Posterior decompression and stabilization offer effective neurological recovery, pain relief, and deformity correction in thoracolumbar spinal tuberculosis with minimal morbidity and quicker rehabilitation. The posterior-only approach provides stable fusion and adequate decompression while being practical and resource-efficient. Even in resource-limited settings, it delivers reliable clinical and radiological outcomes comparable to more extensive surgical methods.
Dr. Dharam Kabir Panthi, Department of Orthopaedics, Gandhi Medical College, Bhopal, Room No 205, SR-JR Building, Dadaji Dhunewale District Hospital Campus, Khandwa - 450001, Madhya Pradesh, India. E-mail: dharampanthi1994@gmail.com
Introduction: Spinal tuberculosis (TB) remains a common cause of spinal infection worldwide and may result in severe neurological deficits and progressive deformity if not treated appropriately. While anti-tubercular therapy (ATT) is the cornerstone of management, surgical intervention is indicated in patients with neurological deterioration or mechanical instability. Posterior decompression and stabilization have emerged as a safe and effective surgical option.
Aim: The aim of the study is to evaluate the functional and radiological outcomes in patients with thoracic and lumbar TB treated by posterior decompression and stabilization.
Materials and Methods: A prospective observational study was conducted on 30 patients with thoracic, lumbar, or thoracolumbar spinal TB between July 2022 and December 2023. Indications for surgery included neurological deterioration, sensory or sphincter deficits, recurrent neurological complications, or lack of improvement after 6 weeks of ATT. Functional outcomes were evaluated using the Visual Analog Scale (VAS) for pain, the American Spinal Injury Association impairment scale for neurological function, and the combined Prolo scale for functional and economic recovery. Radiological outcomes were assessed by kyphotic angle correction and Bridewell grading, while neurological recovery was additionally assessed by Kumar and Tuli’s classification. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were measured to monitor inflammatory activity.
Results: The mean patient age was 39.9 ± 14.4 years, with higher female prevalence and more frequent thoracic involvement. The mean intraoperative blood loss was 266 ± 50.1 mL, mean operative time was 2.46 ± 0.41 h, and mean hospital stay was 13.9 ± 4.7 days. At final follow-up, the mean VAS score improved significantly to 2.33 ± 0.99. Mean ESR and CRP declined to 25.5 ± 5.5 mm/h and 16 ± 6.1 mg/L, respectively. The mean post-operative kyphotic correction was 11.7° ± 3.8°, with a mean correction loss of 3.4° ± 1.4° at final follow-up. Functional evaluation showed excellent recovery in 50% of patients on the Prolo scale, and 57.1% achieved Grade I fusion according to Bridewell criteria.
Conclusion: Posterior decompression and stabilization are safe and effective surgical strategies for thoracolumbar spinal TB. It provides reliable decompression, neurological recovery, deformity correction with maintenance, early mobilization, shorter hospital stays, and minimal complications, making it a viable option in resource-limited settings.
Keywords: Thoracolumbar Pott’s spine, posterior decompression, stabilization, Visual Analog Scale, Prolo scale, neurological recovery, deformity correction.
Tuberculosis (TB) continues to pose a significant health burden in underdeveloped nations, while its incidence has decreased in developed countries due to increased sanitation, nutrition, and hygiene, even before the introduction of anti-tubercular therapy (ATT). Nevertheless, a resurgence of TB, particularly spinal TB, has been observed in developed regions, largely due to the increasing prevalence of human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome, immigration, and the prolonged survival of immunocompromised individuals. Globally, TB accounted for 1.4 million deaths in 2014, reflecting its major impact on public health [1]. Spinal TB, or Pott’s disease, is the most common and severe form of skeletal TB, representing nearly half of all osteoarticular cases [2]. It may result in bone destruction, severe kyphotic deformity, and paraplegia. Management strategies vary widely, ranging from conservative treatment with ATT alone to more invasive procedures such as anterior-only or combined anterior-posterior surgeries [3]. Historically, anterior debridement and reconstruction were considered the gold standard for surgical management. However, with advances in imaging, earlier detection of spinal TB is now possible, enabling treatment at a stage where less invasive procedures can achieve similar results. Posterior instrumentation has increasingly emerged as the preferred surgical approach in thoracolumbar and lumbar spinal TB, offering three-column stabilization and circumferential decompression with reduced morbidity [3,4,5].
