Open clavicle fractures can be definitively treated with external fixation using LCP, as a single effective procedure offering good functional and radiological outcome.
Dr. Amaresh Cadapa Prahallad, Department of Orthopaedics, Bangalore Medical College and Research Institute, Bengaluru, Karnataka, India. E-mail: amareshprahallad@gmail.com
Introduction: Open clavicle fracture is an uncommon injury caused by severe direct trauma. In situations of bony exposure, significant contamination, and severe soft-tissue damage, external fixation is the treatment of choice as it provides stable fixation with minimal local tissue damage resulting in excellent union rates and better soft-tissue outcome. Disadvantages of traditional external fixation are bulkiness and sharp edges causing discomfort to the patient.
Case Report: We present an interesting case of a 25-year-old male who presented to our trauma care center with a history of fall from two wheeler, sustaining injury to his left shoulder. On examination, a Type IIIB open clavicle fracture was noted. He was treated with debridement and external fixation with a locking compression plate (LCP). Vacuum-assisted closure and culture sensitive intravenous antibiotics were administered for 5 days. Post-operative follow-up was satisfactory with no signs of infection and radiological evidence of fracture healing by 3 months.
Conclusion: External fixation with LCP for clavicle fracture is a simple procedure and can be used as a definitive treatment for Type III B open clavicle fracture. Advantages include anatomical reduction, less bulk, and stable fixation. It causes less skin irritation and is comfortable to the patient ensuring good patient compliance until removal. However, the pre-operative planning and surgical technique, such as plate length, the number of locking screws, screw positioning, and locking technique, should aim to create stable fixation and avoid excessive screw penetration.
Keywords: Clavicle, Open clavicle fracture, locking compression plate external fixator, LCP, Shoulder Trauma
Fractures of the middle third of the clavicle are among the most frequent fractures in adults, with an incidence of 5–10% in young patients [1]. Open clavicle fractures are rare orthopedic injuries caused by severe direct penetrating or blunt trauma with significant multiple injuries such as chest and head trauma [2]. Open clavicle fractures or closed fractures where the skin is compressed are considered to be at high risk for necrosis and may also present a significantly increased risk for infection [3]. Preventing infection, covering soft tissues, achieving bone union, and restoring function are the objectives of open fracture care. Important principles of management include antibiotics, timing of initial surgery, thorough debridement, choice of wound closure, and fixation of fracture with acceptable alignment [4]. As external fixation offers stable fixation with little local tissue damage leading to perfect union and superior soft-tissue outcome, it is the preferred treatment for open clavicle fractures [5,6]. Only a few case reports have been previously published in the literature and, to our knowledge, no treatment recommendation or fixation devices have been established for the treatment of open and contaminated clavicle fractures. We present a case of Type IIIB open clavicle fracture which was definitively managed with a locking compression plate (LCP) as an external fixator.
A 25-year-old male patient presented to the trauma care center of Bangalore medical college and research institute after sustaining a fall from two wheeler injuring his left shoulder. On primary survey, vitals were stable and a left Type III B open midshaft clavicle fracture (Gustilo–Anderson Classification) was noted. There was a 12 × 6 cm open wound with fractured clavicle ends exposed and gross contamination with organic matter. Deltoid and pectoralis major laceration was noted at the clavicle insertion site. No neurovascular injury was found. A wound swab was taken and sent for culture and sensitivity. Thorough wound wash was given with saline, hydrogen peroxide, and betadine. Foreign bodies were removed and intravenous antibiotics were administered as per institutional protocol. On radiographic evaluation, left midshaft clavicle fracture was revealed (Allman group 1) (Fig. 1).
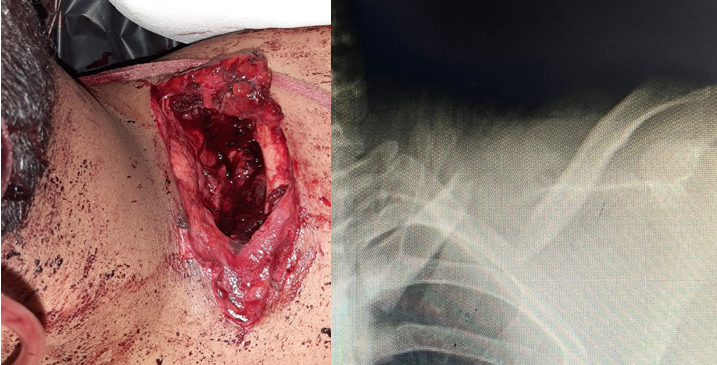
Figure 1: 12 × 6 cm open wound and midshaft clavicle fracture.
