Achieving optimal TAD, positive cortical reduction, and intact lateral wall intraoperatively significantly improves outcomes and reduces mechanical failures in PFN-treated unstable intertrochanteric fractures.
Dr. Nishant Kumar Niraj, Department of Joint Replacement and Orthopaedics, Tata Main Hospital, Jamshedpur, Jharkhand, India. E-mail: doc.nkniraj@gmail.com
Introduction: The global elderly population is steadily increasing, and among the fractures commonly observed in this age group, trochanteric hip fractures are particularly prevalent. Over time, various implant designs have been developed to manage these fractures, with the proximal femoral nail (PFN) emerging as the preferred choice for treating unstable trochanteric fractures due to its biomechanical advantages. However, despite its benefits, the application of PFN is not without challenges. Complications such as screw cut-out, Z-effect, reverse Z-effect, and suboptimal functional outcomes have been reported in some cases. This study aims to evaluate the individual and combined effects of key factors – tip-apex distance (TAD), lateral wall integrity, and the type of cortical reduction observed in immediate post-operative images – on the final radiological outcomes in elderly patients with unstable intertrochanteric fractures managed using PFN.
Materials and Methods: This retrospective observational study was conducted in our institution from June 2021 to December 2023. After fulfilling the inclusion and exclusion criteria, we had 100 patients (35 males and 65 females) with a mean age of approximately 71 years, all of whom had unstable intertrochanteric fractures managed with a PFN. All patients were followed for at least 6 months. Regular anteroposterior (AP) and lateral view X-rays of the operated femur were taken when patients came for follow-ups and were analyzed for signs of radiological union and any mechanical failure.
Results: Patients with all three parameters in the acceptable range (i.e., TAD <25 mm, positive cortical reduction (PCR) in AP and lateral views, and maintained/restored integrity of the lateral cortical wall) showed comparatively better radiological outcomes with fracture union. Eight patients experienced mechanical failure and had two or more unmet radiological criteria.
Conclusions: This study highlights that achieving positive cortical support, preserving lateral wall integrity, and maintaining a TAD <25 mm intraoperatively are critical factors in reducing mechanical failure and improving radiological outcomes in intertrochanteric fractures treated with PFNs.
Keywords: Intertrochanteric fracture, proximal femoral nail, tip-apex distance, lateral wall, positive cortical support.
Intertrochanteric fractures are a significant concern in the aging population [1], accounting for 55% of all hip fractures in the elderly [2]. Despite advances in treatment, these injuries remain associated with high morbidity and mortality, with rates as high as 30.8% within a year [3]. While the vascular and cancellous nature of the bone contributes to a generally high union rate, achieving optimal functional outcomes remains a challenge [4]. Dynamic hip screws, though effective in some scenarios, have demonstrated limitations in managing unstable intertrochanteric fractures, including excessive screw sliding, screw cut-out, and malunion [5,6,7]. Proximal femoral nailing (PFN), with its superior biomechanical design, addresses these limitations by providing enhanced stability through better resistance to fracture collapse and support for the posteromedial wall [8,9,10]. However, despite the widespread adoption of PFN, complications such as implant failure and mechanical issues (e.g., screw cut-out and Z-effect) persist [11]. While several studies have explored these complications, there remains a gap in understanding the specific roles of key radiological parameters – tip-apex distance (TAD), lateral wall integrity, and cortical reduction type – in influencing surgical outcomes. This study aims to address this gap by analyzing the individual and combined impact of these parameters on radiological outcomes and mechanical failures, providing insights into optimizing the use of PFN in unstable intertrochanteric fractures.
After Institutional Ethics Committee approval (IRB no. TMH/IEC/JULY/163/2024), a retrospective non-randomized observational study was conducted in our institute, evaluating all patients who sustained intertrochanteric fractures from June 2021 to December 2023 and presented to our hospital. A total of 552 patients visited our hospital during the period. The COVID-19 pandemic struck the world during 2020–2022, and many of the patients were managed conservatively, and a lot of our geriatric patients perished in that pandemic. After fulfilling the inclusion and exclusion criteria, 100 patients (35 males and 65 females) were included in the study. Follow-up data included radiographic checks at 6 weeks, 3 months, and 6 months after surgery to assess signs of radiological union and any signs of mechanical failure in AP and lateral views.