This prospective observational study was conducted between July 2022 and December 2023 following approval from the institutional ethics committee. 30 patients with thoracic, lumbar, or thoracolumbar spinal TB who fulfilled the inclusion criteria were enrolled. Patients presenting with neurological deterioration, sensory or sphincter disturbances, recurrent neurological complications, or failure to improve after 6 weeks of adequate ATT were included, whereas patients with spinal pathologies other than TB, such as tumors or metastases, those with active pulmonary or abdominal TB, and those deemed unfit for surgery were excluded. Informed consent was obtained from all participants before enrollment. Diagnosis was established through detailed clinical history and radiological evaluation and confirmed by cartridge-based nucleic acid amplification test (CBNAAT) and/or histopathological biopsy. Radiological investigations included plain radiographs and contrast-enhanced magnetic resonance imaging to identify the extent of vertebral involvement, presence of abscesses, skip lesions, and cord compression. Routine pre-operative hematological investigations, along with inflammatory markers such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), were obtained. All patients underwent posterior decompression and stabilization following detailed counseling regarding surgical options. Patient outcomes were assessed preoperatively and at subsequent follow-ups. The response to infection control was monitored by serial ESR and CRP levels. Back pain was considered as pain and its severity was assessed using the Visual Analog Scale (VAS), while motor and sensory function was graded with the American Spinal Injury Association (ASIA) impairment scale. Functional and economic recovery to measure the quality of life (QoL) was evaluated using the Combined Prolo scale at each follow-up visit. Radiological assessment included measurement of the kyphotic angle (k-angle) on lateral radiographs to determine deformity correction and subsequent loss of correction, along with fusion grading based on the Bridewell classification. The neurological status of patients was also evaluated at each follow-up using Kumar and Tuli’s neurological grading system. This study was conducted as a prospective observational design to objectively document early clinical, functional, and radiological outcomes following posterior decompression and stabilization in thoracolumbar spinal TB. A single-arm design was chosen intentionally to ensure procedural uniformity and to eliminate the confounding effects of surgeon variability or heterogeneous operative approaches. This design allowed consistent data collection, protocol-driven management, and accurate follow-up, providing a clear reflection of real-world outcomes in a controlled institutional environment.
Surgical technique
All patients underwent surgery under general anesthesia in the prone position using a posterior approach. Prophylactic antibiotics were administered before incision. The operative level was confirmed with fluoroscopy, and a midline incision was made. Following incision of the subcutaneous tissue and fascia, the erector spinae muscles were subperiosteally stripped bilaterally along the spinous processes. Pedicle screws were inserted one or two levels above and below the diseased segment. Thorough debridement of necrotic tissue and drainage of pus were performed, followed by decompression of the spinal cord using laminotomy or laminectomy and a transpedicular approach, as required. Pedicle screws were connected with pre-contoured rods, and tissue samples were obtained for CBNAAT, histopathological examination, pus culture and sensitivity, and fungal culture and sensitivity. Autologous bone grafts were placed posterolaterally to promote fusion. Wound closure was performed in layers over a No. 14 drain. Immediate post-operative radiographs were obtained to assess implant position and k-angle correction. The drain was removed once output was <30 mL over 24 h. Patients were allowed to sit with appropriate braces from the 2nd post-operative day, and the wound was inspected during dressing change. Ambulation with braces and walker support was initiated when neurological status permitted. All patients continued ATT postoperatively. Bracing was advised for 3 months, and no patient received corticosteroids during the perioperative period.
Post-operative assessment
Patients were followed up at 6 weeks, 3 months, 9 months, and at the final follow-up at 12 months in the outpatient department. Clinical, functional, radiological, and biochemical parameters were recorded and compared with pre-operative values at each visit.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences version 26. Continuous variables were expressed as mean ± standard deviation, while categorical variables were presented as proportions. Statistical comparisons for qualitative data were performed using the Chi-square test and the proportion test. Quantitative variables were analyzed using the Gaussian test, Student’s paired t-test, Wilcoxon rank test, and analysis of variance, as appropriate. A P < 0.05 was considered statistically significant.
