 6: 6-month follow-up X-rays showing bony union of right wrist fracture in anteroposterior (a) and lateral (b) view, and left wrist fracture in anteroposterior (c) and lateral (d) view.

Figure 7: 12-month follow-up clinical image showing elbow flexion of 130° (a), wrist extension of 60° (b), wrist flexion of 60° (c), supination of 80° (d), and pronation of 80° (e).
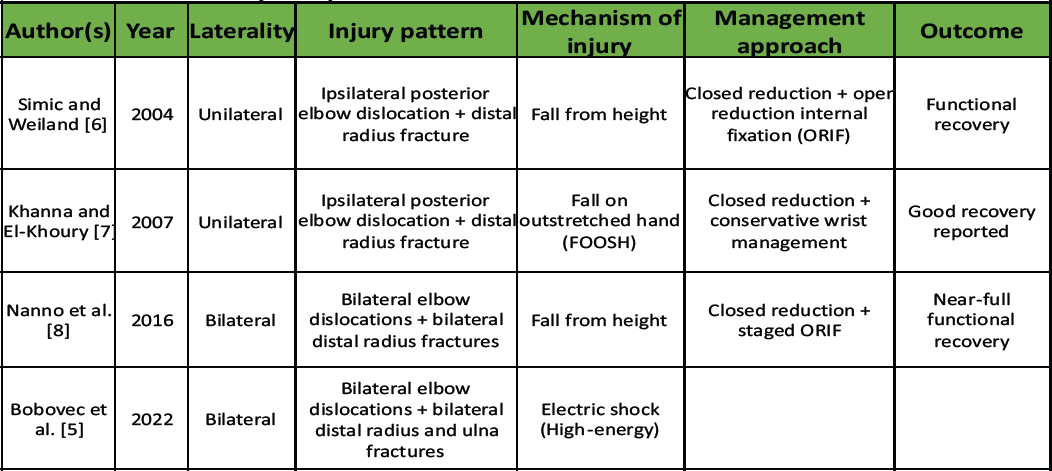
Table 2: Summary of reported cases of elbow dislocation with distal radius fracture
This case report presents an exceptionally rare clinical scenario: bilateral posterior elbow dislocations occurring simultaneously with bilateral distal radius fractures as a result of a high-energy fall. Individually, distal radius fractures and elbow dislocations are frequently encountered in trauma practice. Distal radius fractures account for up to 18% of adult fractures, often following a FOOSH [1], while posterior elbow dislocations are the most common type of elbow dislocation [2]. However, the simultaneous bilateral presentation of these injuries is almost unheard of and adds significant complexity to both diagnosis and management. The mechanism of injury here is classic: A FOOSH event in which extended elbows transmitted axial loading proximally through the arm to the wrist, resulting in comminuted intra-articular distal radius fractures and forcing the elbow out of its normal alignment posteriorly [3,4]. Bilateral symmetry suggests that both upper extremities bear near-equal loads—a pattern seen in falls where instinctive and effective protection with one arm is lacking [5]. Literature regarding concurrent injuries has largely focused on unilateral presentations. For instance, Mehlhoff et al. analyzed proximal and distal injuries in elbow dislocations, noting fractures of the radial head and neck but rarely addressing distal radius involvement. (Table 2). Given its unusual presentation, a thorough clinical and radiographic evaluation was paramount. The presence of multiple injuries can obscure symptoms, particularly swelling at the wrist that masks elbow deformity. As recommended by Mauffrey et al., imaging should cover the entire upper limb – shoulder to wrist – in any high-energy trauma scenario [9]. Prompt recognition ensured early closed reduction under sedation, which restored joint alignment and minimized risks of neurovascular damage, cartilage injury, and heterotopic ossification [10,11,12]. Treatment of the bilateral distal radius fractures followed established guidelines by Orbay and Fernandez [13], utilizing volar locked compression plating through a modified Henry approach. This technique is widely recognized as superior for intra-articular and comminuted fractures, offering stable fixation, anatomic restoration, and an expedited rehabilitation timeline [14,15,16]. In our case, a bilateral radius fracture was fixed with a volar compression plate. Multiple meta-analyses support early functional superiority of volar plates compared to casting, though complications including hardware irritation, tendon disruption, and carpal tunnel syndrome are non-negligible, occurring in approximately 12% of cases [17,18,19]. A staged surgical strategy was employed to reduce operative time per session, manage soft tissue swelling effectively, and optimize patient tolerance, critical factors in bilateral limb injuries. Fresh tissue trauma can complicate simultaneous bilateral fixation, so spacing procedures are allowed for better outcomes. The rehabilitation protocol was meticulously timed. Early elbow motion is key to preventing stiffness; studies show that immobilization beyond 3 weeks significantly increases the risk of restricted range and poor functional results [20,21]. In our patient, controlled active-assisted motion was started during the 2nd post-operative week, with gradual strengthening from week 6 onward. A 2024 scoping review by van der Vliet et al. emphasized that, when addressing determinants of outcome after volar plating, early movement and targeted physiotherapy are associated with significantly improved functional scores [22]. By 3 months, the patient had regained nearly full functional range—elbow flexion-extension from 10° to 130°, wrist flexion-extension of over 60°. At 12 months, a return to manual labor was imperative, mirroring the favorable recovery described by Bobovec et al. in their 2022 follow-up [5]. Finally, while exceedingly rare, such injury patterns must be recognized and addressed using standardized trauma protocols balanced with tailored surgical and rehabilitative strategies. This case enhances the body of knowledge on complex bilateral upper limb trauma and underscores the potential for excellent functional outcomes with coordinated, evidence-based treatment planning.
