Traditionally, total elbow arthroplasty involves resection of the humeral condyles; however, in this case report, the condyles were preserved and sutured to the prosthesis to achieve improved anatomical replication.
Dr. Ankush Mohabey, Department of Orthopaedics, All India Institute of Medical Sciences, Nagpur, Maharashtra, India. E-mail: ankushmohabey@aiimsnagpur.edu.in
Introduction: Total elbow arthroplasty (TEA) is a valuable salvage procedure, traditionally reserved for elderly or rheumatoid patients. However, expanding indications have allowed selective application in younger patients with debilitating post-traumatic elbow pathology.
Case Report: A 74-year-old female presented with persistent instability and ulnar neuropathy following non-union of a distal humerus fracture and chronically dislocated elbow, complicated by progressive arthropathy. On evaluation, she exhibited valgus-varus laxity, restricted range of motion (ROM), and crepitus. A semi-constrained TEA was performed using a posterior triceps-splitting approach. The humeral condyles, though destabilised from prior instrumentation, were preserved and secured using No. 5 Ethibond sutures. These sutures were tied to the humeral prosthesis. Postoperatively, by 3 months the patient achieved a functional, pain-free elbow with improved ROM and resolution of neurological symptoms.
Conclusion: This case highlights the potential of condylar-preserving TEA as a reliable management option in advanced post-traumatic elbow dysfunction. Even in the presence of instability, non-union and prior instrumentation, preserving the native condyles and securing them to the prosthesis can yield a stable, pain-free, functional result.
Keywords: Total elbow arthroplasty, Ethibond sutures, anatomical reconstruction, condylar preservation.
Distal humerus fractures, particularly those involving articular surfaces, can result in chronic elbow dysfunction if not treated effectively. In younger patients, internal fixation is generally favored to maintain native anatomy and permit functional recovery. However, complications such as non-union, post-traumatic arthropathy, and chronic elbow instability may necessitate salvage options. Total elbow arthroplasty (TEA), once primarily indicated for rheumatoid or osteoarthritic pathology, has emerged as a valuable solution in such cases [1,2]. Despite improvements in implant design and surgical technique, the application of TEA in younger patients (<50 years) remains controversial due to the risk of implant failure and limitations in post-operative loading [1,3]. Nevertheless, literature increasingly supports its use in select post-traumatic cases where reconstruction is unfeasible, especially when pain and loss of motion severely impact quality of life [4,5].
A 74-year-old female presented with complaints of persistent pain, restricted motion, and paraesthesia in the left elbow. She had sustained a closed distal humerus fracture 1 year prior, managed with open reduction and internal fixation using cancellous compression screws at an outside institution. The fixation failed, leading to non-union of the elbow joint. Following implant removal 3 months prior, the patient reported worsening symptoms, including instability, deformity, and neurological symptoms in the ulnar distribution.
- Clinical examination shows that the medial side of the elbow prominence has with loss of 3-point bony alignment
- Tenderness over the medial and lateral joint lines
- Painful crepitus on motion
- ROM limited to 20–90° with terminal pain
- Valgus and varus laxity confirmed
- Ulnar nerve: Paraesthesia over the little finger, motor function preserved.
Investigations:
- Radiographs: Non-union of the distal humerus, joint space narrowing, articular irregularity, and subluxation (Fig. 1)

Figure 1: Pre-operative radiograph.
- CT scan: Misaligned fragments, condylar attenuation, cartilage loss
Surgical management:
- Rationale for TEA: Given the chronic nature of the instability, non-union, and degenerative changes, reconstructive fixation was not viable. The patient was counseled on the benefits and limitations of TEA, including permanent lifting restrictions and prosthesis longevity.
Surgical tips and tricks
Under general and regional anesthesia, a posterior midline incision was used. A triceps-sparing approach provided access to the joint [6]. Dense fibrous tissue and synovitis were debrided. The ulnar nerve was isolated and protected. Intraoperatively, the condyles were found intact but with compromised cortical support. Instead of resection, both condyles were preserved and secured with multiple tensioned loops of no. 5 Ethibond suture, restoring the supracondylar architecture and facilitating prosthesis fit. The medullary canals were broached, and an uncemented, hinged prosthesis was implanted. Trialling confirmed joint stability and good arc of motion (0–110°). The triceps was repaired with heavy non-absorbable sutures. (Fig. 2 and 3) (Table 1).