The mean age of the study population was 39.9 ± 14.38 years, with a female predominance (56.67%, n = 17) compared to males (43.33%, n = 13). Educational status revealed that 26.67% had completed higher secondary education, while 23.33% were illiterate. Indications for surgery included progressive neurological deficits in 9 patients (30%), sensory and sphincter disturbances in 4 (13.33%), recurrent neurological deterioration in 2 (6.67%), and failure to improve after adequate ATT in 13 (43.33%). The mean intraoperative blood loss was 266.67 ± 50.06 mL, with an average operative time of 2.46 ± 0.41 h. The mean hospital stay was 13.87 ± 4.68 days. Clonus was observed in 6 patients (16.67%), while skip lesions were identified in one patient (3.33%). Intraoperative samples tested positive on CBNAAT in 10 patients (30%), including one case of multidrug-resistant TB. Dorsal spine involvement was noted in 17 patients (56.67%), while 13 patients (43.33%) had lumbar spine disease. Most patients (73.33%) had no comorbidities; however, one patient each had acute cerebellar peduncle infarction with diabetes, isolated HIV, and combined diabetes–hypertension–HIV, while 4 patients (13.33%) were hypertensive.
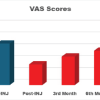
Pain outcomes (VAS)
The mean pre-operative Visual Analog Scale (VAS) score was 7.07, which improved to 3.67 postoperatively and further to 2.33 at final follow-up, demonstrating a statistically significant reduction (P < 0.001) (Fig. 1).
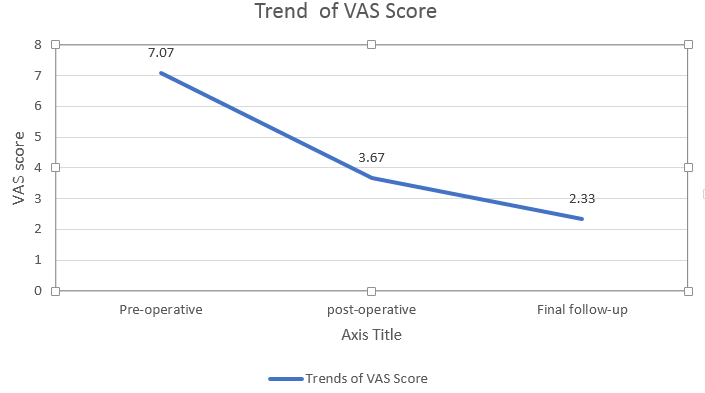
Figure 1: Trends of Visual Analog Scale scores over time.
Neurological recovery (ASIA scale)
Preoperatively, 24 patients (80%) had neurological involvement. Of these, 12 (40%) were graded ASIA D, 4 (13.33%) ASIA C, 2 (6.67%) ASIA B, and 6 (20%) ASIA A, while 6 patients (20%) had no deficit (ASIA E). At final follow-up, 93.33% of patients improved by at least one ASIA grade, with no patients remaining in grade A. Neurological recovery to ASIA E was achieved in 20 patients (71.42%), while 4 (14.28%) improved to ASIA B, and 2 each (7.14%) to ASIA C and D. Two patients died in the post-operative period (Fig. 2).
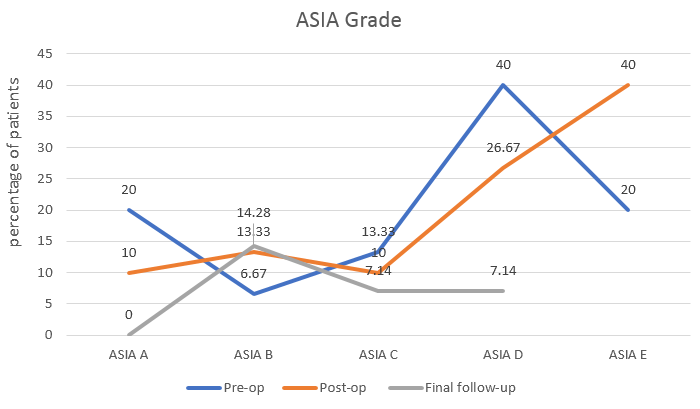
Figure 2: Neurological improvement.
