Fixed flexion deformity of the knee is a complex pathology with various etiologies. Proper pre-operative assessment and planning help in yielding good functional outcomes. Fixed-angle blade plates can be a very useful implant in deformity correction.
Dr. Adithyaa Sivaramakrishnan, Department of Orthopedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai - 600116, Tamil Nadu, India. E-mail: adhityaa.srk@gmail.com
Introduction: Fixed flexion deformities of the knee joint can be due to a variety of causes – intra-articular, extra-articular, muscular, neurogenic, etc. The etiology decides the mode of management and prognosis.
Case Report: A 16-year-old male with a 2-year-old malunited right distal femur physeal injury presented with “fixed flexion deformity” of the knee. Clinical and radiological assessment showed that the “fixed flexion knee deformity” was actually a procurvatum deformity of the distal femur. Supracondylar extension osteotomy was done after thorough planning and using an angle blade plate as an alignment tool.
Conclusion: Following the procedure, the patient had complete correction of the deformity. His quality of life indicators were in support of a good to excellent functional outcome.
Keywords: Fixed flexion deformity , Extension osteotomy, distal femur malunion, Supracondylar osteotomy
Fixed flexion deformities of the knee joints are common and can be caused by various etiologies. This particular deformity occurs in the sagittal plane and causes severe morbidity and cosmetic disapproval to the patient. Flexion contractures [1] can be caused by intra-articular pathologies, soft-tissue contractures due to scars, burns, prolonged immobilization in non-anatomical positions, inflammatory arthritis such as rheumatoid arthritis, neurological disorders such as poliomyelitis, cerebral palsy, etc. In neurological disorders, weakness of the quadriceps with normal or overacting hamstrings can lead to fixed flexion knee deformity. Knee flexion contractures may cause abnormalities of gait. Since full knee extension is required during the heel strike of the stance phase, in the presence of fixed flexion deformity (FFD), the patient tends to bend excessively forward (at the hips or spine) to bring his center of gravity forward to complete the gait cycle. The characteristic gait associated with flexion contractures in cerebral palsy patients is the crouch gait, where there is excessive knee flexion in the stance phase. The loss of ankle plantar flexion and/or knee extension keeps the ground reaction force behind the knee joint and in front of the hip and ankle joints [2]. In electromyography, usually overactivity of the hamstrings is found. Contractures of the iliopsoas or gastrocnemius also have the potential to flex the hips and knees, respectively. In the setting of knee flexion deformity post-trauma, clinical and radiological assessment of the deformity is very important. A distal femur or proximal tibia procurvatum (anterior angulation or posterior tilt) may clinically mimic a knee flexion deformity. Hence, the sagittal plane deformity assessment principles as described by Dror Paley have to be meticulously followed to find out the origin and location of the extra-articular deformity. Long-term sagittal plane deformities, such as procurvatum, can cause abnormal loading of the posterior tibial condyles and cause early osteoarthritis. Early osteoarthritis makes planning for total knee arthroplasty in the future a tedious process and extensive planning [1]. Hence, it is better to correct clinically significant sagittal plane deformities.
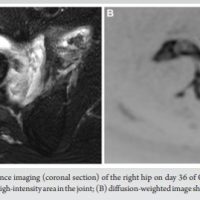
A 16-year-old male presented with complaints of deformity over his right knee for the past 2 years, associated with altered gait for the same period. He gives a history of a road traffic accident 2 years back, when he sustained a closed injury to his right knee. He was treated with indigenous splinting for 45 days, after which he was allowed to weight-bear and walk. On starting to weight bear, he noticed the deformity over his right knee. He was unable to extend his right knee fully, and his gait had changed following the injury. He was initially treated elsewhere with physiotherapy, but had no improvement in deformity, even though pain subsided. Even though he was managing functionally well with the deformity, he found it cosmetically displeasing to walk with the deformity. On examination, he had a short limb gait, a FFD of his right knee of around 30°, and multiple healed scars over his right knee were present. Bony thickening and broadening were felt over the distal femur. The range of right knee flexion was from 30° to 120°. A 3 cm femoral segment shortening was present on the right side. Distal neurovascular status was intact. Radiograph of right knee anteroposterior (AP) and lateral views (Fig. 1) were taken and showed a malunited fracture of the distal femur with open physis of the proximal tibia and fibula.
