Rotational malalignment is a common but often under-recognized complication after femoral intramedullary nailing that can significantly affect functional outcomes. By employing CT-based assessment, this study provides insights into preventing and identifying malrotation in post-operative patients
Dr. Navdeep Singh Keer, Sports Injury Centre, Vardhman Mahavir Medical College and Safdarjung Hospital, B-2/149 Paschim Vihar, Ansari Nagar West, New Delhi - 110029, India. E-mail: drnavdeepsinghkeer@gmail.com
Introduction: Rotational malalignment is a frequently overlooked yet clinically significant complication following closed intramedullary nailing (IMN) of femoral shaft fractures. Malrotation may result in functional impairment, altered gait biomechanics, and patient dissatisfaction. Computed tomography (CT) remains the most accurate modality for quantifying femoral torsion. This study aimed to determine the incidence, degree, and functional consequences of malrotation following IMN in diaphyseal and diaphyseo-metaphyseal femur fractures using CT-based assessment.
Materials and Methods: This prospective observational study was conducted at a tertiary trauma center in Delhi over 18 months. Thirty skeletally mature patients with closed diaphyseal or diaphyseo-metaphyseal femur fractures treated with closed antegrade IMN were included. Post-operative femoral torsion was assessed through axial CT scans using the method described by Jeanmart. Lower extremity functional scale (LEFS) scores were recorded preoperatively and at 6 weeks, 12 weeks, and 6 months postoperatively. Correlation analyses were performed between malrotation magnitude, fracture comminution, timing of surgery, and functional outcomes. Significant malrotation (defined as >10° difference compared to the contralateral limb) was observed in 20% of patients. Internal rotation deformities (mean: 12.6°) and external rotation deformities (mean: 8°) occurred in equal proportion. Malrotation >10° was significantly associated with lower LEFS scores at 6-month follow-up (P < 0.05). Fracture comminution and delay in surgical fixation (>10 days) were independently correlated with greater degrees of malrotation and worse functional recovery (P < 0.001 and P = 0.0086, respectively). All patients eventually achieved radiological union by 6 months.
Conclusion: CT-based assessment revealed a notable incidence of malrotation following IMN of femoral shaft fractures, with deformities >10° adversely affecting functional outcomes. Intraoperative vigilance in fracture reduction and early fixation may reduce the risk of malalignment. Routine CT evaluation in selected patients may be warranted to detect clinically relevant torsional deformities.
Keywords: Femoral fractures, intramedullary nailing, femur, bone malalignment, tomography, X-ray computed, treatment outcome.
Femoral shaft fractures are among the most common long-bone injuries encountered in orthopedic trauma, particularly affecting young males involved in high-energy mechanisms such as road traffic accidents and falls from height [1]. Closed antegrade intramedullary nailing (IMN) is the gold standard for surgical management of these fractures, offering biological fixation, minimal soft-tissue disruption, and early mobilization [2]. Despite these advantages, rotational malalignment remains a recognized complication of this technique, often underestimated both intraoperatively and in post-operative follow-up [3]. Malrotation following IMN can significantly alter lower limb biomechanics, lead to functional impairment, and cause long-term dissatisfaction, even in the presence of radiological union [4]. While various intraoperative techniques exist for assessing rotational alignment – such as the cortical step sign and lesser trochanter profile comparison – none are entirely reliable, especially in the absence of clear anatomical landmarks or in comminuted fractures [5]. Computed tomography (CT) remains the most accurate and reproducible method for post-operative evaluation of femoral torsion [6]. The prevalence and functional consequences of malrotation have been inconsistently reported in the literature, with limited data from the Indian subcontinent. Furthermore, there remains a lack of consensus on the threshold of clinical significance and its correlation with patient-reported outcomes. The present study was designed to evaluate the incidence and degree of femoral malrotation following IMN, using CT-based assessment, and to analyze its functional impact using validated scoring systems over serial follow-up.
This prospective observational study was conducted at a tertiary-level trauma center in Delhi over 18 months after obtaining approval from the respective institutional ethics committee. Written informed consent was obtained from all participants before inclusion. Thirty skeletally mature patients (aged ≥18 years) presenting with closed diaphyseal or diaphyseo-metaphyseal femoral fractures who were managed with closed antegrade IMN were enrolled consecutively. Patients with pathological fractures, compound injuries, old neglected fractures, abnormal femoral anteversion in the contralateral limb, uncontrolled systemic comorbidities, or pregnancy were excluded from the study. All procedures were performed under spinal anesthesia with the patient positioned supine on a fracture table. A standard lateral approach was used to access the proximal femur. Closed reduction was achieved using traction and image intensifier guidance. Rotational alignment was approximated intraoperatively by evaluating the cortical diameter and lesser trochanter profile compared to the contralateral limb. Post-operative assessment of femoral torsion was performed using CT. The rotational alignment was measured using the Jeanmart method [6], which calculates the angle between a line drawn along the posterior condylar axis distally and a line through the femoral neck axis proximally (Fig. 1).