Neurological recovery (Kumar and Tuli’s grading)
Preoperatively, 8 patients (26.67%) were in grade 1, 10 (33.33%) in grade 2, 8 (26.67%) in grade 3, and 4 (13.33%) in grade 4. At final follow-up, 20 patients (71.43%) were in grade 1, 6 (21.42%) in grade 3, and 2 (7.14%) in grade 2. No patient remained in grade 4. The improvement was statistically significant (P < 0.005), with 99.33% showing recovery by at least one grade (Fig. 3).
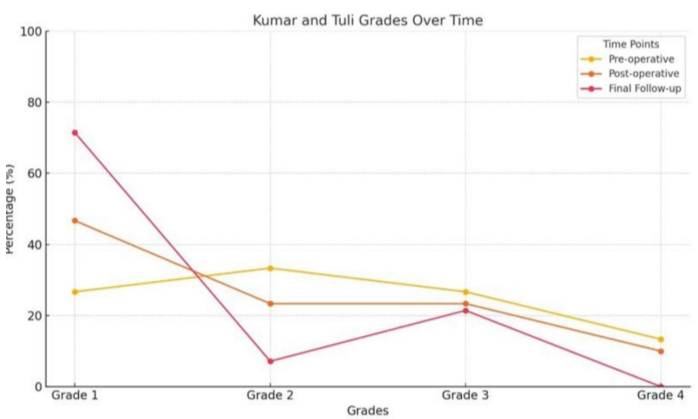
Figure 3: Improvement in Kumar and Tuli’s grade.
Inflammatory markers
Mean pre-operative ESR and CRP values were 59.53 ± 20.7 mm/h and 33.0 ± 15.52 mg/L, respectively, which reduced significantly at final follow-up to 25.33 ± 5.49 mm/h and 16.00 ± 6.06 mg/L (P < 0.0001) (Fig. 4).
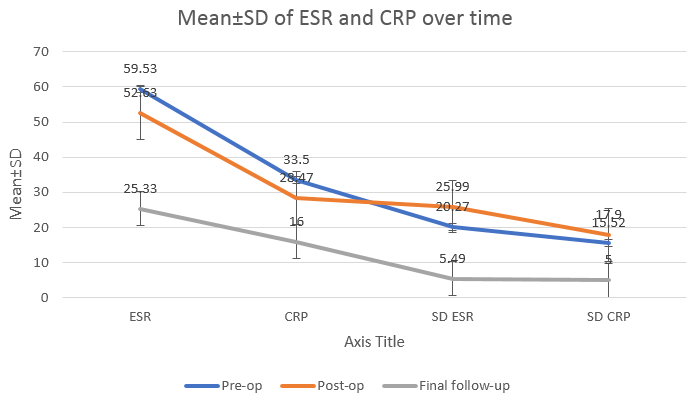
Figure 4: Trend of erythrocyte sedimentation rate and C-reactive protein.
Radiological outcomes (k-angle)
The mean pre-operative k-angle was 26 ± 9.94°, which improved to 11.70 ± 3.79° postoperatively. A mean loss of correction of 3.42 ± 1.35° was observed at final follow-up (P < 0.0001) (Figs. 5, 6, 7).
 Figure 5: Pre-operative kyphotic angle.
Figure 5: Pre-operative kyphotic angle.

Figure 6: Post-operative kyphotic angle.

Figure 7: Final follow-up.
Fusion outcomes (Bridewell grading)
At the final follow-up, 16 patients (57.14%) achieved Grade I fusion, 11 (39.29%) had Grade II and 1 patient (3.57%) had Grade III fusion. Despite radiological evidence of incomplete fusion, the Grade III patient remained asymptomatic, functionally independent, and radiologically stable. The summary of results is shown in Table 1.