The patient was planned for emergency debridement and external fixation of clavicle fracture.
Under general anesthesia, the patient was placed in prone position with a sandbag in the interscapular space. Debridement was done as follows – foreign bodies such as gravel/stones and organic matter were removed using forceps after thorough exploration of the open wound. Necrosed muscle parts of pectoralis major and deltoid were debrided. Pulsed lavage gun was used to deliver wound wash with copious amount of saline. Hydrogen peroxide and betadine application was accompanied with wound wash (Fig. 2).

Figure 2: Wound condition after debridement.
Surgical technique for clavicle external fixation with LCP
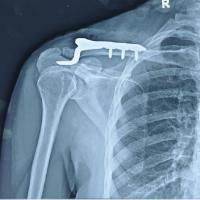
Fracture was reduced temporarily with a bone reduction clamp. Plate was planned to be fixed above the clavicle at a desirable distance of 4 cm in our case to accommodate dressing. Plate was positioned anterosuperiorly for patient’s ergonomic comfort. An 8 holed left clavicle LCP was used as an external fixator. Plate is held close to the bone initially, locking sleeve was attached and pilot hole is drilled with a 2.8 mm drill bit. Depth gauge was used to determine the length of pilot hole. Appropriate screw length can be calculated by adding 3 cm (which was the distance between the plate and skin) to the measured depth of pilot hole. For example, if 14 mm is the depth of pilot hole, adding 3 cm gives a screw length of 44 mm. Screws were inserted through the locking hole into the pre-drilled pilot hole until it engaged the far cortex. The plate was then lifted up and secured in an appropriate position before continuing to drive the screw heads into the locking holes. 3.5 mm cortical screws with bicortical purchase of determined length were inserted and locked to the plate. Inferiorly, a bone lever is used to provide counter force and protect vascular structures while drilling. Screws to be ideally placed in a near-near far-far position according to the principle of external fixation. Similarly, a total of 2 locking screws on either side of fracture are applied (Fig. 3).
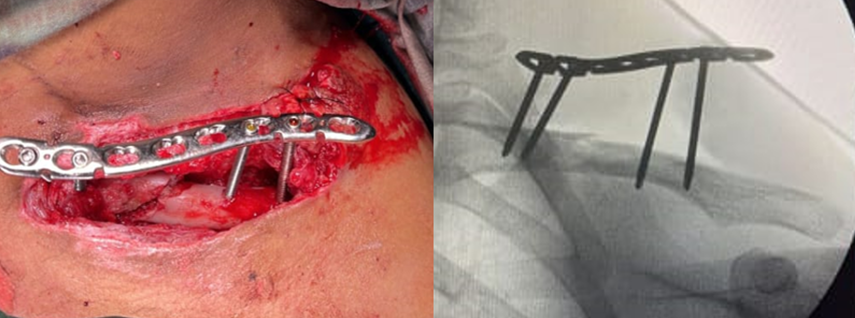
Figure 3: Intraoperative and C-arm image of clavicle locking compression plate used as ex-fix.
Stay sutures were put and vacuum-assisted closure (VAC) dressing was used for 5 days. Culture and sensitivity revealed infection with Staphylococcus aureus sensitive to piperacillin and tazobactam. Culture sensitive intravenous antibiotics and VAC were administered for 5 days by which time the exudation reduced and granulation tissue appeared healthy. VAC was removed and secondary closure was done with Ethilon. The patient was discharge on day 6 and advised shoulder immobilization with arm sling for 2 weeks after which the sutures were removed. The wound healed completely without any evidence of discharge or infection. Active range of movement exercises for shoulder was advised for the next 4 weeks. The plate was removed at 12 weeks. The patient was followed up for 6 months and no complications were noted.
Follow-up timeline
- Week 1- No discharge from the wound, stable external fixator with no signs of infection
- Week 2- Sutures from the wound removed, range of movements at shoulder initiated
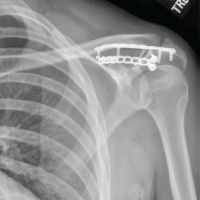
- Week 4- Physiotherapy continued and no signs of pin tract infection noted (Fig. 4)

Figure 4: Post-operative X-ray and local skin condition at 3 weeks post-operative.