Figure 1: Computed tomography (CT)-based measurement of femoral malrotation using the Jeanmart method. Axial CT slices at the femoral neck and condylar levels demonstrating angle α on the operated side and angle β on the contralateral side; the difference (α-β) represents the degree of femoral malrotation.
The difference in femoral torsion between the operated and contralateral limbs was recorded. A discrepancy >10° was defined as significant malrotation. Functional outcomes were assessed using the lower extremity functional scale (LEFS), recorded preoperatively and at 6 weeks, 12 weeks, and 6 months postoperatively. Radiographic union was assessed at each follow-up visit using standard anteroposterior and lateral femur radiographs. Statistical analysis was performed using the Statistical Package for the Social Sciences version 21.0. Descriptive statistics were used to summarise baseline characteristics. T-tests and Pearson correlation coefficients were applied where appropriate, and a P < 0.05 was considered statistically significant.
Demographic and injury characteristics
A total of 30 patients were included in the study. The mean age was 28.7 years, with 70% of patients under the age of 30 years. Males constituted 86.7% (n = 26) of the cohort. The most frequent fracture pattern was diaphyseal (56%), followed by subtrochanteric/diaphyseo-metaphyseal (44%). Road traffic accidents were the leading mechanism of injury (56.6%). These baseline characteristics are depicted in Table 1.
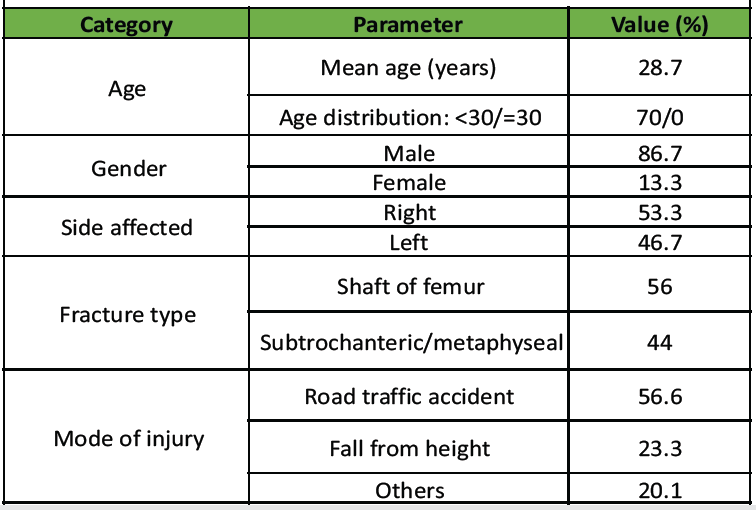
Table 1: Baseline demographic and injury characteristics
Post-operative malrotation analysis
CT-based assessment revealed that 50% of patients had internal rotation deformity (mean: 12.6°) and 50% had external rotation deformity (mean: 8.0°). Significant malrotation, defined as a torsional discrepancy of >10° between the operated and contralateral limb, was observed in 20% (n = 6) of patients.
Correlation with fracture comminution
Preoperative comminution at the fracture site was observed in 53% (n = 16) of cases. Patients with comminuted fractures demonstrated a significantly higher mean degree of malrotation (10.4° ± 2.1) compared to those without comminution (5.4° ± 2.0), with a P < 0.001.
LEFS score progression and correlation with degree of malrotation
The mean LEFS score improved progressively across follow-up intervals: 7.9 preoperatively, 32.1 at 6 weeks, 47.2 at 12 weeks, and 66.6 at 6 months. These improvements were statistically significant (P < 0.001). At 6 months, patients with malrotation >10° demonstrated significantly lower LEFS scores compared to those with ≤10° malrotation (P < 0.05), indicating impaired functional recovery (Fig. 2).