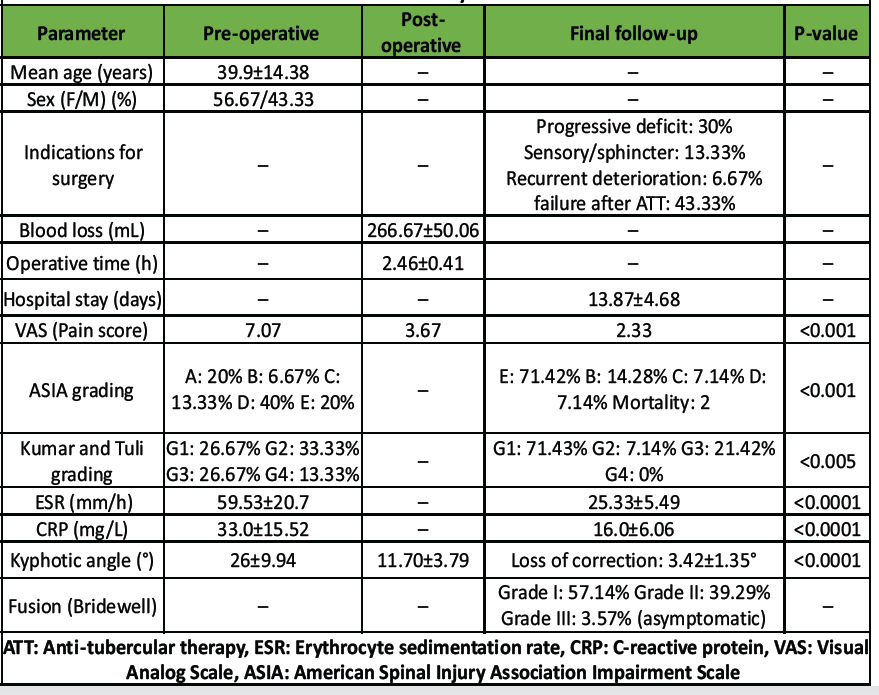
Table 1: Summary of results
The present study evaluated clinical and radiological outcomes of posterior decompression and stabilization in 30 patients with thoracic or lumbar spinal TB. Our results suggest that this approach is effective and safe, offering pain relief, three-column stabilization, neurological recovery, deformity correction, and functional improvement. These benefits are particularly relevant in resource-limited settings, where posterior-only instrumentation is feasible, economical, and associated with fewer complications compared with traditional anterior approaches. While ATT, strict rest, and supportive care remain the mainstay of treatment for Pott’s spine, they do not prevent progressive kyphotic deformity, thereby justifying surgical intervention in selected cases. The prospective observational design was intentionally selected to evaluate the outcomes of a standardized posterior decompression and stabilization technique in a uniform patient cohort. Unlike retrospective analyses, this approach allowed for predefined inclusion criteria, structured data acquisition, and systematic follow-up. Although it does not provide the inferential strength of randomized comparative studies, it offers valuable real-world clinical evidence and highlights the reproducibility and safety of the posterior-only approach under consistent surgical and institutional conditions. Historically, the anterior-only approach allowed direct access for debridement and decompression but was associated with limitations, particularly at the lumbosacral junction due to vascular anatomy, and carried risks of pleural effusion, atelectasis, blood loss, neurological injury, and prolonged immobilization. Comparative studies, such as that by Huang et al. [6], demonstrated similar outcomes in deformity correction, pain relief, and neurological recovery between anterior and posterior approaches, but with reduced operative morbidity in the posterior group. In our series, the mean age was 39.9 years, comparable to Anand et al. [7], with a higher prevalence in females. The mean loss of blood was 266.67 ± 50.06 mL, consistent with Lee et al. [4] study, and Huang et al. [6] in their anterior versus posterior approach found lesser blood loss in patients operated on by the posterior approach. Operative duration averaged 2.46 ± 0.41 h, which was shorter than the anterior approach (2.9 h) reported by Huang et al. [6] and comparable to that of Kire et al. [8]. The mean hospital stay was 13.9 ± 4.7 days, influenced by patients’ socioeconomic status and distance of residence, yet shorter than that reported for anterior surgery (25.5 ± 5.26 days) as shown by Huang et al. [6]. Similar observations were made by Zhou et al. [9], although their posterior cohort demonstrated slightly longer stays compared with ours. Microbiological confirmation with CBNAAT was achieved in 30% of patients, including one multidrug-resistant case. This yield, although apparently low, is comparable to previous reports (25–45%) due to the paucibacillary nature of spinal TB, difficulty in obtaining representative samples, and frequent necrosis or fibrosis in the diseased tissue. While CBNAAT remains a valuable rapid diagnostic tool, its sensitivity in osseous TB is limited compared to pulmonary samples. Therefore, the diagnosis in our study relied on a composite reference standard comprising clinical, radiological, and histopathological correlation, along with therapeutic response. Future research incorporating advanced molecular diagnostics or extended culture techniques may enhance the detection of resistant strains and microbial diversity. This yield was lower than the 45.7% reported by Guha et al. [10], highlighting that despite its high sensitivity and specificity, CBNAAT may not detect all the cases. Another potential source of bias arises from the selective inclusion of patients who were medically fit for surgery and met the defined eligibility criteria. This selection inherently excludes patients with extensive disease, uncontrolled systemic TB, or poor general health. Although this may limit the external applicability of our findings, it was necessary to ensure patient safety and to achieve homogeneity in surgical and perioperative management. By restricting the cohort to operable and optimized