The primary goal of metacarpal fracture fixation is to restore bony alignment and stability to allow early mobilization and functional recovery, while minimizing complications such as stiffness, malunion, or tendon adhesions.
Dr. Makesh Ram Sriraghavan2Department of Orthopaedics, Periyar Government Hospital-Madras Medical College, Chennai - 82, Tamil Nadu, India. E-mail: ram23ortho@yahoo.com
Introduction: Metacarpal fractures are one of the most commonly encountered musculoskeletal injuries in the hand often caused by road traffic accidents, trivial fall or workplace injuries. It can lead to severe disability of the hand if left untreated or improperly treated. About 88% of all metacarpal fractures are non-thumb metacarpals, with the fifth finger being most frequently affected. Hence, achieving optimal function will be the primary goal, though it remains challenging.
Materials and Methods: A prospective study done at Government Thoothukudi Medical College for a period of 3 years from March 2022 to February 2025. There are about 40 patients of multiple metacarpal fractures fixed with K-wire and Herbert screws. Each group consists of 20 patients. Both groups are followed up at 3rd week, 6th week, 10th week, and 16th week postoperatively. Assessment done by radiological union, grip strength, range of movements, early return to activity, and disability of arm, shoulder, and hand (DASH) score.
Results: A significantly shorter time to fracture union in the Herbert screw group, compared to K-wire group, was observed. Herbert screw group demonstrated better range of movements, early return to activity and grip strength postoperatively. DASH questionnaire showed excellent results in the Herbert screw group compared to K-wire group.
Conclusion: Our study concludes that healing time was significantly lower in the Herbert screw group. Range of movements and grip strength was also better in the Herbert screw group. Thus, we conclude that the Herbert screw has a better functional outcome in the management of displaced metacarpal shaft fractures compared to the K-wire group.
Keywords: Metacarpal fracture, K-wire, Herbert screw, disability of arm, shoulder, and hand questionnaire.
Metacarpal fractures account for about 40% of all hand injuries [1,2,3]. Metacarpal fractures are common hand injuries, accounting for 30–50% of all hand fractures [4]. Few metacarpal fractures necessitate surgical intervention, and the majority can be treated conservatively. The treatment aims to restore function, maintain joint mobility, and ensure early return to daily activities [5,6]. Various fixation methods have evolved to provide stable fixation and allow early mobilization. Improperly treated hand injuries result in shortening, rotation, and angulation of the metacarpals, resulting in severe functional disability, loss of strength, and flexibility of the hand – even affecting the day-to-day activities of the patient. Although undisplaced metacarpal fractures are treated conservatively, displaced metacarpal shaft fractures need proper reduction and internal fixation to limit the disability [7,8]. Various methods of fixation are available for metacarpal shaft fractures, such as K-wire fixation, miniplate fixation, and Herbert screw fixation [9,10]. K-wire fixation was the first surgical modality employed in the treatment of displaced metacarpal shaft fractures. However, as it leads to less stable fracture fixation – more cases of malunion, non-union and infection had been reported paving the way for new modalities of fixation like miniplates and headless intramedullary compression screws – Herbert screws [11,12]. Miniplates are not so popular due to the potential complications of implant irritation and skin necrosis.
Aim
This study aims to find out the functional outcome of metacarpal shaft fractures treated by K-wires and Herbert screws and to evaluate grip strength, pain, and return to daily activities.
The present study is a prospective study carried out over a 3-year period (March 2022 to February 2025) in the Department of Orthopedics at Government Thoothukudi Medical College Hospital, Tamil Nadu, India. Patients with displaced metacarpal fractures requiring surgical treatment were enrolled in the study after taking informed written consent, two groups were enrolled in the study. Group A (case) consisted of 20 metacarpal fractures for whom K-wire fixation done and Group B (control) consisted of 20 metacarpal fractures for whom Herbert screw fixation done. Surgical method of K-wire fixation and Herbert screw fixation was divided on alternate basis to avoid bias. We included multiple metacarpal shaft fractures with an age range from 18 to 60 years and fractures sustained with <1 week duration. Intra-articular fractures, comminuted fractures, pathological fractures and compound fractures were excluded from the study.
Surgical technique
Group A (K-wire fixation)
Patient in supine, with affected limb in arm table, parts painted and draped. Retrograde K-wire technique was used. A skin incision of size 0.5 cm was made over the dorsal aspect of metacarpophalangeal (MCP) joint. Extensor tendons incised and retracted medially and laterally. A 1.5 mm K-wire was selected and inserted over the dorsal aspect of the metacarpal head after closed reduction of the fracture by traction and digital manipulation under fluoroscopic guidance. With fracture in reduction, K-wire was passed across the fracture site up to the base of the metacarpal. Protruding K-wire was bent and cut externally (Fig. 1a, b, c, d).

