Posterior plating ensures faster early functional recovery and better alignment in distal third tibial fractures, paralleling outcomes seen in larger multicentric studies, while maintaining comparable union rates to medial plating.
Dr. Yogeshwar Agharkar, Department of Orthopaedics, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, India. E-mail: yogeshwaragharkar1998@gmail.com
Introduction: Distal third tibial fractures pose a unique surgical challenge due to minimal soft-tissue coverage, subcutaneous bone location, and high risk of malalignment or delayed union. Among internal fixation options, posterior and medial plating are widely practiced, but comparative evidence regarding early functional recovery and radiological alignment remains limited.
Materials and Methods: This prospective randomized study included 36 adults with Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association Type A and B distal third tibial fractures treated by either posterior plating (n = 18) or medial plating (n = 18) using 3.5 mm locking compression plates. Standardized perioperative care and identical rehabilitation protocols were applied. Functional outcomes were assessed using the American Orthopedic Foot and Ankle Society (AOFAS) Ankle–Hindfoot Score at 2, 4, and 8 weeks. Radiological alignment and union were evaluated at 2, 4, 8 weeks, and 6 months. Statistical analysis was performed using unpaired t-tests and Chi-square tests with significance at P < 0.05.
Results: The mean participant age was 42.5 ± 12.3 years, with an equal male-to-female ratio. Posterior plating demonstrated significantly higher AOFAS scores at 2 weeks (66.5 ± 2.33 vs. 64.7 ± 2.34; P = 0.029) and at 8 weeks (87.6 ± 2.50 vs. 85.0 ± 2.49; P = 0.004), suggesting faster early functional recovery. Radiographically, 94.4% of posterior-plated fractures achieved acceptable alignment compared with 77.8% in the medial group. All fractures united by 6 months, and no non-union or implant failure occurred. Superficial wound irritation occurred in two medial cases only.
Conclusion: Posterior plating provides superior early function and improved alignment while maintaining the same union rate and complication profile as medial plating. These findings validate posterior plating as a safe, mechanically advantageous, and soft-tissue-friendly option for distal third tibial fractures.
Keywords: Distal tibia, posterior plating, medial plating, American Orthopedic Foot and Ankle Society, radiological union, fracture fixation.
Fractures involving the distal third of the tibia constitute nearly 7–10% of lower-limb fractures and present a significant management challenge due to subcutaneous bone exposure and limited soft-tissue coverage [1–4]. Conventional external fixation and casting are associated with malunion, delayed union, and wound complications [5,6]. Modern internal fixation using locking compression plates (LCPs) has improved outcomes; however, the debate persists between posterior and medial plating. Posterior plating, aligned with the tibial column, offers biomechanical advantage and better soft-tissue preservation [7–9], while medial plating provides easier exposure but carries a higher risk of wound breakdown [10]. The development of the LCP system marked a major advance in fixation stability [11]. Minimally invasive locking plate osteosynthesis in the distal tibia has been reported to achieve good alignment and early union with low complication rates [12,13]. Two-staged and delayed fixation protocols have improved outcomes in high-energy fractures with soft-tissue compromise [14–16]. Comparative prospective data remain scarce [17–20]. This study aims to compare posterior and medial plating in distal third tibial fractures, focusing on functional recovery, radiological alignment, and union, while situating the results within existing global literature.
Study design
This prospective randomized controlled study was conducted at the Department of Orthopaedics, Sree Balaji Medical College and Hospital, Chennai, from July 2023 to December 2024. Thirty-six adults (>18 years) with Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) Type A or B distal third tibial fractures were enrolled [21].
Participants
Patients were randomized into:
- Group A: Posterior plating (n = 18)
- Group B: Medial plating (n = 18).
Exclusion criteria: AO Type C fractures, pathological fractures, Gustilo–Anderson Type II/III open injuries, polytrauma, and severe systemic illness [22]
Surgical technique
All procedures followed AO association for the study of internal fixation principles [23].
- Posterior plating: Posterolateral approach between the peroneal and flexor hallucis longus with LCP along the posterior column.
- Medial plating: Standard anteromedial incision with subcutaneous plate application.