patients, the study maintained procedural uniformity and allowed a clearer assessment of the true outcomes attributable to the posterior decompression and stabilization technique. Pain outcomes in our series showed a significant reduction in VAS scores from 7.1 preoperatively to 2.3 at final follow-up (P < 0.001), in line with reports by Prakashappa et al. [11] and D’Souza et al. [12]. The reduction in the VAS score is due to 3-column stabilization in posterior instrumentation, which in turn reduces the inflammation and infection at the disease site. The neurological outcomes assessed using the ASIA scale showed that 71.4% of patients achieved complete recovery, while 93.3% improved by at least one grade, consistent with prior findings by Rawall et al. and Zeng et al. [13,14], and Jain et al. [15]. None of the patients remained in ASIA grade D, and 93.33% of the patients improved by at least one grade at final follow-up, further reinforcing the efficacy of posterior decompression and stabilization. Kyphotic correction averaged 11.7° ± 3.8° with a mean loss of correction of 3.4° ± 1.4° at final follow-up, comparable to Jain et al. [15] and favorable compared with anterior fixation results reported by Kim et al. [16]. Posterior pedicle screw instrumentation provides robust three-column fixation, likely accounting for the lower progression of kyphosis in our series compared to anterior approaches. Inflammatory markers also showed significant improvement, with ESR and CRP values declining to near-normal levels at follow-up, echoing findings by Zeng et al. [14], Prakashhappa et al. [11], and Broner et al. [17]. In this study, biological monitoring was limited to conventional inflammatory markers – ESR and CRP – which are established indicators of infection control and therapeutic response in spinal TB. Although more advanced biochemical and immunological markers such as interleukin profiles, bone-specific alkaline phosphatase, or osteocalcin could provide deeper insight into bone healing and immune modulation, their use was not feasible due to financial and technical limitations. Furthermore, the clinical utility of such markers in routine follow-up of spinal TB remains investigational. Future research incorporating these parameters may help elucidate long-term biological responses and optimize treatment monitoring. Radiological fusion was achieved in nearly all patients, with only one patient remaining in Bridewell grade 1 but clinically asymptomatic. Spinal TB typically heals by bony ankylosis, which reduces the necessity for anterior cage augmentation in most cases. Our findings align with those of Prakashappa et al. [11] and Lee et al. [4], who also reported satisfactory posterolateral fusion and maintenance of alignment without the routine use of cages. In the present study, kyphotic correction and fusion grading were evaluated using plain radiographs, which provide a reliable, cost-effective, and low-radiation method for post-operative monitoring in spinal TB. Although computed tomography (CT) scans could offer a more objective and detailed assessment of fusion, their routine use was avoided due to financial constraints and the desire to minimize radiation exposure, particularly in younger patients. This approach aligns with previous clinical series that have validated plain radiographs as an acceptable tool for assessing deformity correction and bony consolidation in tuberculous spondylitis. Nevertheless, future studies incorporating CT-based fusion assessment may further enhance objectivity and precision in radiological evaluation. Functionally, the majority of our patients regained their pre-illness level of activity, similar to outcomes reported by Anand et al. [7] using the Prolo scale. Although the VAS, ASIA grading, and Combined Prolo scale were used to assess pain, neurological status, and functional recovery, the study did not incorporate broad-based quality-of-life assessment tools such as the Short Form-36 or Oswestry disability index. This was primarily due to the focus on disease-specific parameters and practical feasibility within a resource-limited tertiary care setting. However, future studies incorporating validated global QoL instruments would allow a more comprehensive assessment of patient outcomes, including psychosocial and functional domains beyond surgical recovery.
