Early total care (ETC) with prompt mobilization is key in managing rare cases of simultaneous bilateral proximal femoral fractures.
Dr. Bekteshi Labinot, University Clinic of Surgical Diseases “St. Naum Ohridski,” Skopje, North Macedonia. E-mail: bekteshilabinot@gmail.com
Introduction: Simultaneous and bilateral proximal femoral fractures (PFF) are very rare, and only a few cases have been reported so far. A case of simultaneous and bilateral extra capsular PFF is presented.
Case Report: An 85-year-old male patient, who was hit by a car as a pedestrian, was diagnosed with PFF consisting of both an intertrochanteric and a subtrochanteric fracture. He underwent intramedullary fixation for both fractures without any relevant complications and started early mobilization.
Conclusion: Simultaneous bilateral extracapsular BFF are very rare therefore PFF management is not well established. Our goal was early total care accompanied with early mobilization and ambulation.
Keywords: Simultaneous and bilateral proximal femoral fractures, elderly, high-energy trauma, intramedullary fixation.
Simultaneous and bilateral proximal femoral fractures (PFF) are very rare, and only a few cases have been reported so far. According to Rodriguez-Zamorano, “this fracture pattern has generally been described for femoral neck fractures and in association with high-energy trauma, systemic diseases that involve bone structure alterations (primary hyperparathyroidism, multiple myeloma, metastatic disease, chronic kidney failure, or cirrhosis), and as a result of violent seizures” [1]. Bilateral extracapsular PFF have been rarely reported in relation to high-energy trauma in the elderly [2]. A case of high-energy trauma involving simultaneous bilateral extracapsular PFF of a male patient is presented.
An 85-year-old male patient who was hit by a car as a pedestrian presented at our emergency department. The patient has a medical history of chronic obstructive pulmonary disease and compensated chronic cardiomyopathy. He lives with his son and could independently perform daily activities. On examination, external rotation and shortened lower limbs on both sides were evident, as well as pain in palpation and/or mobilization of the lower extremities bilaterally. Following the radiological study, a transtrochanteric fracture of the right femur and a subtrochanteric fracture of the left femur were revealed (Fig. 1).

Figure 1: Anteroposterior view of the pelvis. Right intertrochanteric fracture. Left subtrochanteric fracture.
The computed tomography trauma series revealed vertebral osteoporotic fractures of TH12, L1, and L3, which are not related to the acute trauma. He was given adequate painkillers, immobilized with a coxo-femoral cast bilaterally, and was admitted to the intensive care unit. After a short pre-operative preparation, he underwent operative treatment for both fractures on the day of admission, which was performed under general anesthesia. The patient was placed on a radiolucent traction table, and the right transtrochanteric fracture was first fixated with closed reduction and a non-reamed intramedullary short nail. After open reduction, the left subtrochanteric fracture was fixated with a non-reamed long nail with distal static locking screws. Fluoroscopic image controls were acceptable, and there were no intraoperative complications. Postoperatively, patient recovery was without complications; the only problem was non-complicated anemia (67 g/L), solved with two units of blood. On the 1st post-operative day, radiographic control was done (Figs. 2 and 3).
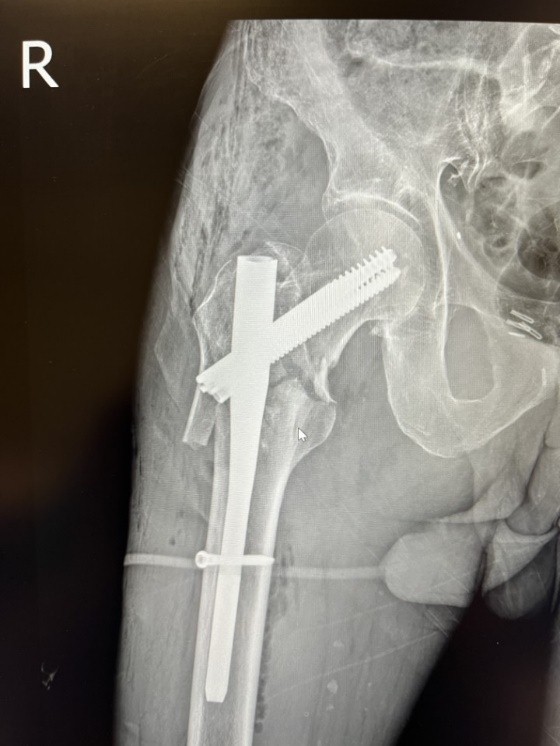
Figure 2: First post-operative day radiographic control of the right hip. Closed reduction and intramedullary fixation (InterTan 10×200).

Figure 3: First post-operative day radiographic control of the left hip. Open reduction and intramedullary fixation (InterTan 10×400).