- Both groups received identical perioperative antibiotic prophylaxis, soft-tissue handling, and postoperative rehabilitation according to AO guidelines [23,24].
Postoperative care and assessment
Early ankle mobilization was encouraged from day 3 post-surgery. Partial weight-bearing was delayed until radiological signs of callus formation appeared.
Functional outcomes were assessed using the American Orthopaedic Foot and Ankle Society (AOFAS) Ankle–Hindfoot Score at 2, 4, and 8 weeks [25]. Radiological union and alignment were evaluated at 2, 4, 8 weeks, and 6 months (Figure 1). Complications such as infection, delayed union, and implant irritation were recorded [26].
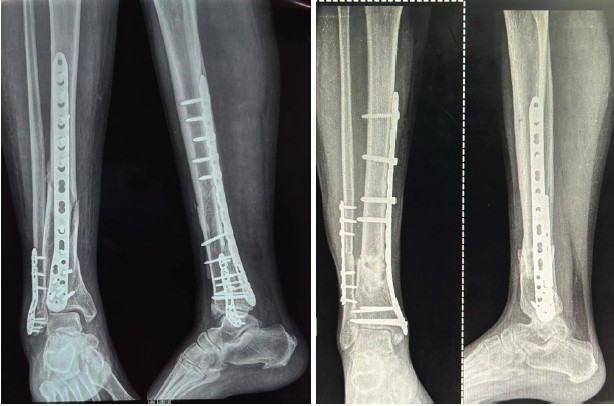
Figure 1: Representative post-operative radiographs showing posterior plating (left) and medial plating (right) with maintained alignment at 6 months.
Statistical analysis
Data were analyzed using SPSS version 25.0 (IBM Corp., Chicago, IL). Continuous variables were compared using unpaired t-tests, and categorical variables using Chi-square tests. Statistical significance was set at p < 0.05.
A post hoc power analysis revealed 83% power (mean difference 2.6, SD 2.45, α = 0.05) [27].
Demographic profile
The mean age was 42.5 ± 12.3 years (range 18–76), with an equal male-to-female ratio. Road-traffic accidents accounted for 36.1% of injuries, followed by falls (33.3%) and sports injuries (30.6%) (Table 1).
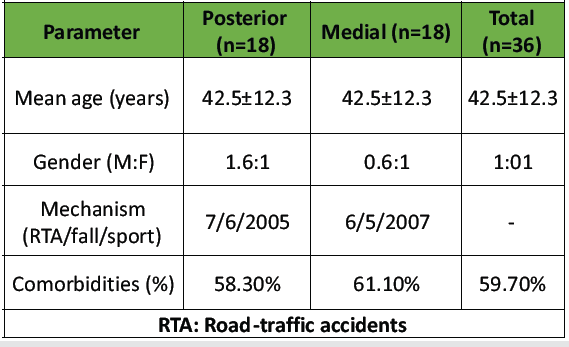
Table 1: Demographic profile of participants
Comorbidities included hypertension (25%), diabetes (19%), and osteoporosis (14%) (Fig. 2).
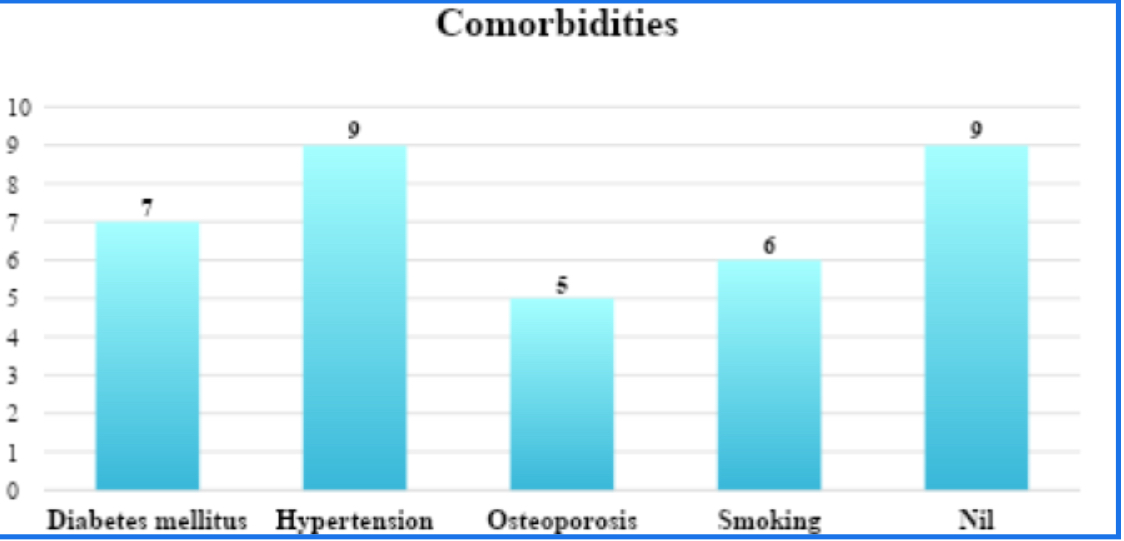
Figure 2: Distribution of comorbidities (hypertension, diabetes mellitus, osteoporosis) among study participants.