Limitation
The major limitation of our study is the relatively small sample size (n = 30), which limits the statistical power and generalizability of our findings. However, the prospective design, uniform surgical protocol, and consistent follow-up lend reliability to the observed trends. Larger multicentric studies with extended follow-up are warranted to confirm these results. Another limitation of the present study is the relatively short follow-up duration of 12 months. While this period was sufficient to evaluate early post-operative pain relief, neurological recovery, deformity correction, and fusion, it may not fully reflect long-term outcomes such as recurrence, implant failure, or late progression of deformity. Longer follow-up studies are needed to determine the durability and stability of posterior instrumentation over time and to identify delayed complications that may influence ultimate functional results. In addition, the study reflects the experience of a single tertiary care center where all surgeries were performed using a standardized posterior decompression and stabilization technique by a single surgical team. While this uniformity strengthens the internal validity of the study, it may limit the external applicability of the results to other institutions with differing resources, surgical expertise, or case profiles. Multicentric studies with larger and more diverse patient populations are recommended to validate these findings across varied clinical environments. In addition, selection bias may exist since only surgically fit patients were included, potentially underrepresenting outcomes in those with advanced disease or poor general condition. Radiological fusion was assessed by plain radiographs without CT confirmation, which may have limited the objectivity of fusion assessment but minimized unnecessary radiation exposure. The absence of randomization and blinding in this prospective observational study may have introduced potential selection and observer bias. However, randomization was not feasible, as the study was designed to evaluate a single standardized surgical approach rather than to compare different treatment modalities. All surgeries were performed by the same senior surgical team following a uniform operative protocol, ensuring technical consistency. Furthermore, post-operative clinical and radiological evaluations were performed by independent assessors to minimize bias in outcome measurement. Although blinding could not be implemented, the prospective design and standardized methodology helped maintain objectivity and reproducibility in data collection.
Posterior decompression and stabilization for thoracolumbar spinal TB demonstrated significant neurological recovery, pain reduction, deformity correction, and improvement in functional outcomes, with minimal complications. The approach was associated with shorter operative times, reduced intraoperative blood loss, decreased hospital stay, and effective infection control, making it particularly suitable for developing regions with limited resources. Given its safety profile and favorable clinical outcomes, the posterior-only approach represents a reliable primary surgical option for thoracolumbar Pott’s spine. Nevertheless, larger prospective studies with extended follow-up are warranted to validate these findings and further define long-term outcomes. Although the sample size was limited, the findings provide meaningful clinical insight and form a basis for future larger-scale studies evaluating posterior decompression and stabilization in thoracolumbar spinal TB. Furthermore, as this study reports only short-term results, long-term follow-up is essential to assess implant longevity, deformity progression, and recurrence risk. As this work represents a single-institutional experience, its applicability may vary in centers with different clinical infrastructure or surgical practices; hence, multicentric validation is encouraged.
Posterior decompression and stabilization provide effective neurological recovery, pain relief, and deformity correction in thoracolumbar spinal TB. The posterior-only approach ensures adequate decompression and stable fusion with reduced morbidity, shorter hospital stay, and early mobilization. It represents a safe, practical, resource-efficient surgical option in thoracolumbar TB of the spine.