Radiological measurement
During the immediate post-fixation period (C-arm fluoroscopic imaging) and at subsequent follow-up – 6 weeks, 3 months, and 6 months – standard anteroposterior (AP) radiographs of the hip were obtained. These images were captured with both legs positioned in 15° of internal rotation. Lateral radiographs were also taken with the contralateral hip flexed and abducted to optimize visualization. The quality of cortical reduction was evaluated in the immediate post-fixation fluoroscopic images in both AP and lateral views. In the AP view, it was classified based on the position of the medial cortex between the femoral head–neck fragment and the shaft:
- Positive cortical reduction (PCR): The medial cortex of the proximal head–neck fragment is positioned 1–2 mm medial to the medial cortex of the distal femoral shaft.
- Neutral position (NP): The medial cortices of the head–neck fragment and shaft are anatomically aligned.
- Negative cortical reduction (NCR): The medial cortex of the head–neck fragment is displaced 1–2 mm or more laterally to the medial cortex of the femoral shaft (Fig. 1).

Figure 1: Cortical reductions seen in anteroposterior views of the hip joint.
In the lateral view, reduction quality was assessed using the anterior cortical continuity between the head–neck fragment and the shaft fragment:
- PCR: The anterior cortex of the proximal head–neck fragment is positioned 1–2 mm anterior to the anterior cortex of the distal femoral shaft.
- NP: The anterior cortices of the head–neck fragment and shaft are anatomically aligned.
- NCR: The anterior cortex of the head–neck fragment is positioned posteriorly to the anterior cortex of the femoral shaft (Fig. 2).
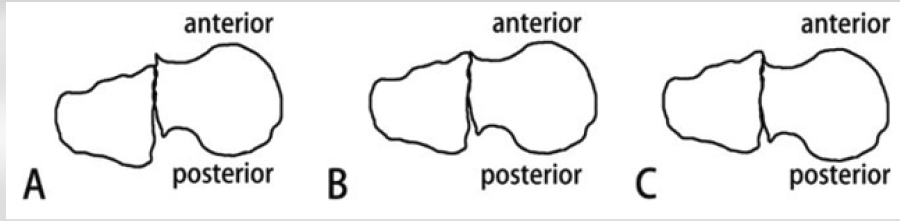
Figure 2: (a, b, c) Cortical reduction seen in lateral view of hip joint [12].
A reduction was classified as PCR only if the criteria were met in both AP and lateral views.
(Fig. 3)
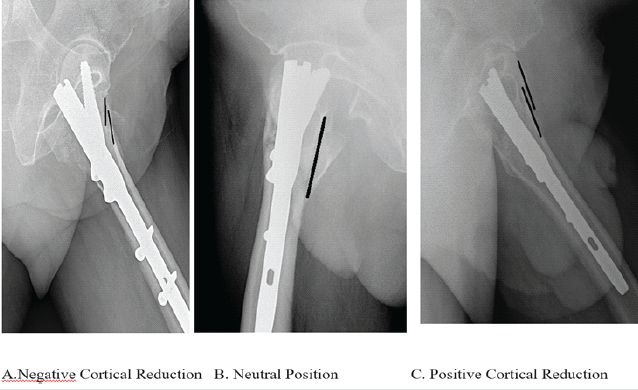
Figure 3: (a, b, c) X-ray images showing the type of reduction in the lateral view.
Validation
- Blinded observations: Radiographs were independently reviewed by two trained radiologists
- Agreement metrics: Interclass correlation coefficient (ICC) calculations ensured robust classification reliability across observers.
The TAD, introduced by Baumgaertner et al.[13]. It is widely regarded as the gold standard for predicting the risk of lag screw cut-out. This metric applies to the positioning of both intramedullary nails and sliding hip screws.