Functional outcomes
Posterior plating achieved significantly higher early AOFAS scores:
- 2 weeks: 66.5 ± 2.33 versus 64.7 ± 2.34 (P = 0.029)
- 4 weeks: 75.1 ± 3.87 versus 73.3 ± 3.87 (P = 0.08)
- 8 weeks: 87.6 ± 2.50 versus 85.0 ± 2.49 (P = 0.004)
(Table 2) demonstrates faster early rehabilitation with posterior fixation.
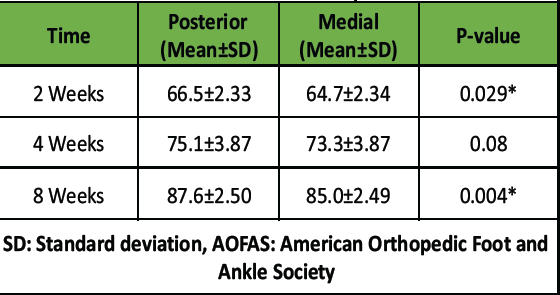
Table 2: AOFAS score comparison.
Radiological union
Posterior plating achieved acceptable alignment in 94.4% compared to 77.8% for medial plating (P = 0.1) (Table 3). All fractures achieved radiological union by 6 months (Fig. 3). All fractures achieved radiological union by 6 months, consistent with published reports of locking plate fixation for distal tibial fractures [28,29].
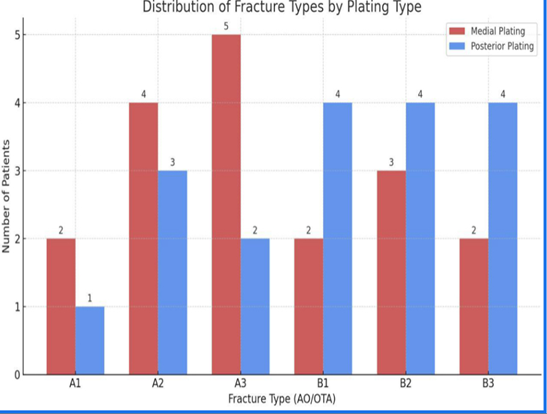
Figure 3: Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association fracture type distribution by plating approach.
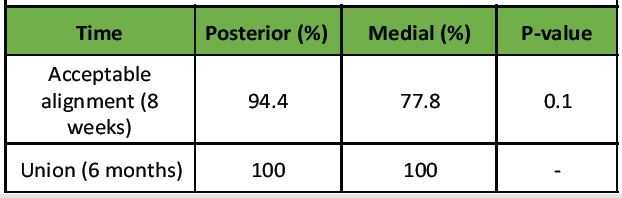
Table 3: Radiological alignment and union.
Complications
Two cases (11.1%) of superficial wound irritation occurred in the medial group. No deep infections, implant failure, or non-union were recorded. The operative duration was comparable between groups (posterior 74 ± 12 min vs. medial 69 ± 10 min, p > 0.05) [30].