The patient was mobilized from the beginning with the help of our physiotherapists. The patient was discharged on the 7th post-operative day. Outpatient follow-up is satisfying. No surgical wound problems or infections were identified. At 6 weeks from surgery, radiographic evaluation was done (Fig. 4), and the patient was ambulatory with the help of crutches.
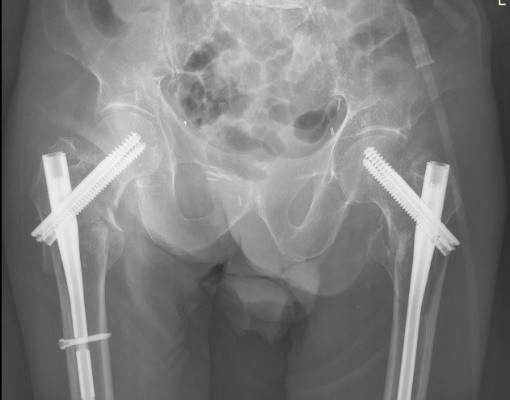
Figure 4: Six weeks post-operative X-ray.
Anti-osteoporotic drug treatment was implemented, and a healthy diet with protein intake, calcium, and Vitamin D supplementation was encouraged.
Following the 3-month examination, the patient showed consolidation on radiographic control (Fig. 5).
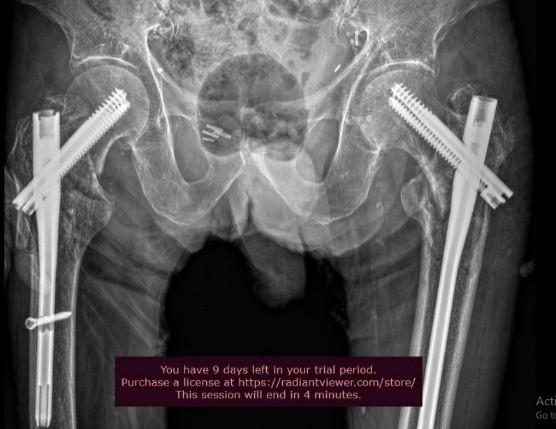
Figure 5: Twelve weeks post-operative X-ray.
He was ambulatory without crutches, had no pain complaints, and no limping was evident.
Hip fractures in the elderly are quite frequent and result in a high morbimortality rate [3,4]. The functional impairment leads to considerable social as well as economic implications due to the inability of the patients to perform their daily activities [5,6]. The morbidity of unilateral hip fractures ranges from 40 to 50% in women and from 13 to 22% in men [7], which is quite a high incidence. Contrary to this, simultaneous bilateral PFFs are not that common; therefore, there is a lack of data in the literature regarding the management of these injuries. According to Grisoni et al., over the period of 10 years, only eight cases were reported, with a frequency of 0.3% of the total number of hip fractures [8]. Furthermore, Verma et al. over the period of 3 years presented only four cases of simultaneous bilateral PFF with a rate of 0.24% [9]. Because of the low incidence of these types of injuries, there is no established, reliable treatment protocol yet, making these patients unique and demanding in the treatment process. Rodriguez-Zamorano has reviewed and analyzed the corresponding literature related to simultaneous bilateral PFF, and they have identified three patient profiles: “(i) Young patients involved in a traffic accident with multiple associated injuries, for which the definitive surgical intervention was sometimes delayed, having an impact on the overall survival. (ii) Patients aged 65–75 years old with fractures in the context of high-energy accidents. (iii) Patients over 80 years who sustain fragility fractures after casual falls from their height”[1]. An interesting fact that must be emphasized here is that our case does not fit into any of the above-mentioned patient profiles because the patient is above 85 years old and has sustained a high-energy trauma. In this course of events, this case would make an independent “fourth” profile of patients with simultaneous bilateral PFF. There are different approaches regarding the surgical treatment of simultaneous bilateral extracapsular hip fractures. We decided on proceeding with intramedullary fixation bilaterally since it offers better results compared to extramedullary fixation – shorter intraoperative time, smaller surgical wound, lower infection rate, less blood loss, and earlier weight bearing. There is an ongoing debate about whether to ream the intramedullary canal. While reaming allows usage of a thicker implant – thus biomechanically more stable fixation, on the other hand, it increases intraoperative time and the risk of fat embolism syndrome, especially in patients with bilateral proximal fractures. Furthermore, adult respiratory distress syndrome is considered significantly higher in bilateral fractures [10]. In our case, we decided not to use reaming in either of the fractures. Closed reduction and percutaneous K-wires were used for the fixation of the right intertrochanteric fracture (Fig. 6), whereas open reduction and percutaneous K-wires were used for the fixation of the left subtrochanteric fractures since closed reduction was unsatisfying (Fig. 7).