In this study, TAD was measured specifically in relation to the lag screw, excluding the derotation screw, with adjustments made to account for radiographic magnification [14], using the software available in the C-ARM fluoroscope and calibrating measurements with the known size of the PFN nail introduced in the fracture. TAD is calculated as the sum of two distances: The distance from the tip of the lag screw to the apex of the femoral head measured on the AP view (XAP) and the corresponding distance measured on the lateral view (XLat). Both measurements are corrected for magnification using the true diameter of the lag screw (Dt11rue) as a reference, i.e, TAD = XAP + XLat.
(Fig. 4)
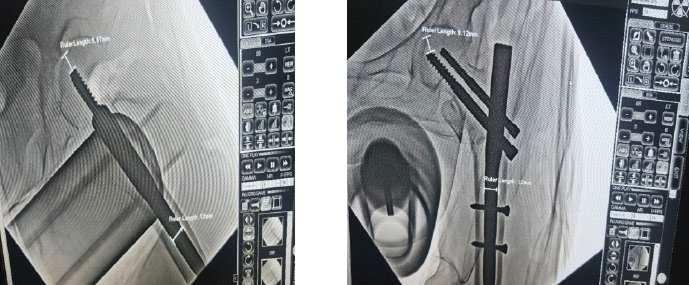
Figure 4: Tip apex distance in anteroposterior and lateral views.
- Validation process: TAD, a critical metric for predicting mechanical failure, was validated through standard protocols
- Standardized methodology: Measurements taken on AP and lateral radiographs using digital software, corrected for magnification
- Observer reliability: Two independent observers measured TAD for 20% of the sample, with results analyzed for consistency
- Statistical analysis: ICC > 0.75 confirmed excellent intra- and interobserver reliability.
Integrity of the lateral wall is important in the management of intertrochanteric fractures, as about 21% of intertrochanteric fractures following fixation have post-operative lateral wall fracture [15], and among those, 22% undergo reoperation, with the remainder having protracted healing time or shortening in limbs [16,17]. Lateral wall integrity is also important for providing lateral buttress support and preventing varus collapse. The lateral wall thickness is defined as the distance in mm from a reference point 3 cm below the innominate tubercle of the greater trochanter, angled at 135° upward to the fracture line (the midline between the two cortex lines) on anteroposterior radiograph [18] .Lateral wall thickness is a simple and quantitative parameter for the pre-evaluation of the integrity of the lateral wall. Lateral wall integrity was also assessed in the immediate post-operative X-rays to see if it was maintained or lost post-fixation. (Fig.5)

Figure 5: Lateral wall integrity is seen on the fluoroscopic image.
Statistical analysis
Data were collected using MS Excel. Continuous variables were expressed as mean (SD) and ranges; Categorical variables were expressed as numbers and percentages.
Comparison between two variables was assessed using the Chi-square test.
All tests were two-sided. A P < 0.05 was statistically significant. The analysis was done using Statistical Package for the Social Sciences version 21.0.
In this study, among 100 patients, 65 were female and 35 were male.
The age range of patients was from a minimum of 61 years to the most elderly patient of 93 years, with a mean age of about 71 years.
In this study, out of 100 patients, 62 had PCR, 24 had neutral reduction, and 14 patients had NCR.
Seventy-one of our patients’ lateral wall integrity was maintained.
Fifty-five of our patients had TAD <25 mm in AP and lateral views.
In patients with neutral reduction over the follow-up period, 25 % of them had collapsed to NCR. Three patients had a negative reduction at the end of 4 weeks, while the remaining patients got a negative reduction at the end of 6 months. (Fig. 6)
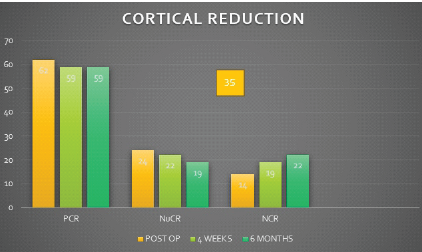
Figure 6: Bar graph showing the type of reduction in immediate post-operative, 4 weeks and 6 months
All these patients also had either TAD>25 or no lateral wall maintained. Five patients with a positive reduction in the immediate post-operative period were found to have neutral reduction at the end of 6 months.