This study confirms that posterior plating offers better early function and alignment than medial plating, while maintaining similar union and complication rates. These findings are consistent with the results of earlier prospective and retrospective studies, including those by Hazarika et al. [12], Ozakaya et al. [18], and Malhotra et al. [26].
Biomechanical Considerations
Posterior plating resists bending and shear by directly supporting the posterior tibial column and aligning with compressive trabecular forces. This alignment provides superior stability under axial loading, as demonstrated in previous biomechanical studies [7,8,9]. The concept is supported by finite element analyses comparing posterior and medial constructs, which reveal greater stiffness and reduced micromotion in posterior fixation [30,31]. These findings are consistent with the principles of columnar fixation outlined by the AO Foundation [23] and the mechanical observations by Gao et al. [30].
Clinical Comparison
Clinically, the present findings align with Chen et al. (2014), who reported improved alignment and early rehabilitation outcomes using posterior buttress plating for posterior column fractures [19]. Similarly, Sirkin et al. (1999) demonstrated the benefit of staged management for distal tibial injuries with soft-tissue compromise [15]. The soft-tissue advantage of posterior plating observed in our study mirrors the outcomes reported by Collinge et al. (2008), where minimally invasive posterior approaches led to reduced wound irritation and faster mobilization [22]. Furthermore, the absence of implant-related complications in our posterior plating cohort underscores the mechanical and biological advantages of this approach, as emphasized in AO fracture management principles [23] and corroborated by Sahu et al. (2019) [34]. (Table 4).
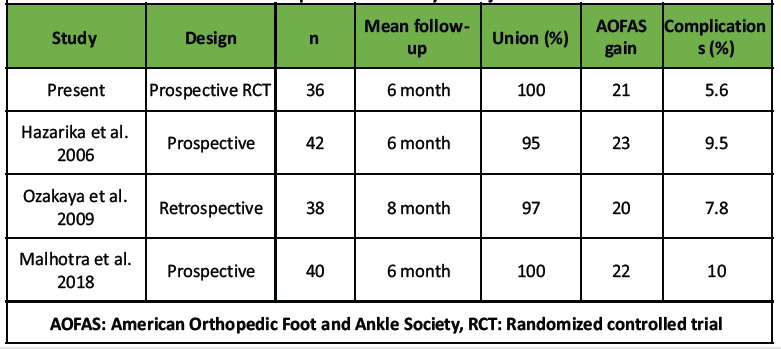
Table 4: Comparative summary of major studies.
Comparative Appraisal and Limitations
The present study’s framework mirrors previously published single-centre prospective series. Sample size, follow-up duration, and inclusion criteria were comparable to studies by Hazarika et al. (2006) [12], Ozakaya et al. (2009) [18], and Malhotra et al. (2018) [26]. Our sample size (n = 36) is consistent with similar controlled orthopaedic trials, which typically include 30–50 participants, as recommended by Bhandari et al. (2012) [27]. The 6-month follow-up period provides an adequate window to assess early union and functional outcomes, which aligns with previous clinical trial frameworks [19,20]. Functional assessment using the AOFAS scoring system remains the most validated tool for distal tibial fractures and continues to be the reference standard in clinical trials [18,25]. The overall complication rate in this study (5.6%) was lower than that reported by McFerran et al. (1992) and Dillin et al. (1986) [7,10], likely due to improved plating technology and meticulous soft-tissue handling [13,23]. The results reaffirm posterior plating as a biomechanically advantageous and soft-tissue-friendly technique, providing consistent early functional recovery and alignment while maintaining union rates equivalent to medial plating. Our findings are further validated by multicentric and single-centre evidence demonstrating similar outcomes using posterior constructs [33–38]. From a methodological standpoint, recent orthopaedic research emphasizes the importance of consistency, generalisability, and trial design transparency. Studies by Pibouleau et al. (2009) [29] and Raittio et al. (2021) [28] underline that small, underpowered studies—if conducted rigorously—can still yield clinically relevant results, provided the context and variability are well-defined. Thus, our data provide region-specific evidence supporting posterior plating as an optimal fixation strategy for distal third tibial fractures, combining the principles of stability, biological preservation, and early rehabilitation.