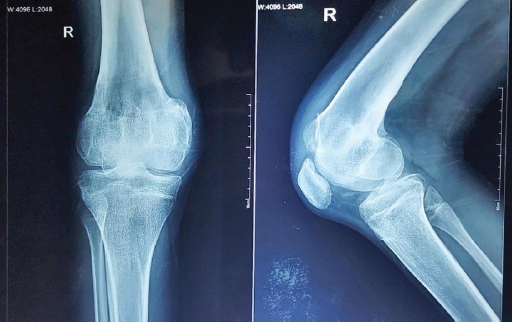
Figure 1 Presenting right knee radiograph
The distal femur physis was not clearly visible, suggesting that the injury was a distal femur physeal injury. Full-length radiographs of both lower limbs (Figs. 2) spanning from the hips to the ankles were taken to assess the mechanical axis of both lower limbs and to identify the pathology.
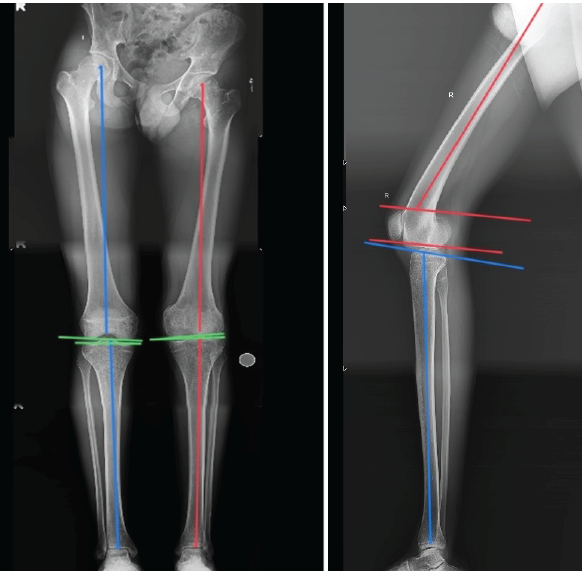
Figure 2 Skannogram of right lower limb
On assessing the radiographs, using Paley’s malalignment tests, no coronal plane deformities were seen as the mechanical medial proximal tibial angle, the mechanical lateral distal femoral angle, and joint line convergence angle were within the normal limits.
On the lateral view, the mechanical posterior distal femoral angle (mPDFA) was below the normal range of 79°, and hence our patient was diagnosed with procurvatum deformity of the right distal femur with premature closure of physis, probably due to right distal femur physeal injury, malunion, which eventually turned out to be the etiology of his FFD of the right knee. He was then planned for right distal femur supracondylar extension osteotomy (Fig. 3), where lines A, D, and E are parallel and lines B and X are perpendicular to each other. Even under the effect of anesthesia, the FFD did not reduce (Fig. 4).
Figure 3: Pre-op planning of extension osteotomy

Figure 4: Under anaesthesia right knee showing FFD of 30°
Under general anesthesia, under pneumatic tourniquet control, the distal femur was exposed through a lateral approach. A 90° fixed-angle AO blade plate was chosen for fixing the osteotomized femur. A pin was inserted just proximal to the physeal scar at the planned osteotomy site so that the blade of the blade plate and one screw could be used distal to the osteotomy site for fixation. The path for the blade portion of the blade plate was prepared distal to the planned osteotomy site before starting the osteotomy, such that the blade of the blade plate lies parallel to the proximal tibial plateau (Fig. 5) and forms an angle with the femoral shaft proximally, which indicates the amount of correction needed.