Twenty-four of our patients had all three parameters within an acceptable range, and every one of them showed complete radiological union at the end of 6 months. None of those patients showed any implant failure, Z effect, or varus collapse. (Fig. 7)
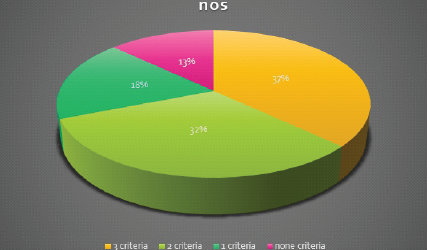
Figure 7: Pie chart showing the distribution of the sample with no of criteria fulfilled.
This study had 3 patients with Z-effect, 4 patients with varus collapse, and 2 patients who had to be reoperated due to implant failure. In patients with Z-effect, 2 presented at the end of 4 weeks and had all 3 parameters unfulfilled, while the other one presented at 6 months and had only one parameter out of three fulfilled. Out of four varus collapse patients, 2 with all 3 unmet parameters presented at the 4th week, while the rest 2 were seen at the end of 6 months, of which only 1 had a single unmet parameter. Implant failure is defined as a complete screw backing out or joint perforation leading to another surgery of the bone. In patients with mechanical failure, this type of reduction played an important role, as about 50% of patients with NCR had mechanical complications. The relation between mechanical failures and the number of unmet radiological parameters is shown in Table 1,while Table 2 shows distribution of patients according to parameters they met in immediate post op period. (Table 1-2).
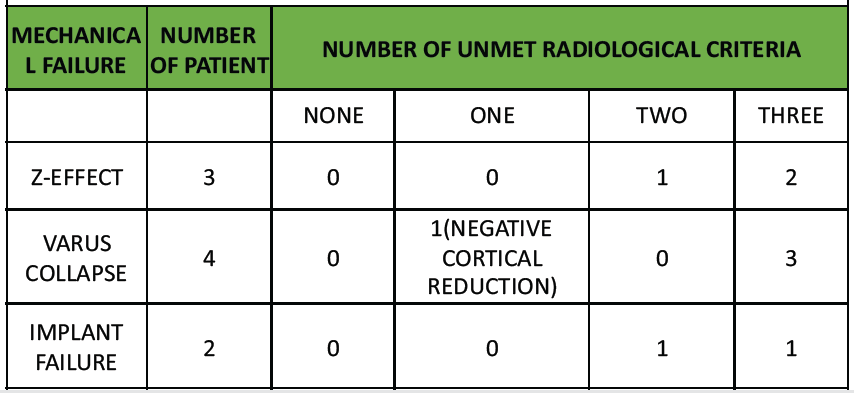
Table 1: Mechanical failure in relation to unmet radiological factors involved.

Table 2: Distribution according to the parameters met in the immediate post-operative period.
Unstable intertrochanteric fractures remain a major challenge in orthopedic surgery, particularly among the elderly, where reduced bone quality further complicates fracture management. PFN has gained widespread acceptance due to its superior biomechanical stability [19,20]. However, complications such as screw cut-out, Z-effect, and lateral wall fractures remain significant concerns, necessitating a focus on surgical precision and intraoperative planning [21,22,23]. This study underscores the importance of three critical radiological parameters – PCR, TAD, and lateral wall integrity-in determining successful surgical outcomes. The findings in this study are consistent with prior research. Baumgaertner et al. identified a TAD of <25 mm as a key predictor of reduced mechanical failure, an observation corroborated in this study. Kashigar et al.[24] and Shivashankar and Keshkar [25] also reported a higher risk of mechanical failure when TAD exceeded 25 mm, reinforcing our results. In addition, Gotfried [26] and Tan et al.[27] highlighted the role of lateral wall integrity in ensuring fracture stability and reducing complications, which was further validated in this investigation. PCR, as emphasized by Gotfried et al. [28] and expanded on by Chang et al., was also found to be instrumental in minimizing complications. When comparing complication rates with previous studies, notable differences emerge. Fogagnolo et al.[29] reported a complication rate of 23.4% with PFN, while Uzun et al.[30] observed non-union in 5.7% and varus collapse in 25.7% of cases. The comparatively lower complication rates in this study suggest that adherence to optimal intraoperative parameters – achieving proper TAD, maintaining lateral wall integrity, and ensuring PCR – can significantly improve outcomes. This reinforces the necessity of standardized surgical protocols and meticulous operative techniques in reducing mechanical failures.