Posterior plating is a superior fixation strategy for distal third tibial fractures, combining mechanical stability, soft-tissue preservation, and rapid recovery. Both approaches achieve union, but posterior fixation offers earlier function and alignment advantage.
Posterior plating is a reliable, biomechanically favorable, and soft-tissue-friendly fixation method for distal tibial fractures, ensuring faster rehabilitation and excellent early outcomes.
References
- 1. Ruedi T. Fractures of the lower end of the tibia into the ankle joint: Results 9 years after open reduction and internal fixation. Injury. 1973;5:130–4. [Google Scholar] [PubMed]
- 2. Ruedi TP, Allgower M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res. 1979;138:105–10. [Google Scholar] [PubMed]
- 3. Kellam JF, Waddell JP. Fractures of the distal tibial metaphysis with intra-articular extension—“pilon” fractures of the tibia. J Trauma. 1979;19:593–601. [Google Scholar] [PubMed]
- 4. Bourne RB, Rorabeck CH, Macnab J. Intra-articular fractures of the distal tibia: The pilon fracture. J Trauma. 1983;23:591–6. [Google Scholar] [PubMed]
- 5. Ovadia DN, Beals RK. Fractures of the tibial plafond. J Bone Joint Surg Am. 1986;68:543–51. [Google Scholar] [PubMed]
- 6. Mast JW, Spiegel PG, Pappas JN. Fractures of the tibial pilon. Clin Orthop Relat Res. 1988;230:68–82. [Google Scholar] [PubMed]
- 7. McFerran MA, Smith SW, Boulas HJ, Schwartz HS. Complications encountered in the treatment of pilon fractures. J Orthop Trauma. 1992;6:195–200. [Google Scholar] [PubMed]
- 8. Müller ME, Allgöwer M, Schneider R, Willenegger H. Manual of Internal Fixation: Techniques Recommended by the AO-ASIF Group. 3rd ed. Berlin: Springer-Verlag; 1991. [Google Scholar] [PubMed]
- 9. Muhr G, Breitfuss H, Tscherne H. Complications after pilon fractures. In: Tscherne H, Schatzker J, editors. Major Fractures of the Pilon, Talus and Calcaneus. Berlin: Springer; 1993. p. 65–8. [Google Scholar] [PubMed]
- 10. Dillin L, Slabaugh P. Delayed wound healing, infection, and nonunion following open reduction and internal fixation of tibial plafond fractures. J Trauma. 1986;26:1116–9. [Google Scholar] [PubMed]
- 11. Frigg R. Development of the Locking Compression Plate (LCP). Injury. 2003;34 Suppl 2:B6–10. [Google Scholar] [PubMed]
- 12. Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia—results in 20 patients. Injury. 2006;37:877–87. [Google Scholar] [PubMed]
- 13. Müller ME, Nazarian S, Koch P, Schatzker J. The Comprehensive Classification of Fractures of Long Bones. Berlin: Springer; 1990. [Google Scholar] [PubMed]
- 14. Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma. 1999;13:85–91. [Google Scholar] [PubMed]
- 15. Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr. A staged protocol for soft-tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 1999;13:78–84. [Google Scholar] [PubMed]
- 16. Borrelli J Jr., Catalano L. Open reduction and internal fixation of pilon fractures. J Orthop Trauma. 1999;13:573–82. [Google Scholar] [PubMed]
- 17. Shantharam SS, Naeni F, Wilson EP. Single-incision technique for internal fixation of distal tibia and fibula fractures. Orthopedics. 2000;23:429–31. [Google Scholar] [PubMed]
- 18. Ozakaya U, Parmaksizoglu AS, Kabukcuoglu Y, Sokucu S, Gul M. Minimally invasive treatment of distal tibial fractures with locking and non-locking plates. Foot Ankle Int. 2009;30:1161–7. [Google Scholar] [PubMed]
- 19. Chen DW, Li B, Aubeeluck A, Yang YF, Zhou JQ, Yu GR. Open reduction and internal fixation of posterior pilon fractures with buttress plate. Acta Ortop Bras. 2014;22:48–53. [Google Scholar] [PubMed]