Figure 1: (a and b) Pre-operative X-ray left hand showing # of 3rd, 4th, 5th metacarpals, and (c and d) Post-operative X-ray after K-wire fixation.
Post-operative immobilization was done with a volar splint for 4 weeks by protocol in fear of loss of fracture reduction. Out of 20 cases, three cases needed percutaneous reduction of fracture. Initially, for the first six cases, we used only single K-wires, and after we started using multiple K-wires (Fig. 2a, b, c).

Figure 2: (a) # of 4th, 5th metacarpal shaft, (b) fixed with multiple K-wires, and (c) after wire removal at 10th week.
Group B (Herbert screw fixation)
Patient in supine, with affected limb in arm table, parts painted and draped. A skin incision of size 1 cm was made over the dorsal aspect of MCP joint. Extensor tendons incised longitudinally with proximal phalanx in maximal flexion to expose the metacarpal head. After closed reduction of the fracture, a guide wire was inserted from the metacarpal head and passed across the fracture site. With fracture in reduction, medullary canal reaming is done with a cannulated drill bit. Appropriate size Herbert screw inserted and tightened – interfragmentary compression achieved (Fig. 3a, b, c, d). Head of the screw must be buried under the metacarpal head to prevent joint irritation (Fig. 4a, b, c, d). Wound wash given. Suturing done in layers. Sterile dressing done. Post-operative immobilization was not done. Out of 20 cases, two cases needed percutaneous reduction of fracture.
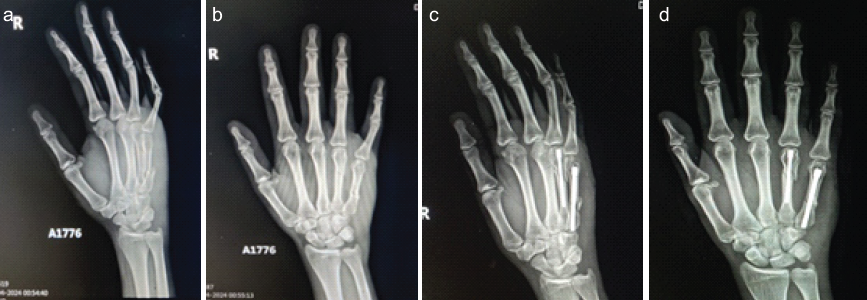
Figure 3: (a and b) Pre-operative X-ray left hand showing # of 4th, 5th metacarpals, and (c and d) after Herbert screw fixation.
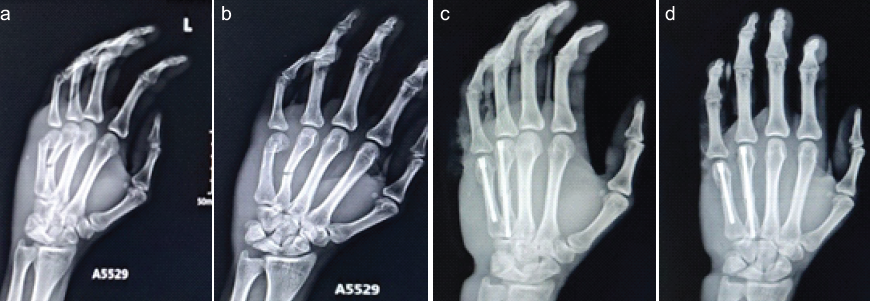
Figure 4: (a and b) Pre-operative X-ray left hand showing # of 4th, 5th metacarpals, and (c and d) after Herbert screw fixation.
Post-operative follow-up
Patients in both groups were followed up for a period of 6 months. They were reviewed at 3rd week, 6th week, 10th week, and 16th week postoperatively. During those reviews, X-rays were taken to find out the radiological evidence of union. Furthermore, during each visit- the functional assessment was done by range of movements, return to activity, grip strength and disability of arm, shoulder and hand (DASH) questionnaire [13]. After obtaining the data, results were interpreted statistically.
Demography characteristic
In our study, the mean age was higher in the K-wire group, and male predominance were noted in both the groups. There was almost equal number of fracture distribution pertaining to the fracture pattern in both the groups (Table 1).