Figure 2: Implantation of prosthesis.

Figure 3: Reconstruction and anatomical replication.
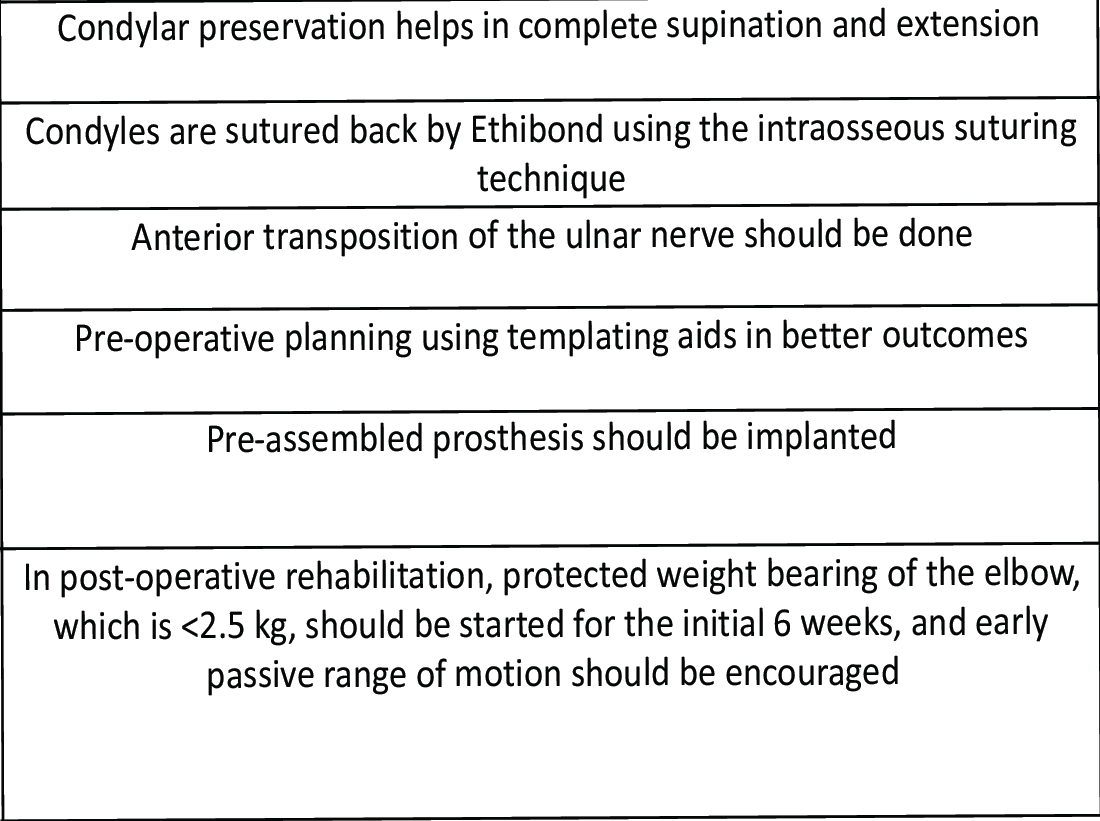
Table 1: Key pointers for surgical management.
Post-operative protocol
Immobilization with a posterior slab was done for 14 days. Passive ROM initiated at day 14 under physiotherapy supervision. Active-assisted ROM at 4 weeks. Muscle strengthening was continued thereafter. Lifelong precautions on lifting weights and fall prevention were followed. Clinical examination at 6 weeks shows that the surgical scar was well-healed. There was a loss of 3-point bony alignment as compared to the opposite side. There was tenderness over the medial and lateral joint lines. Rom was 20–90°, disabilities of the arm, shoulder, and hand (DASH) score of 40, and there was no valgus or varus laxity. Ulnar nerve paraesthesia over the little finger was present, for which nerve conduction velocity was done, which revealed ulnar neuropathy; motor functions were preserved. At 6 months follow-up, ulnar neuropathy was resolved, and she has 10–110° of ROM with full supination and pronation with a DASH score of 20. There was no tenderness over the scar and joint line. Power was 4/5 in both wrist flexion and extension at the end of 6 months. Whereas follow-up and outcome at 1 year was ROM 10–120°. (Fig. 4,5)

Figure 4: Range of motion clinical post-operative.