- Week 6- Radiological signs of uniting clavicle fracture with satisfactory alignment noted
- Week 12- United clavicle fracture on X-ray and LCP External fixator removed,
- No discharge/pin tract infection (Fig. 5)
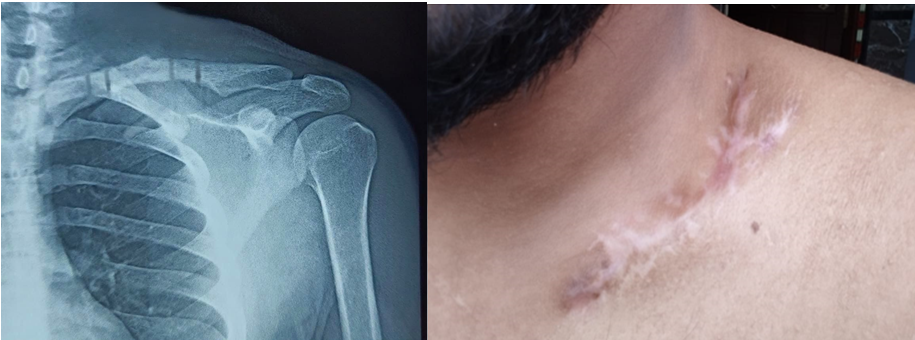
Figure 5: Post-operative X-ray at 3 months demonstrating good bony union and completely healed surgical scar post ex-fix removal .
- Week 16- Completely healed surgical site, complete range of motion at shoulder, and no signs of infection (Fig. 6).

Figure 6: Full range of movements.
Surgical fixation is recommended in open clavicle fractures, floating shoulder and fractures associated with neurovascular injuries [7]. Managing an open clavicle fracture depends on the patient’s general condition, the level of contamination, fracture severity, and degree of soft-tissue damage. Open reduction and internal fixation with internal fixation devices is not recommended due to risk of further soft-tissue damage and skin necrosis. Therefore, external fixation was advised either as a definitive fixation to stabilize the fracture with little soft-tissue injury or as temporary stabilization in damage control orthopedics, to enable multiple debridement for infection [8].External fixation does not disrupt the soft tissue envelope and permits early mobilization. Furthermore, external fixation is beneficial in comminuted fractures which is quite common in open high velocity injuries.[9]. Determining appropriate screw length is crucial in using LCP as an external fixator. According to a study by Zhang et al. on distal tibial fracture treated with LCP as an external fixator, the ideal plate to bone distance for stable fixation was determined to be <30 mm [10]. However, we could not find similar studies on clavicle fractures. We prefer to use a plate to bone distance of 3 cm which is clinically stable and provides optimum space for post-operative dressing. Traditional external fixator to clavicle causes discomfort to patient because of bulkiness, sharp edges causing local skin irritation, abrasion, and restrictions of neck movements [8]. Locking plates serve as constructs by which stability at a fracture site is achieved. The use of locking plates as a device for achieving external fixation is not a new concept. A number of authors have described the use of this method for the treatment of tibia fractures [8]. The technique has been referred to as “supercutaneous plating” [6,8]. Outlining the advantages, the locking screw head mechanism provides additional degree of stability to the construct by resisting of angular forces and reducing screw loosening. Applying a locking plate is arguably easier than a traditional external fixator. The patient is likely to tolerate the locking plate better due to its consistent shape, smooth edges, and low profile [3]. LCP is anatomically precontoured to the shape of clavicle. Strong fixation is provided by this method, which allows the clavicle to sustain load and maintain stability over time [6,8]. Our proposed management flowchart for definitive management of open clavicle fractures is mentioned in (Chart 1).
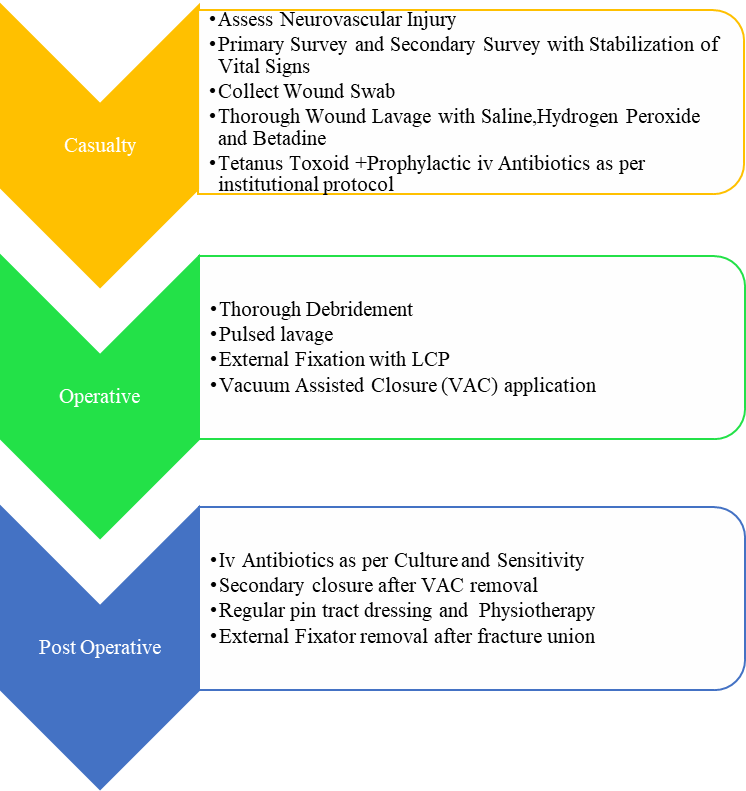
Chart 1: Proposed management flowchart for definitive management of Open clavicle fractures (BMCRI Protocol).