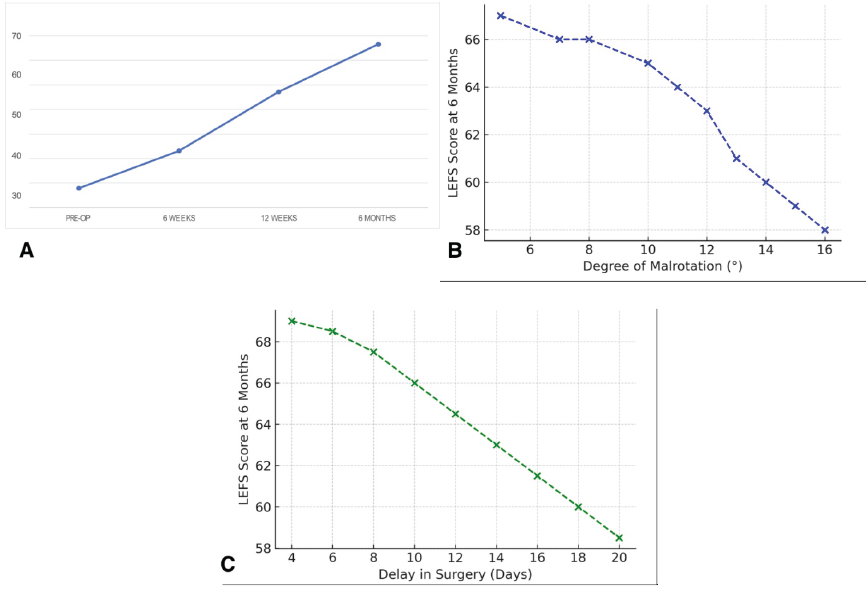
Figure 2: Functional and correlation analysis of post-operative outcomes (a) shows the progressive improvement in lower extremity functional scale (LEFS) scores from preoperative to 6-month follow-up. (b) demonstrates a negative correlation between LEFS scores and the degree of malrotation. (c) illustrates the decline in LEFS scores with increasing delay in surgical fixation.
Correlation between timing of surgery and LEFS scores
Delayed surgical fixation (>10 days from injury) was associated with significantly lower LEFS scores at final follow-up (mean 65.1 vs. 68.2; P = 0.0086). This suggests that prolonged intervals before definitive fixation may adversely affect functional outcomes, possibly due to difficulty in achieving optimal closed reduction (Fig. 2). The post-operative radiological and functional outcomes, along with their correlations, are depicted in Table 2.
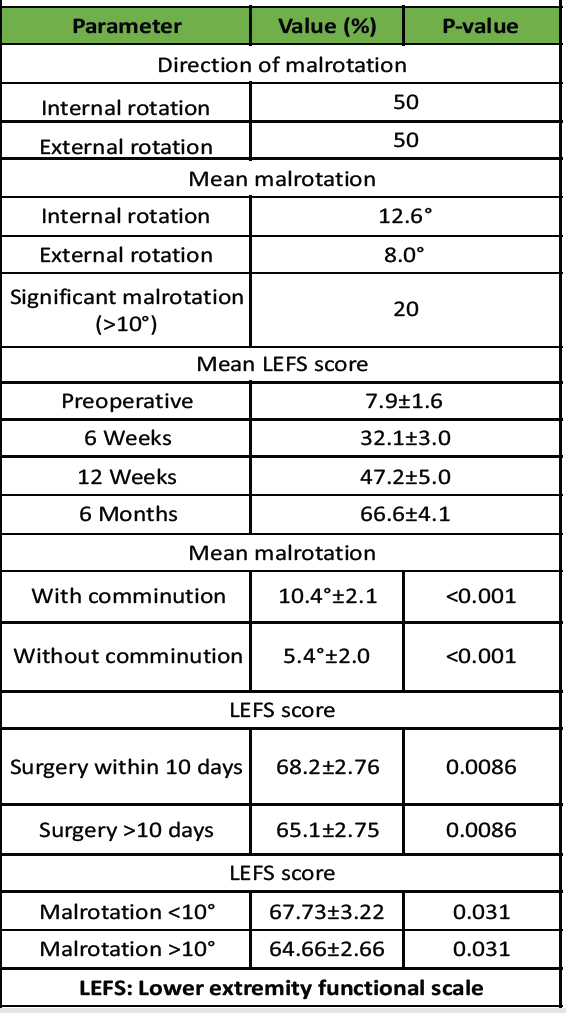
Table 2: Post-operative outcomes and correlation analysis
Radiological union and patient satisfaction
Radiographic evidence of union was observed in all patients by 6 months. Sixty percent of patients showed signs of union by 12 weeks. All patients reported satisfaction with the outcome at final follow-up, regardless of malrotation status.