Practical implications for surgical planning
The findings underscore the importance of specific intraoperative goals in managing unstable intertrochanteric fractures. Maintaining a TAD below 25 mm with the use of adequate screw length, ensuring lateral wall integrity (by adding trochanteric wiring/trochanteric buttress plate), and achieving PCR during initial fracture reduction and throughout the procedure are actionable targets that can be incorporated into surgical planning. Real-time radiographic assessment and careful reduction techniques are practical strategies to improve fixation stability and promote early mobilization in elderly patients.
Strengths of the study
A key strength of this analysis is the comprehensive evaluation of radiological parameters, offering insights into their combined impact rather than examining them in isolation. This approach provides a more holistic understanding of the factors influencing surgical outcomes and highlights actionable intraoperative targets for improving fracture stability and healing.
Limitation
Retrospective study design
The retrospective nature of the study may lead to selection and information bias. To minimize this limitation, strict inclusion and exclusion criteria were applied, and all available medical records and radiographic images were thoroughly analyzed. Radiological assessments were performed by two independent observers, and inter- and intra-observer reliability was statistically validated using the ICC, ensuring consistency in measurements. This has been mentioned in the discussion and conclusion sections, and it is recommended that future studies adopt a prospective design to further improve data quality and reduce bias.
Limited sample size and single-center data
This study had a limited sample size, and single-center nature of the restricts the generalizability of the findings. The study period was impacted by the COVID-19 pandemic, resulting in fewer eligible patients. Nonetheless, the sample size was sufficient to demonstrate significant trends regarding the impact of radiological parameters on outcomes. This study recommends future multicentric, larger cohort studies to validate and extend our findings.
Loss to follow-up
A substantial number of patients were lost to follow-up, mainly due to pandemic-related travel restrictions and health concerns. This has been transparently reported in the methodology section, and the possible impact on outcome completeness in the discussion is also highlighted. Despite this, it was ensured that the remaining cohort had a minimum follow-up of 6 months with consistent radiographic evaluations, providing valuable insights into fracture healing and mechanical complications.
Unmeasured confounding factors
Unmeasured confounding factors such as osteoporosis severity, nutritional status, and comorbidities may influence outcomes. Due to the retrospective nature of the study, uniform documentation for these variables was not available in patient records, and thus, these were not systematically included in the study. This study acknowledged this limitation and suggested that future studies incorporate these parameters through prospective data collection and multivariate analysis to better understand their contribution to fracture healing and implant stability.
Radiological outcome focus
Functional outcome scores provide a more comprehensive view of patient recovery and quality of life. However, the primary focus of this study was to evaluate radiological parameters influencing fracture healing and mechanical failures. This has been highlighted and it is recommended that future studies integrate validated functional outcome measures to establish correlations between radiological findings and patient-reported outcomes.
Measurement variability
Measurement variability cannot be eliminated, even with robust reliability testing. To mitigate this, standardized imaging protocols with proper limb positioning and digital measurement tools calibrated for magnification were used. In addition, measurements were independently reviewed by two experienced radiologists, and statistical analysis confirmed excellent inter- and intra-observer reliability (ICC >0.75).
Short- to mid-term follow-up
A longer follow-up would provide deeper insights into late complications and long-term implant performance. The current study’s follow-up period of at least 6 months was chosen to assess early union and mechanical failures, which are critical indicators of surgical success. This study clearly mentions this limitation and recommends that extended follow-up studies be conducted to explore the durability of the fixation and long-term functional outcomes.