References
- 1. Global Tuberculosis Report 2015. 20th ed. Available from: https://www.who.int/publications/i/item/9789241565059 [Last accessed on 2024 Jun 24]. [Google Scholar] [PubMed]
- 2. World Health Organization. Global Tuberculosis Control: WHO Report 2010. World Health Organization; 2010. Available from: https://iris.who.int/handle/10665/44425 [Last accessed on 2024 Jun 24]. [Google Scholar] [PubMed]
- 3. Sahoo MM, Mahapatra SK, Sethi GC, Dash SK. Posterior-only approach surgery for fixation and decompression of thoracolumbar spinal tuberculosis: A retrospective study. J Spinal Disord Tech 2012;25:E217-23. [Google Scholar] [PubMed]
- 4. Lee TC, Lu K, Yang LC, Huang HY, Liang CL. Transpedicular instrumentation as an adjunct in the treatment of thoracolumbar and lumbar spine tuberculosis with early stage bone destruction. J Neurosurg 1999;91:163-9. [Google Scholar] [PubMed]
- 5. Chacko AG, Moorthy RK, Chandy MJ. The transpedicular approach in the management of thoracic spine tuberculosis: A short-term follow up study. Spine (Phila Pa 1976) 2004;29:E363-7. [Google Scholar] [PubMed]
- 6. Huang Z, Liu J, Ma K. Posterior versus anterior approach surgery for thoracolumbar spinal tuberculosis. J Coll Physicians Surg Pak 2019;29:187-8. [Google Scholar] [PubMed]
- 7. Anand MG, Kumar GP, Ku K. Evaluation of functional and Radiological outcome of anterior spinal decompression and stabilisation in the thoracolumbar potts’s spine: A prospective study. Int J Orthop Sci 2020;6:1-5. [Google Scholar] [PubMed]
- 8. Kire N, Kundnani VG, Jain S, Sagane SS, Asati S. Surgical outcomes of posterior trans-facetal decompression and stabilisation in tuberculous spondylodiscitis with neuro-deficit. J Clin Orthop Trauma 2021;16:35-42. [Google Scholar] [PubMed]
- 9. Zhou Y, Li W, Liu J, Gong L, Luo J. Comparison of single posterior debridement, bone grafting and instrumentation with single-stage anterior debridement, bone grafting and posterior instrumentation in the treatment of thoracic and thoracolumbar spinal tuberculosis. BMC Surg 2018;18:71. [Google Scholar] [PubMed]
- 10. Guha M, Lal H, Boruah T, Kumar S, Sareen A, Patralekh MK, et al. Clinico-Radio-histopathological correlation by C-arm image-guided biopsy in spinal tuberculosis. IJOO 2021;55:1028-36. [Google Scholar] [PubMed]
- 11. Prakashappa TH, Mohan NS, Shyamsundar Y. A prospective study of functional outcome in Thoracolumbar potts spine with posterior only approach. Int J Orthop Sci 2021;7:667-72. [Google Scholar] [PubMed]
- 12. D’Souza AR, Mohapatra B, Bansal ML, Das K. Role of posterior stabilization and transpedicular decompression in the treatment of thoracic and thoracolumbar TB: A retrospective evaluation. Clin Spine Surg 2017;30:E1426-33. [Google Scholar] [PubMed]
- 13. Rawall S, Mohan K, Nene A. Posterior approach in thoracolumbar tuberculosis: A clinical and radiological review of 67 operated cases. Musculoskelet Surg 2013;97:67-75. [Google Scholar] [PubMed]
- 14. Zeng Y, Wu W, Lyu J, Liu X, Tan J, Li Z, et al. Single-stage posterior debridement, decompression and transpedicular screw fixation for the treatment of thoracolumbar junction (T12-L1) tuberculosis with associated neurological deficit: A multicentre retrospective study. BMC Musculoskelet Disord 2019;20:95. [Google Scholar] [PubMed]
- 15. Jain A, Jain RK, Kiyawat V. Evaluation of outcome of transpedicular decompression and instrumented fusion in thoracic and thoracolumbar tuberculosis. Asian Spine J 2017;11:31-6. [Google Scholar] [PubMed]
- 16. Kim KS, Ko SH, Youm KS, Choi CH, Yang JH. Anterior spinal instrumentation in treatment of spinal tuberculosis. J Korean Orthop Assoc 2015;33:1560-8. [Google Scholar] [PubMed]
- 17. Broner FA, Garland DE, Zigler JE. Spinal infections in the immunocompromised host. Orthop Clin North Am 1996;27:37-46. [Google Scholar] [PubMed]