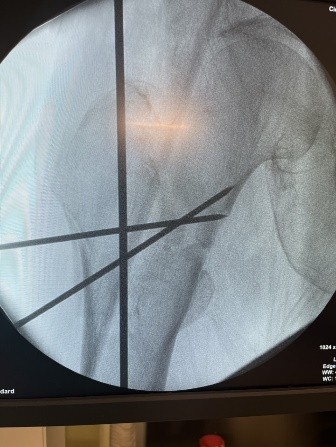
Figure 6: Right hip. Closed reduction and percutaneous K-wires.
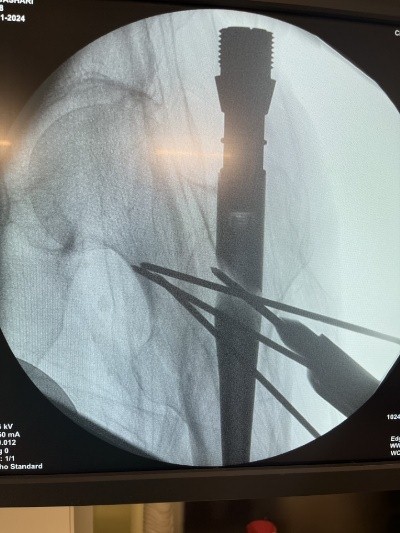
Figure 7: Left hip. Open reduction and K-wires.
The average length of hospitalization in our hospital for patients with unilateral hip fractures is 4–5 days, whereas this patient was discharged on the 7th post-operative day. At 6 weeks, the patient was ambulatory with crutches, and at 3 months from the operation, the patient was full weight-bearing with no major complaints and with signs of consolidation in the radiographic control.
Simultaneous bilateral PFF is a very rare but life-threatening injury, with a serious impact on the quality of the patient’s life. A very small number of cases have been reported in the literature, making these cases very difficult to manage, especially the subgroup of elderly patients with high-energy trauma, in which cases the morbimortality rate is very high. In these patients, three steps are of paramount importance: A thorough pre-operative preparation, prompt stabilization of the fractures, and early mobilization. Having these postulates in mind, we aim for a successful treatment of these rare and complicated cases.
Even though there are limited data due to the rarity of these injuries, in patients with bilateral extracapsular proximal femoral fractures (PFF), early fixation and mobilization usually lead to favorable outcomes despite the complexity of the injury.
References
- 1. Rodríguez-Zamorano P, Galán-Olleros M, Garcia-Coiradas J, Llanos S, Valle-Cruz JA, Marco F. Simultaneous bilateral extracapsular proximal femur fractures in the elderly. A case report. J Surg Case Rep 2022;2022:rjac313. [Google Scholar]
- 2. Aydın E, Dülgeroğlu TC, Metineren H. Bilateral simultaneous intertrochanteric fractures of femur without major trauma. Int Med Case Rep J 2015;8:137-9. [Google Scholar]
- 3. Panula J, Pihlajamäki H, Mattila VM, Jaatinen P, Vahlberg T, Aarnio P, et al. Mortality and cause of death in hip fracture patients aged 65 or older: A population-based study. BMC Musculoskelet Disord 2011;12:105. [Google Scholar]
- 4. Robbins JA, Buzkova P, Barzilay JI, Cauley JA, Fink HA, Carbone LD, et al. Mortality following hip fracture in older adults with and without coronary heart disease. Am J Med 2023;136:789-95.e2. [Google Scholar]
- 5. Auais M, Al-Zoubi F, Matheson A, Brown K, Magaziner J, French SD. Understanding the role of social factors in recovery after hip fractures: A structured scoping review. Health Soc Care Community 2019;27:1375-87. [Google Scholar]
- 6. Selaković I, Mandić-Rajčević S, Milovanović A, Tomanović-Vujadinović S, Dimitrijević S, Aleksić M, et al. Pre-fracture functional status and early functional recovery are significant predictors of instrumental activities of daily living after hip fracture: A prospective cohort study. GeriatrOrthop Surg Rehabil 2024;15:Online ahead of print. doi: 10.1177/21514593241255627. [Google Scholar]
- 7. Galán-Olleros M, Rodríguez-Zamorano P, García-Coiradas J, Llanos S, Mora-Fernández J, Valle-Cruz JA, et al. Literature review on the management of simultaneous bilateral extracapsular hip fractures in the elderly. Current Orthopaedic Practice 2022;33:186-96. [Google Scholar]
- 8. Grisoni N, Foulk D, Sprott D, Laughlin RT. Simultaneous bilateral hip fractures in a level I trauma center. J Trauma 2008;65:132-5. [Google Scholar]
- 9. Verma V, Kundu ZS, Batra A, Singh R, Sangwan SS, Gupta P. Simultaneous bilateral trochanteric fractures-a report of four cases. Chin J Traumatol 2012;15:360-3. [Google Scholar]
- 10. O’Toole RV, Lindbloom BJ, Hui E, Fiastro A, Boateng H, O’Brien M, et al. Are bilateral femoral fractures no longer a marker for death? J Orthop Trauma 2014;28:77-81. [Google Scholar]