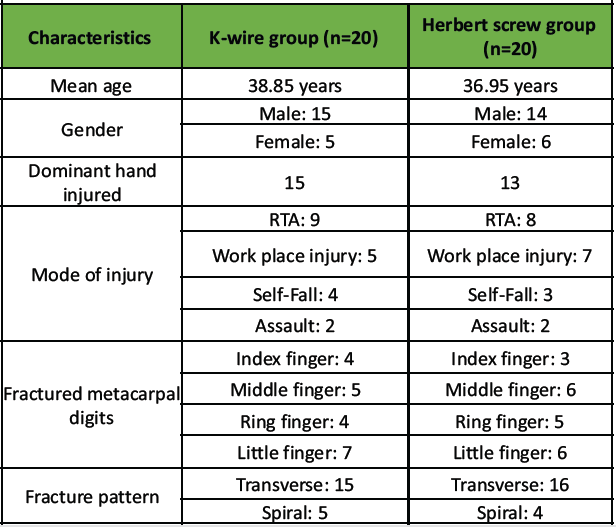
Table 1: The various demography characteristic in both the groups
Functional outcome analysis and DASH score [14]
We observed that the duration of surgical time was comparatively less in K-wire group, but the range of motion, DASH score and radiological healing were good in Herbert screw group (Table 2).
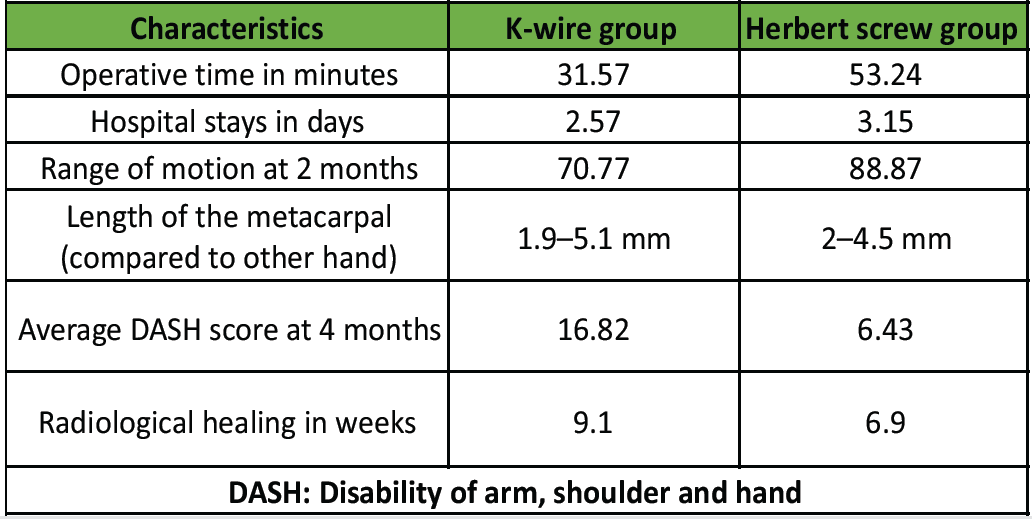
Table 2: The functional analysis and its characteristics
The length of the involved metacarpal was compared to the opposite side and we noticed that there was only few mm length difference in both the groups. Furthermore, the rotational deformity was very minimum. Grip strength and total active motion of fingers comparatively good in Herbert screw group at 3–6 months follow-up (Table 3 and 4). There was an excellent outcome for 13 cases in the Herbert screw group and three cases of poor outcome in K-wire group (Table 3).
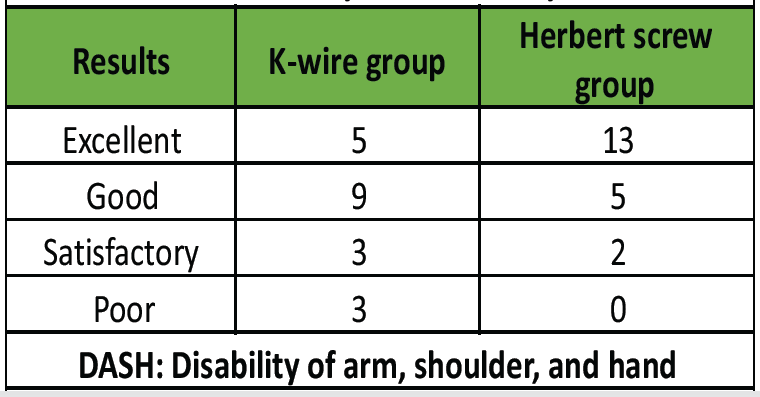
Table 3: Outcome analysis assessed by DASH score
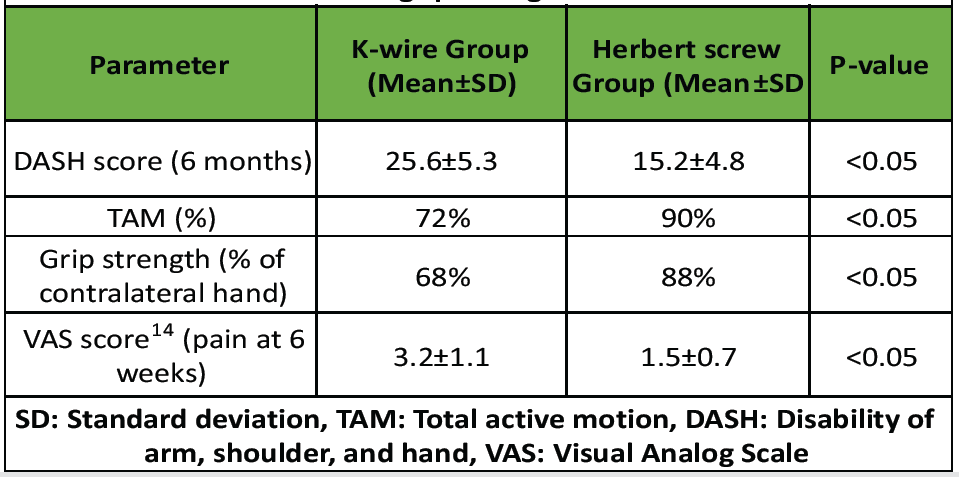
Table 4: The grip strength and TAM%
Complications
In our series, we noted stiffness of MCP and interphalangeal joints was more in K-wire group compared to Herbert screw group. At the same time, recovery of finger stiffness was early in Herbert screw group. We also noted pin tract infection in K-wire group, which also lead to implant loosening, and subsequently they were removed at 3–4 weeks (Table 5).
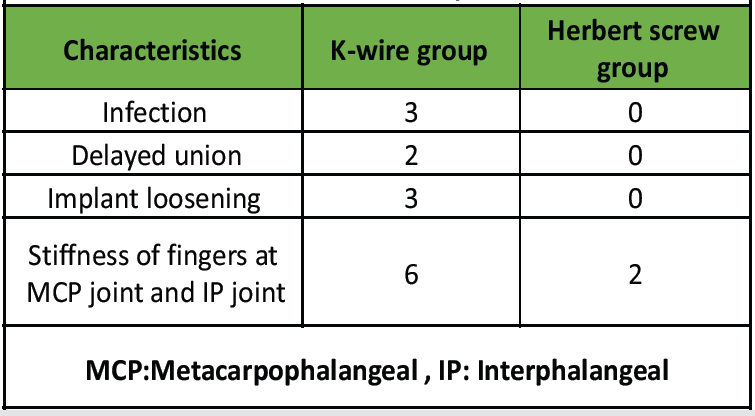
Table 5: Observed complications
Metacarpal fractures are often neglected or regarded as trivial injuries. Hand injury may cause significant disability from loss of sensation, loss of strength, and flexibility [15,16]. Considerable judgment is required to select the appropriate modality. K-wire fixation is