Figure 5: Range of motion clinical post-operative.
Pain-free with complete resolution of paraesthesia with DASH score, which improved from 65 (pre-operative) to 15.3 (at the end of 1 year). Radiographs at 6 weeks, 6 months, and 1 year revealed no aseptic loosening of the elbow prosthesis along with non-displacement of both the condyles. (Figure 6,7,8)

Figure 6: Post-operative radiograph.

Figure 7: Post-operative radiograph.
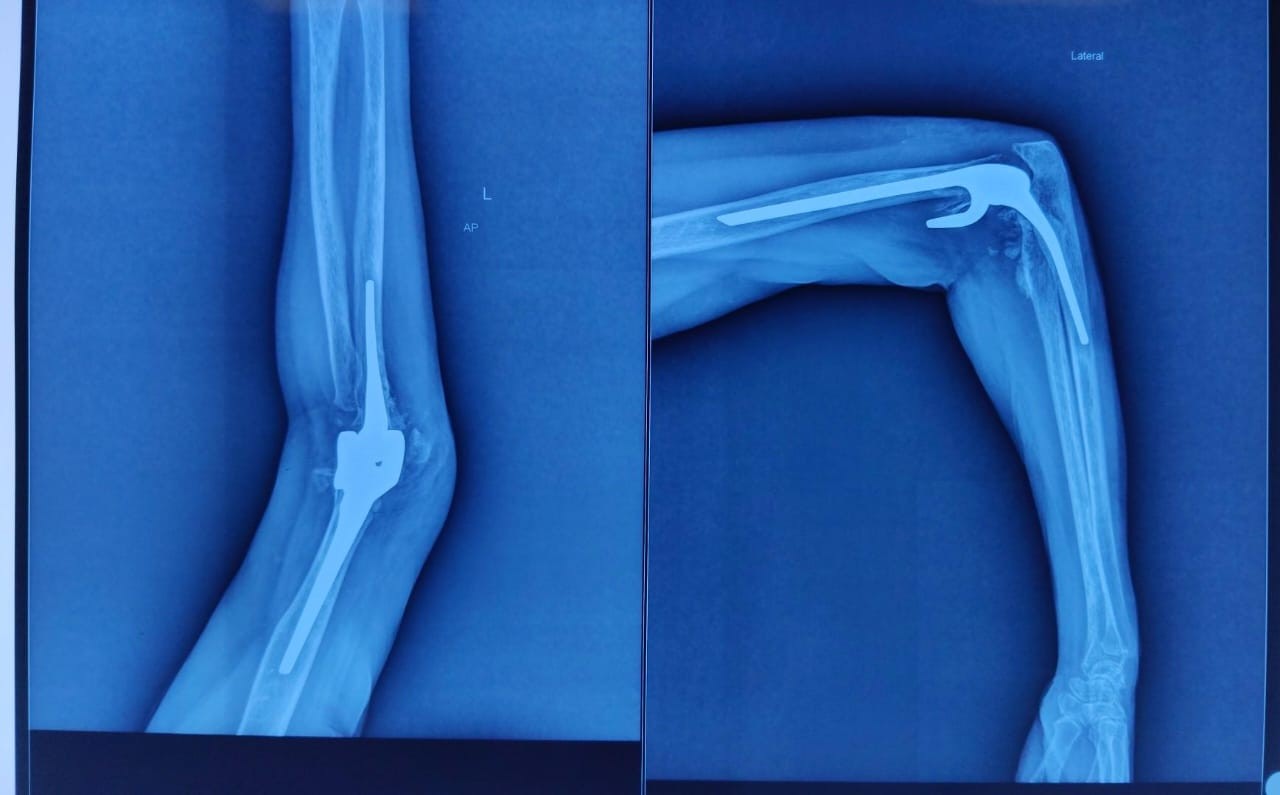
Figure 8: Follow-up radiograph.
The management of complex elbow injuries remains a surgical challenge when primary internal fixation fails. The risk of long-term disability due to chronic pain, stiffness, deformity, and instability is significant. In the present case, the presence of non-union and chronic elbow misalignment led to progressive arthropathy, which rendered the joint irreparable by conventional means. In such scenarios, TEA provides an alternative pathway to restore function and reduce pain [7]. TEA was historically limited to elderly patients with inflammatory arthropathies due to concerns about mechanical wear and activity restrictions. However, advancements in prosthetic design, cementing techniques, and soft-tissue handling have broadened its use. Coonrad–Morrey-type semi-constrained implants, such as the one used in this case, offer a balance between joint mobility and stability, particularly valuable in elbows with ligamentous incompetence [3]. Several authors have demonstrated the successful application of TEA in young, low-demand individuals when reconstruction is not feasible. Savio et al. [1] described a similar case of TEA in a 38-year-old patient with schizophrenia and a neglected terrible triad, resulting in significant post-traumatic changes. Their study emphasized the role of TEA in providing pain relief and restoring the functional range of motion when traditional methods were contraindicated. Similarly, Prasetia et al. [4] highlighted the importance of soft-tissue management during TEA in neglected non-union and arthropathy. They used a triceps turn-down flap for adequate lengthening and tissue coverage, allowing for improved post-operative outcomes. While our case did not require such augmentation, the meticulous handling of triceps and preservation of humeral condyles helped avoid soft-tissue compromise. The concept of condylar preservation in TEA has been less frequently reported but offers several potential benefits. It aids in maintaining the natural shape of the distal humerus, improves implant seating, and provides additional cortical support. In our case, cerclage with no. 5 Ethibond sutures allowed secure stabilization of the condylar fragments, recreating an anatomic scaffold for the prosthesis. This strategy avoids the need for extensive distal bone resection, a critical consideration in