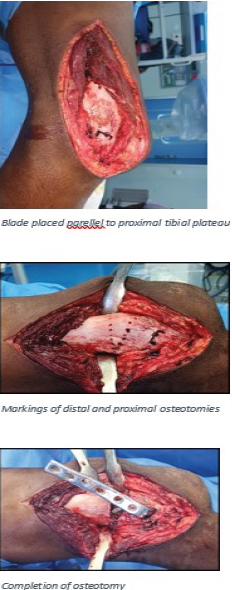
Figure 5: Osteotomy of distal femur
The distal osteotomy is performed first by marking the osteotomy site 15 mm proximal to the blade such that it is also in parallel with the proximal tibial plateau (Fig. 5). The proximal osteotomy is marked in such a way that the osteotomy is perpendicular to the proximal femoral shaft (Fig. 5). Both the osteotomies are performed with the tip of the wedge ending posteriorly (Fig. 5). The bone is then removed and the distal portion is extended and fixed to the proximal portion with the blade plate and appropriate screws – blade and one cancellous screw distally and four 4.5 mm cortical screws proximally (Fig. 6).

Figure 6: Correction of Fixed flexion deformity
Post-operative radiograph (Fig. 7) was taken and showed good correction of mPDFA. He was started on non-weight-bearing mobilization with a long knee extension brace and walker support from post-operative day 1. Active knee mobilization exercises were also started, and his wound healed uneventfully.
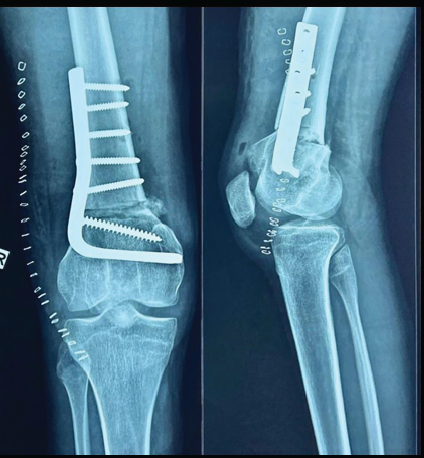
Figure 7: Post operative radiograph
He was routinely reviewed and was started on full weight-bearing mobilization at 2 months post-operative. He was reviewed recently at 2 years post-operative period and showed excellent functional outcome with full pain free active range of movements of right knee from 0° to 150° (Fig. 8). He was able to do straight leg raise (Fig. 8) independently and had full extension- 0° (Fig. 8). No limb length discrepancies were noted (Fig. 8) and bilateral stance from anterior (Fig. 8) and posterior aspects (Fig. 8) were also normal. Post-operative radiograph showing the knee with distal femur AP (Fig. 9) and lateral views (Fig. 9) showed union of the osteotomy with no signs of implant failure or loosening and good correction of the mPDFA.

Figure 8: Post operative follow up clinical images
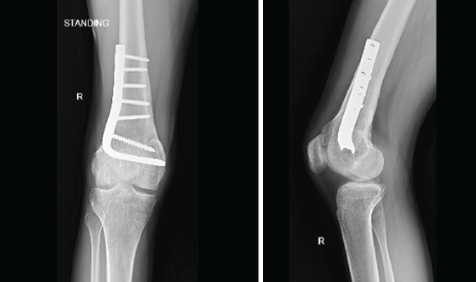
Figure 9: Post operative follow up radiography
Cerebral palsy and the resulting spastic diplegia causing crouch gait is one of the most common clinical scenarios where distal femur extension osteotomies are performed as a part of single-event multilevel surgeries [3]. Most of the supracondylar distal femur extension osteotomies are done for fixed flexion deformities in cerebral palsy patients with crouch gait [4,5]. It was also associated with hamstrings shortening and quadriceps lengthening [6], which had to be addressed by patellar tendon advancement [7,8]. This procedure addresses an FFD in a young active male due to malunion of the distal femur physeal injury. The technical tip is that the blade of the 90° angle blade plate was inserted parallel to the knee joint line/articular surface of the proximal tibia. The angle that the plate forms with the shaft of the femur is the degree of correction required to attain full extension. Rotating the plate after fixation of the blade and removing the osteotomy wedge, and fixing the plate to the proximal segment of the femur will automatically correct the deformity to the desired level of correction.
The previous supporting literature regarding the distal femur osteotomy for correcting FFD due to malunion has been addressed using a Dome’s osteotomy [9] as reported in the Egyptian Journal of Orthopaedics. Since in our patient, the deformity using Paley’s principles of deformity correction discerns the deformity mainly in the Sagittal plane with acceptable normal angles in the coronal plane, this negates the necessity of doing a multiplanar or Dome osteotomy.