cost-effective, simpler, and widely used, but carries risks such as pin tract infection, secondary displacement, and need for wire removal [1]. Herbert screws offer rigid internal fixation, allow early mobilization, and are buried beneath the skin, reducing infection risk and discomfort. In our study, the Herbert screw group showed significantly better functional outcomes, less pain, and faster return to activities. However, Herbert screws require more technical expertise, are costlier, and are only suitable for certain fracture patterns; surgery is inevitable in unstable and displaced hand fractures. Out of various treatment options available for internal fixation, K-wires and Herbert screw fixations predominates. Results of the previous studies comparing these two treatment modalities were inconclusive. The present study was thus planned to evaluate the clinical and radiological outcome of patients of metacarpal fractures with Herbert screw fixation and K-wire. A previous study done by Lv F. et al. [17] revealed more operating time in the Herbert screw group [16]. Most common location of fractures was observed as shaft followed by base and then neck. The results of our study showed that fracture healing time of Herbert screw group was significantly shorter than K-wire group which matched the previous study done by Lv F, et al. [17]. The incidence of post-operative complications in our study in Herbert screw group was lower than that in K-wire group with a statistically significant difference. The previous comparative study was done by Lv F, et al. [17]. The clinical results were similar in K-wire and Herbert screw group. In our study, the clinical results were significantly better in Herbert screw group in terms of grip strength of hand, DASH score and time of union.