Clinical significance
This case offers critical lessons:
- Vigilance for rare combinations: Any trauma patient with bilateral upper limb deformity should undergo full-length imaging.
- Staged fixation is effective: Prioritizing dislocation reduction followed by internal fixation allows compartmentalized management.
- Rehabilitation drives outcome: Early and aggressive mobilization post-fixation is crucial in regaining near-complete function.
Bilateral elbow dislocation combined with distal radius fractures is a rare yet serious upper limb injury requiring prompt recognition. A structured treatment plan involving early dislocation reduction, surgical fixation, and timely rehabilitation can lead to excellent outcomes. High clinical suspicion and comprehensive evaluation are key, especially in high-energy trauma.
High-energy upper limb trauma can result in atypical bilateral injury patterns. Prompt recognition, early reduction, and surgical stabilization, followed by structured rehabilitation, lead to optimal recovery in complex cases involving bilateral elbow dislocation and distal radius fractures.
References
- 1. Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury 2006;37:691-7. [Google Scholar] [PubMed]
- 2. Mehlhoff TL, Noble PC, Bennett JB, Tullos HS. Simple dislocation of the elbow in the adult. J Bone Joint Surg Am 1988;70:244-9. [Google Scholar] [PubMed]
- 3. Jupiter JB. Current concepts review: Fractures of the distal end of the radius. J Bone Joint Surg Am 1991;73:461-9. [Google Scholar] [PubMed]
- 4. Van der Linden W, Ericson R. Colles’ fracture: how should its displacement be measured and how should it be immobilized? J Bone Joint Surg Am. 1981;63(8):1285–8. [Google Scholar] [PubMed]
- 5. Bobovec D, Rajačić D, Žigman T, Dobrić I. Good functional recovery after bilateral elbow dislocation associated with bilateral distal radius and ulna fractures. Clin Case Rep 2022;10:e05439. [Google Scholar] [PubMed]
- 6. Simic PM, Weiland AJ. Elbow dislocation with ipsilateral distal radius fracture: A case report. J Trauma 2004;56:721-3. [Google Scholar] [PubMed]
- 7. Khanna G, El-Khoury GY. Posterior elbow dislocation with ipsilateral distal radius fracture. Emerg Radiol 2007;13:153-5. [Google Scholar] [PubMed]
- 8. Nanno M, Kodera N, Tomori Y, Takai S. Bilateral elbow dislocations and bilateral distal radius fractures: A case report. J Med Case Rep 2016;10:197. [Google Scholar] [PubMed]
- 9. Mauffrey C, Herbert B, Young H, Wilson ML, Hake M. The role of routine radiographs in evaluation of upper extremity trauma. Injury 2015;46:1211-5. [Google Scholar] [PubMed]
- 10. Anakwenze OA, Kwon D, O’Donnell E, Levine WN, Ahmad CS. Simple elbow dislocations: evaluation and management. J Am Acad Orthop Surg. 2014;22(6):325–35. [Google Scholar] [PubMed]
- 11. López-López D, Alaminos D, López-López MI, Gómez-Hurtado I, Romero-Morales C. Functional results of early rehabilitation after elbow dislocations. J Shoulder Elbow Surg. 2018;27(6):1083–90 [Google Scholar] [PubMed]
- 12. Lindenhovius AL, Jupiter JB. The posttraumatic stiff elbow: A review of the literature. J Hand Surg Am 2007;32:1605-23. [Google Scholar] [PubMed]
- 13. Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: A preliminary report. J Hand Surg Am 2002;27:205-15. [Google Scholar] [PubMed]
- 14. Drobetz H, Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop 2003;27:1-6. [Google Scholar] [PubMed]
- 15. Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg Am 2006;88:2687-94. [Google Scholar] [PubMed]
- 16. Jeudy J, Steiger V, Boyer P, Cronier P, Bizot P, Massin P. Locked volar plating vs external fixation for complex distal radius fractures. Injury 2012;43:174-9. [Google Scholar] [PubMed]
- 17. Lee JH, Lee JK, Park JS, Kim DH, Baek JH, Kim YJ, et al. Complications associated with volar locking plate fixation for distal radius fractures in 1955 cases: A multicentre retrospective study. Int Orthop 2020;44:2057-67. [Google Scholar] [PubMed]
- 18. Jayaram M, Sohal KS, Harper C, Lacey AE, Magnusson J, Costa ML. 24-month outcomes after treatment for distal radial fractures. JAMA Netw Open. 2023;6(6):e2318715. [Google Scholar] [PubMed]
- 19. Oldrini G, Marinoni EC, Riccio M, Malerba F, Bertozzi G, Marongiu G. Functional outcomes in elderly distal radius fractures: volar locking plate versus casting. J Orthop Surg Res. 2024;19:52. [Google Scholar] [PubMed]
- 20. Morrey BF. Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone Joint Surg Am 1990;72:601-18. [Google Scholar] [PubMed]
- 21. Mehlhoff TL, Noble PC, Bennett JB, Tullos HS. Rehabilitation of elbow injuries. J Bone Joint Surg Am 1988;70:244-9. [Google Scholar] [PubMed]
- 22. Van der Vliet QM, Van Dijk A, Janssen SJ, Ring D, Chen NC. Scoping review: factors influencing function after volar locking plate fixation. Scand J Hand Ther. 2024;29(1):7–15. [Google Scholar] [PubMed]