The most important finding of this study was that 20% of patients treated with closed IMN for femoral shaft and diaphyseo-metaphyseal fractures developed clinically significant malrotation (>10°), as determined by CT. Furthermore, this malrotation correlated with impaired functional outcomes, particularly when exceeding 10°, and was more prevalent in comminuted fractures and cases with delayed surgical fixation. These findings reinforce previous literature suggesting that malrotation is an under-recognized but clinically meaningful complication following IMN. Jaarsma et al. reported a malrotation rate of 28% and found external rotational deformities to be associated with greater difficulty in activities involving higher functional demand [4]. Mansouri-Tehrani et al. found 5–10° of malrotation postoperatively after femur nailing in 75.7% of their patients [7]. Our study similarly found both internal and external malrotations to impair function when exceeding the 10° threshold, as evidenced by reduced LEFS scores at 6 months. The correlation between fracture comminution and higher degrees of malrotation highlights the challenge of achieving accurate torsional alignment when fracture morphology provides limited reference points. Similar associations have been previously noted, with Johnson and Greenberg attributing malalignment to the difficulty in controlling fragments during closed reduction [8]. Timing of surgery also emerged as a significant factor. Patients operated on after more than 10 days post-injury exhibited lower functional outcomes, likely due to callus formation and increased technical difficulty in achieving anatomical reduction. This aligns with earlier studies that emphasise the importance of early fixation in optimising mechanical alignment [9]. The study reaffirms that CT-based torsional measurement, particularly using the Jeanmart method, remains the most reliable tool for assessing rotational alignment postoperatively [6]. Given the high incidence of undetected malrotation and its functional impact, selective use of post-operative CT scans in high-risk cases may be justified [8,10]. The primary limitations of this study include a relatively small sample size, which may limit the generalisability of the findings. The lack of long-term follow-up beyond 6 months precludes assessment of delayed functional deficits or degenerative changes. In addition, intraoperative rotational assessment methods were not standardized, reflecting variability but introducing potential confounding.
Rotational malalignment following IMN of femoral shaft fractures is a frequently overlooked issue that can significantly affect functional outcomes, especially when the deformity exceeds 10°. This study found that such malrotation was more likely in comminuted fractures and when surgery was delayed. These findings emphasise the importance of meticulous intraoperative technique to ensure proper rotational alignment. The use of CT for assessing post-operative torsion provides a reliable means of detecting clinically relevant malrotation and may be particularly useful in selected cases. By linking radiological malalignment with patient function, this study adds valuable insight to a topic that remains underreported, particularly in the Indian population, and supports the need for greater awareness and standardization in addressing femoral rotational alignment.
Rotational malalignment following IMN of femoral shaft fractures is a frequently overlooked issue that can significantly affect functional outcomes, especially when the deformity exceeds 10°. The use of CT for assessing post-operative torsion provides a reliable means of detecting clinically relevant malrotation and may be particularly useful in selected cases.
References
- 1. Salminen ST, Pihlajamaki HK, Avikainen VJ, Böstman OM. Population based epidemiologic and morphologic study of femoral shaft fractures. Clin Orthop Relat Res 2000;372:241-9. [Google Scholar] [PubMed]
- 2. Winquist RA, Hansen ST Jr., Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am 1984;66:529-39. [Google Scholar] [PubMed]
- 3. Bråten M, Terjesen T, Rossvoll I. Torsional deformity after intramedullary nailing of femoral shaft fractures. J Bone Joint Surg Br 2002;75:799-803. [Google Scholar] [PubMed]
- 4. Jaarsma RL, Pakvis DF, Verdonschot N, Biert J, Van Kampen A. Rotational malalignment after intramedullary nailing of femoral fractures. J Orthop Trauma 2004;18:403-9. [Google Scholar] [PubMed]
- 5. Jaarsma RL, Verdonschot N, Van der Venne R, Van Kampen A. Avoiding rotational malalignment after fractures of the femur by using the profile of the lesser trochanter: An in vitro study. Arch Orthop Trauma Surg 2005;125:184-7. [Google Scholar] [PubMed]
- 6. Jeanmart L, Baert AL, Wackenheim A. Computer tomography of neck, chest, spine and limbs. In: Atlas of Pathologic Computer Tomography. Vol. 3. London: Springer; 1983. p. 171-7. [Google Scholar] [PubMed]
- 7. Pape HC, Rixen D, Morley J, Husebye EE, Mueller M, Dumont C, et al. Impact of the method of initial stabilization for femoral shaft fractures in patients with multiple injuries at risk for complications (borderline patients). Ann Surg 2007;246:491-9; discussion 499-501. [Google Scholar] [PubMed]
- 8. Mansouri-Tehrani MM, Yavari P, Moosayii D, Eslami S, Nourian SM. Evaluation of femoral malrotation after intramedullary nailing. Int J Burns Trauma 2021;11:418-23. [Google Scholar] [PubMed]
- 9. Johnson KD, Greenberg M. Comminuted femoral shaft fractures. Orthop Clin North Am 1987;18:133-47. [Google Scholar] [PubMed]
- 10. Branca Vergano L, Coviello G, Monesi M. Rotational malalignment in femoral nailing: Prevention, diagnosis and surgical correction. Acta Biomed 2020;91:e2020003. [Google Scholar] [PubMed]