The present study observed that fixation of fracture metacarpal with Herbert screw is a better option than K-wire fixation. It effectively provides patients with better stability, which promotes faster fracture healing and early joint function recovery. Better functional outcome was observed after Herbert screw fixation, along with a lower incidence of post-operative complications. Hence, we conclude that Herbert screw fixation is more effective than K-wire fixation in the management of metacarpal fractures. We recommend Herbert screw fixation in transverse or short oblique fractures with good bone stock. However, K-wire remains a viable option in resource-limited settings or in comminuted fractures unsuitable for screw fixation. Further large-scale studies with longer follow-up are recommended.
Both K-wire and Herbert screw fixation are effective in achieving union in non-thumb metacarpal shaft fractures. However, Herbert screw fixation demonstrates superior early functional outcomes, allows quicker return to activity, and is associated with fewer complications.
References
- 1. Gocke T. Metacarpal fractures: A review of fracture characteristics and treatment options. JBJS J Orthop Physician Assist 2023;11:e22.00018. [Google Scholar] [PubMed]
- 2. Lambi AG, Rowland RJ, Brady NW, Rodriguez DE, Mercer DM. Metacarpal fractures. J Hand Surg Eur Vol 2023;48 2 Suppl:42S-50. [Google Scholar] [PubMed]
- 3. Soong M, Got C, Katarincic J. Ring and little finger metacarpal fractures: mechanisms, locations, and radiographic parameters. J Hand Surg 2010;35:1256-9. [Google Scholar] [PubMed]
- 4. Maslow JI, Gaston RG. Metacarpal fractures. In: Skeletal Trauma of the Upper Extremity. Netherlands: Elsevier; 2022. p. 572-85. [Google Scholar] [PubMed]
- 5. Jerome JT. Metacarpal and Phalangeal Fractures and Fractures-Dislocations. Orthopaedics and Trauma: Current Concepts and Best Practices. Cham: Springer; 2024. p. 259-88. [Google Scholar] [PubMed]
- 6. McNemar TB, Howell JW, Chang E. Management of metacarpal fractures. J Hand Ther 2003;16:143-51. [Google Scholar] [PubMed]
- 7. Haughton DN, Jordan D, Malahias M, Hindocha S, Khan W. Principles of hand fracture management. Open Orthop J 2012;6:43-53. [Google Scholar] [PubMed]
- 8. Taha RH, Grindlay D, Deshmukh S, Montgomery A, Davis TR, Karantana A. A systematic review of treatment interventions for metacarpal shaft fractures in adults. Hand (N Y) 2022;17:869-78. [Google Scholar] [PubMed]
- 9. Kamath JB, Harshvardhan, Naik DM, Bansal A. Current concepts in managing fractures of metacarpal and phalangess. Indian J Plastic Surg 2011;44:203-11. [Google Scholar] [PubMed]
- 10. Rausch V, Harbrecht A, Kahmann SL, Fenten T, Jovanovic N, Hackl M, et al. Osteosynthesis of phalangeal fractures: Biomechanical comparison of Kirschner wires, plates, and compression screws. J Hand Surg Am 2020;45:987.e1-8. [Google Scholar] [PubMed]
- 11. Meals C, Meals R. Hand fractures: A review of current treatment strategies. J Hand Surg Am 2013;38:1021-31; quiz 1031. [Google Scholar] [PubMed]
- 12. Lee SK, Kim KJ, Choy WS. Modified retrograde percutaneous intramedullary multiple Kirschner wire fixation for treatment of unstable displaced metacarpal neck and shaft fractures. Eur J Orthop Surg Traumatol 2013;23:535-43. [Google Scholar] [PubMed]
- 13. Supichyangur K, Tananon T, Sripakdee SA, Chunyawongsak V. Prospective comparison of the early outcomes of headless compression screw and percutaneous K-wire fixation in metacarpal fractures. J Hand Surg Am 2023;48:950.e1-9. [Google Scholar] [PubMed]
- 14. Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): Validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord 2006;7:44. [Google Scholar] [PubMed]
- 15. Gülke J, Leopold B, Grözinger D, Drews B, Paschke S, Wachter NJ. Postoperative treatment of metacarpal fractures-classical physical therapy compared with a home exercise program. J Hand Ther 2018;31:20-8. [Google Scholar] [PubMed]
- 16. Keck K, Dogaroiu A, Aribert M, Awaida C, Odobescu A. Retrograde intramedullary pinning of metacarpal fractures through the collateral recess. Tech Hand Up Extrem Surg 2025;29:e0500. [Google Scholar] [PubMed]
- 17. Lv F, Nie Q, Guo J, Tang M. Comparative analysis of the effects of AO mini-plate and Kirschner wire pinning in the metacarpal fractures: A retrospective study. Medicine (Baltimore) 2021;100:e26566. [Google Scholar] [PubMed]