The other treatment protocol, as evidenced in the article by Fragomen et al. [10], was used in three patients who developed knee FFD post-trauma in their childhood with physeal injuries to the distal femur and also had a lesser posterior distal femoral angle, thus leading to procurvatum deformity of the distal femur. Here, a distal femoral osteotomy and fixation with angle-stable lateral distal femoral locking plates, along with a proximal femoral osteotomy and intramedullary fixation with an intramedullary lengthening nail, were done to negate the limb shortening post the distal femoral osteotomy and to correct the limb shortening post-physeal injury.
Our patient was initially on non-weight-bearing mobilization post the surgery, reviewed on a regular outpatient department basis, and was started on weight bearing following consolidation of the osteotomy site. Physical therapy in the form of isometric quadriceps and hamstrings strengthening exercises, and knee range of movements exercises was started.
The quality of life indicators post the surgery indicated good to excellent functional outcomes for the patient, with a full pain-free range of movements and full extension. He is able to walk independently unaided, able to carry out his Activities of daily living unsupported, and happy with the outcomes post the surgery.
Post-traumatic distal femur procurvatum deformity can present as “fixed flexion deformity” of the knee joint. The angle blade plate still remains a useful implant to intra-operatively template the deformity correction and provide a stable fixation for early mobilization and good functional outcome.
Here in this case report, with proper pre-operative planning, we decided to perform distal femur supracondylar extension osteotomy with a 90° fixed-angle blade plate, which resulted in good correction of deformity and excellent functional outcomes. Hence, angle blade plates can be a useful tool for deformity correction.
References
- 1. Shetty K, Mittal P, Darshan MS. Intra-articular osteotomy for correction of neglected malunion of medial femoral condyle Hoffa’s fracture. J Orthop Rep 2023;2:100158. [Google Scholar] [PubMed]
- 2. Lenhart RL, Smith CR, Schwartz MH, Novacheck TF, Thelen DG. The effect of distal femoral extension osteotomy on muscle lengths after surgery. J Child Orthop 2017;11:472-8. [Google Scholar] [PubMed]
- 3. Thomason P, Selber P, Graham HK. Single event multilevel surgery in children with bilateral spastic cerebral palsy: A 5 year prospective cohort study. Gait Posture 2013;37:23-8. [Google Scholar] [PubMed]
- 4. Das SP, Pradhan S, Ganesh S, Sahu PK, Mohanty RN, Das SK. Supracondylar femoral extension osteotomy and patellar tendon advancement in the management of persistent crouch gait in cerebral palsy. Indian J Orthop 2012;46:221-8. [Google Scholar] [PubMed]
- 5. Stout JL, Gage JR, Schwartz MH, Novacheck TF. Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy. J Bone Joint Surg Am 2008;90:2470-84. [Google Scholar] [PubMed]
- 6. Wallace SJ, Greenstein MD, Fragomen AT, Reif TJ, Rozbruch SR. Staged extra-articular deformity correction in the setting of total knee arthroplasty. Arthroplast Today 2023;24:101247. [Google Scholar] [PubMed]
- 7. Aroojis A, Patel M, Shah A, Sarathy K, Vaidya S, Mehta R. Distal femoral extension osteotomy with 90° pediatric condylar locking compression plate and patellar tendon advancement for the correction of crouch gait in cerebral palsy. Indian J Orthop 2019;53:45-52. [Google Scholar] [PubMed]
- 8. Nabian MH, Zadegan SA, Mallet C, Neder Y, Ilharreborde B, Simon AL, et al. Distal femoral osteotomy and patellar tendon advancement for the treatment of crouch gait in patients with bilateral spastic cerebral palsy. Gait Posture 2024;110:53-8. [Google Scholar] [PubMed]
- 9. El Ghafar K, Diab RA. Supracondylar femoral dome extension osteotomy in treatment of knee flexion deformity. Egypt Orthop J 2021;56:48-55. [Google Scholar] [PubMed]
- 10. Fragomen AT, Fragomen FR. Distal femoral flexion deformity from growth disturbance treated with a two-level osteotomy and internal lengthening nail. Strategies Trauma Limb Reconstr 2017;12:159-67. [Google Scholar] [PubMed]