No direct biomechanical correlation
Biomechanical testing would have provided a more direct validation of the relationship between radiological parameters and fracture stability; this study focused on clinical radiographic outcomes in a real-world surgical setting. Future research combining biomechanical experiments with clinical observations would certainly enrich understanding and provide stronger evidence supporting the role of these parameters in fracture management. Overall, while this study provides valuable insights into the impact of radiological parameters on outcomes of unstable intertrochanteric fractures treated with PFN, certain limitations must be acknowledged. These limitations underline the importance of conducting larger, multicentric, prospective studies with extended follow-up and incorporation of functional outcomes and biomechanical correlations to strengthen and validate the present findings.
Achieving fracture reduction with positive cortical support and valgus alignment ensures controlled sliding of the proximal fragment, maintaining femoral shaft contact and enhancing overall stability. This strategy minimizes the risk of varus collapse and reduces the likelihood of reoperation. Furthermore, maintaining a TAD of <25 mm is critical in preventing mechanical failure, while preservation of the lateral wall serves as a vital buttress against collapse. Although each parameter – optimal TAD, positive cortical support, and intact lateral wall integrity – independently improves outcomes, their combined effect provides the greatest protection against complications. The findings from this study emphasize that failure to achieve two or more of these intraoperative criteria markedly increases the risk of implant failure. Therefore, meticulous pre-operative planning, precise intraoperative technique, and strict adherence to these parameters are essential for optimizing fixation stability and ensuring successful fracture union in unstable intertrochanteric fractures.
For optimal surgical outcomes in unstable intertrochanteric fractures treated with proximal femoral nail, surgeons should aim to achieve a tip-apex distance (TAD) of <25 mm, secure positive cortical reduction in both anteroposterior and lateral views, and preserve the integrity of the lateral femoral wall. Failure to meet two or more of these parameters substantially increases the risk of mechanical complications such as implant failure, varus collapse, or Z‑effect. Meticulous preoperative planning, careful intraoperative execution, and adherence to these radiological and technical principles are therefore critical to ensuring stable fixation, reliable union, and improved patient outcomes.
References
- 1. Russell TA, Sanders R. Pertrochanteric hip fractures: Time for change. J Orthop Trauma 2011;25:189-90. [Google Scholar] [PubMed]
- 2. Herman A, Landau Y, Gutman G, Ougortsin V, Chechick A, Shazar N. Radiological evaluation of intertrochanteric fracture fixation by the proximal femoral nail. Injury 2012;43:856-63. [Google Scholar] [PubMed]
- 3. Jiang HX, Manjumdar SR, Dick DA, Moreau M, Raso J, Otto DD, et al. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res 2005;20:494-500. [Google Scholar] [PubMed]
- 4. Tsang ST, Aitken SA, Golay SK, Silverwood RK, Biant LC. When does hip fracture surgery fail? Injury 2014;45:1059-65. [Google Scholar] [PubMed]
- 5. Andruszkow H, Frink M, Frömke C, Matityahu A, Zeckey C, Mommsen P, et al. Tip apex distance, hip screw placement, and neck shaft angle as potential risk factors for cut-out failure of hip screws after surgical treatment of intertrochanteric fractures. Int Orthop 2012;36:2347-54. [Google Scholar] [PubMed]
- 6. Kokoroghiannis C, Aktselis I, Deligeorgis A, Fragkomichalos E, Papadimas D, Pappadas I. Evolving concepts of stability and intramedullary fixation of intertrochanteric fractures–a review. Injury 2012;43:686-93. [Google Scholar] [PubMed]
- 7. Kulkarni GS, Limaye R, Kulkarni M, Kulkarni S. Intertrochanteric fractures. Indian J Orthop 2006;40:16-23. [Google Scholar] [PubMed]