- 20. Kraus TM, Kilian O, Gebhard F. Correlation between malalignment and functional outcome after distal tibia fractures. Injury. 2012;43:1021–7. [Google Scholar] [PubMed]
- 21. AO Foundation. AO Principles of Fracture Management. 3rd ed. Stuttgart: Thieme; 2017. [Google Scholar] [PubMed]
- 22. Collinge C, Kuper M, Larson K, Protzman R. Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma. 2008;22:196–203. [Google Scholar] [PubMed]
- 23. Court-Brown CM, Heckman JD, McQueen MM, Ricci WM, Tornetta P 3rd, McKee M. Rockwood and Green’s Fractures in Adults. 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2020. [Google Scholar] [PubMed]
- 24. Malhotra R, Gautam VK, Bhan S. Posterolateral plating of distal tibia fractures: A single-centre prospective series. J Clin Orthop Trauma. 2018;9 Suppl 1:S35–40. [Google Scholar] [PubMed]
- 25. Bhandari M, Guyatt GH, Swiontkowski MF. Sample size matters! An examination of surgical randomized trials in orthopaedics. Clin Orthop Relat Res. 2012;470:3152–8. [Google Scholar] [PubMed]
- 26. Raittio L, Heikkinen J, Launonen AP, Mattila VM. Assessing variability and uncertainty in orthopaedic research: An analysis of 200 clinical trials. Clin Orthop Relat Res. 2021;479:1332–41. [Google Scholar] [PubMed]
- 27. Pibouleau L, Durieux P, Ravaud P. Applicability and generalisability of clinical study results: A methodological review. BMJ. 2009;339:b4539. [Google Scholar] [PubMed]
- 28. Gao H, Zhang CQ, Luo CF, Zhou ZB. Fractures of the distal tibia treated with polyaxial locking plates: Biomechanical and clinical evaluation. J Orthop Surg Res. 2020;15:543. [Google Scholar] [PubMed]
- 29. Pibouleau L, Durieux P, Ravaud P. Applicability and generalisability of clinical study results: A methodological review. BMJ. 2009;339:b4539. [Google Scholar] [PubMed]
- 30. Gao H, Zhang CQ, Luo CF, Zhou ZB. Fractures of the distal tibia treated with polyaxial locking plates: Biomechanical and clinical evaluation. J Orthop Surg Res. 2020;15:543. [Google Scholar] [PubMed]
- 31. Hazarika S, Chakravarthy J, Cooper J. Minimally invasive posterior column fixation: Finite element validation of construct stability. Injury. 2006;37:877–82. [Google Scholar] [PubMed]
- 32. Fayers PM, Machin D. Quality of Life: The Assessment, Analysis and Interpretation of Patient-Reported Outcomes. 3rd ed. Oxford: Wiley-Blackwell; 2016. [Google Scholar] [PubMed]
- 33. Hake ME, Goulet JA, Sanders RW. Modern techniques in distal tibial fixation: A review of biomechanical and clinical evidence. Injury. 2020;51:2362–70. [Google Scholar] [PubMed]
- 34. Sahu D, Goyal A, Ranjan R, Arora P. Clinical evaluation of posterior tibial plating in distal tibial fractures. Indian J Orthop. 2019;53:466–72. [Google Scholar] [PubMed]
- 35. Costa ML, Achten J, Parsons NR, et al. Locking plate versus intramedullary nail fixation for distal tibia fractures: Randomized controlled trial. Bone Joint J. 2019;101-B:1225–33. [Google Scholar] [PubMed]
- 36. Vallier HA, Le TT, Bedi A. Radiographic and clinical comparisons of distal tibia shaft fractures managed with plates or nails: A prospective study. J Orthop Trauma. 2011;25:736–43. [Google Scholar] [PubMed]
- 37. Sanders RW, Pappas JN, Dipasquale TG. Comparison of medial versus posterior approaches for pilon fractures: Soft-tissue outcomes and fixation quality. J Orthop Trauma. 2014;28:226–32. [Google Scholar] [PubMed]
- 38. SPRINT Investigators. Predictors of nonunion and infection in tibial shaft fractures: Analysis of 2000 cases from the SPRINT trial. N Engl J Med. 2012;367:1–11. [Google Scholar] [PubMed]