External fixation with LCP for clavicle fracture is a simple procedure and can be used as a definitive treatment for Type III B open clavicle fracture. Advantages include anatomical reduction, less bulk, and stable fixation. It causes less skin irritation and is comfortable to the patient ensuring good patient compliance until removal. However, the pre-operative planning and surgical technique, such as plate length, the number of locking screws, screw positioning, and locking technique, should aim to create stable fixation and avoid excessive screw penetration.
Contaminated open clavicle fractures are therapeutic challenge to an orthopedic surgeon owing to their high risk for neurovascular injuries, osteomyelitis, malunion, and non-union. Multiple surgeries are cumbersome and lead to morbidity and patient unacceptability. Open clavicle fractures can be definitively treated with external fixation using LCP, as a single effective procedure offering good functional and radiological outcome with good patient compliance.
References
- 1. Bonnevialle N, Delannis Y, Mansat P, Peter O, Chemama B, Bonnevialle P. Bilateral clavicle fracture external fixation. Orthop Traumatol Surg Res 2010;96:821-4. [Google Scholar] [PubMed]
- 2. Simon RG, Lutz B. Open clavicle fractures: A case report. Am J Orthop (Belle Mead NJ) 1999;28:301-3. [Google Scholar] [PubMed]
- 3. Kenyon RM, Morrissey DI, Molony DC, Quinlan JF. Locking plate external fixation and negative pressure wound therapy for treatment of a primary infection in a closed clavicle fracture. BMJ Case Rep 2016;2016:bcr2016218241. [Google Scholar] [PubMed]
- 4. Schuind F, Pay-Pay E, Andrianne Y, Donkerwolcke M, Rasquin C, Burny F. External fixation of the clavicle for fracture or non-union in adults. J Bone Joint Surg Am 1988;70:692-5. [Google Scholar] [PubMed]
- 5. Strauss EJ, Kaplan KM, Paksima N, Bosco JA 3rd. Treatment of an open infected type IIB distal clavicle fracture: Case report and review of the literature. Bull NYU Hosp Jt Dis 2008;66:129-33. [Google Scholar] [PubMed]
- 6. Sirisreetreerux N, Sa-Ngasoongsong P, Chanplakorn P, Kulachote N, Laohajaroensombat S, Suphachatwong C, et al. Using a reconstruction locking compression plate as external fixator in infected open clavicle fracture. Orthop Rev (Pavia) 2013;5(2):e11. [Google Scholar] [PubMed]
- 7. Kotekar MF, Pai S, Yogesh K, Kumar MA, Shetty MS. Anatomy of clavicle in the Indian population and its applicability in pre-contoured plating. Int Orthop 2020;44:699-704. [Google Scholar] [PubMed]
- 8. Kloen P. Supercutaneous plating: Use of a locking compression plate as an external fixator. J Orthop Trauma 2009;23:72-5. [Google Scholar] [PubMed]
- 9. Vekris MD, Papadopoulos DV, Elisavet M, Papageorgiou CD, Korompilias AV. External Fixation of Clavicle Fractures with Comminution or in Highly Active Patients. J Long Term Eff Med Implants. 2025;35(1):61-66. doi:10.1615/JLongTermEffMedImplants.2024049825 [Google Scholar] [PubMed] [CrossRef]
- 10. Zhang J, Ebraheim N, Li M, He X, Schwind J, Liu J, et al. External fixation using locking plate in distal tibial fracture: A finite element analysis. Eur J Orthop Surg Traumatol 2015;25:1099-104. [Google Scholar] [PubMed]