- 8. Gundle R, Gargan MF, Simpson AH. How to minimize failures of fixation of unstable intertrochanteric fractures. Injury 1995;26:611-4. [Google Scholar] [PubMed]
- 9. Simpson AH, Varty K, Dodd CA. Sliding hip screws: Modes of failure. Injury 1989;20:227-31. [Google Scholar] [PubMed]
- 10. Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res 1998;348:87-94. [Google Scholar] [PubMed]
- 11. Sadowski C, Lübbeke A, Saudan M, Riand N, Stern R, Hoffmeyer P. Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: A prospective, randomized study. J Bone Joint Surg Am 2002;84:372-81. [Google Scholar] [PubMed]
- 12. Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: A key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg 2015;135:811-8. [Google Scholar] [PubMed]
- 13. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am 1995;77:1058-64. [Google Scholar] [PubMed]
- 14. Khanna V, Tiwari M. Significance of tip apex distance in intertrochanteric fracture femur managed with proximal femoral nailing. Orthop Traumatol Surg Res 2021;107:103009. [Google Scholar] [PubMed]
- 15. Haidukewych GJ. Intertrochanteric fractures: Ten tips to improve results. J Bone Joint Surg Am 2009;91:712-9. [Google Scholar] [PubMed]
- 16. Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am 2001;83:643-50. [Google Scholar] [PubMed]
- 17. Palm H, Jacobsen S, Sonne-Holm S, Gebuhr P, Hip Fracture Study Group. Integrity of the lateral femoral wall in intertrochanteric hip fractures: An important predictor of a reoperation. J Bone Joint Surg Am 2007;89:470-5. [Google Scholar] [PubMed]
- 18. Hsu CE, Shih CM, Wang CC, Huang KC. Lateral femoral wall thickness. A reliable predictor of post-operative lateral wall fracture in intertrochanteric fractures. Bone Joint J 2013;95-B:1134-8. [Google Scholar] [PubMed]
- 19. Park SR, Kang JS, Kim HS, Lee WH, Kim YH. Treatment of intertrochanteric fracture with the gamma AP locking nail or by a compression hip screw–a randomised prospective trial. Int Orthop 1998;22:157-60. [Google Scholar] [PubMed]
- 20. Gadegone WG, Salphale YS. Short proximal femoral nail fixation for trochanteric fractures. J Orthop Surg (Hong Kong) 2010;18:39-44. [Google Scholar] [PubMed]
- 21. Mainds CC, Newman RJ. Implant failures in patients with proximal fractures of the femur treated with a sliding screw device. Injury 1989;20:98-100. [Google Scholar] [PubMed]
- 22. Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev 2008;3:CD000093. [Google Scholar] [PubMed]
- 23. Rethnam U, Cordell-Smith J, Kumar TM, Sinha A. Complex proximal femoral fractures in the elderly managed by reconstruction nailing – complications & outcomes: A retrospective analysis. J Trauma Manag Outcomes 2007;1:7. [Google Scholar] [PubMed]
- 24. Kashigar A, Vincent A, Gunton MJ, Backstein D, Safir O, Kuzyk PR. Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Joint J 2014;96-B:1029-34. [Google Scholar] [PubMed]
- 25. Shivashankar B, Keshkar S. Intertrochanteric fractures: Ten commandments for how to get good results with proximal femoral nailing. Indian J Orthop 2021;55:521-4. [Google Scholar] [PubMed]
- 26. Gotfried Y. The lateral trochanteric wall: A key element in the reconstruction of unstable pertrochanteric hip fractures. Clin Orthop Relat Res 2004;425:82-6. [Google Scholar] [PubMed]
- 27. Tan BY, Lau AC, Kwek EB. Morphology and fixation pitfalls of a highly unstable intertrochanteric fracture variant. J Orthop Surg (Hong Kong) 2015;23:142-5. [Google Scholar] [PubMed]
- 28. Gotfried Y, Kovalenko S, Fuchs D. Nonanatomical reduction of displaced subcapital femoral fractures (gotfried reduction). J Orthop Trauma 2013;27:e254-9. [Google Scholar] [PubMed]
- 29. Fogagnolo F, Kfuri M Jr., Paccola CA. Intramedullary fixation of pertrochanteric hip fractures with the short AO-ASIF proximal femoral nail. Arch Orthop Trauma Surg 2004;124:31-7. [Google Scholar] [PubMed]
- 30. Uzun M, Erturer E, Ozturk I, Akman S, Seckin F, Ozcelik IB. Longterm radiographic complications following treatment of unstable intertrochanteric femoral fractures with the proximal femoral nail and effects on functional results. Acta Orthop Traumatol Turc 2009;43:457-63. [Google Scholar] [PubMed]