younger patients who may outlive their initial implant. D’Ambrosi et al. [5] reported similar success with TEA in a patient with complete post-traumatic elbow ankylosis. Their outcomes mirrored our findings: significant improvement in range of motion, pain scores, and daily activity performance. Furthermore, Cutler et al. [3] demonstrated the feasibility of converting elbow arthrodesis to TEA, which underscores the procedure’s value as a motion-restoring solution in severely compromised elbows. It is essential, however, to recognize the limitations and potential complications of TEA. These include implant loosening, infection, bushing wear, and periprosthetic fractures, particularly with increased mechanical demands [8,9]. Hence, patient selection remains crucial, and pre-operative counseling about lifelong restrictions is vital to ensure implant longevity. This case exemplifies the integration of anatomical preservation, stable prosthetic implantation, and soft-tissue balance, leading to excellent early outcomes in a challenging post-traumatic elbow. Continued follow-up will be essential to monitor long-term performance, but early indicators suggest that condylar-preserving TEA can be a robust solution in appropriately selected young patients. [10]
TEA with condylar preservation and soft-tissue reconstruction offers a promising solution for managing severe post-traumatic elbow dysfunction, including non-union and arthropathy, in select patients. With appropriate surgical planning and patient compliance, TEA can restore function, alleviate pain, and improve quality of life despite age-based constraints.
Condylar preservation and soft-tissue reconstruction in total elbow arthroplasty present a viable approach for managing complex post-traumatic elbow conditions such as non-union and arthropathy in appropriately selected patients. This case highlights the successful combination of anatomical preservation, secure prosthetic fixation, and restoration of soft-tissue balance, resulting in excellent short-term outcomes. Ongoing follow-up will be crucial to evaluate long-term success.
References
- 1. Savio SD, Artha K, Wiguna I. Total elbow arthroplasty as the treatment of choice for a young man with neglected terrible triad of the elbow joint and schizophrenia: A case report. Malays Orthop J 2024;18:66-70. [Google Scholar] [PubMed]
- 2. Sivakumar R, Somashekar V, Shingi PK, Chidambaram M. Total elbow arthroplasty as treatment of non-union with bone loss of distal humerus-A case report. J Orthop Case Rep 2020;10:63-5. [Google Scholar] [PubMed]
- 3. Cutler HS, Heineman N, Hurd A, Koehler D, Bass R, Schacherer T. Conversion of elbow arthrodesis to total elbow arthroplasty: A case report and literature review. J Shoulder Elb Arthroplast 2022;6:1-7. [Google Scholar] [PubMed]
- 4. Prasetia R, Purwana SZ, Hidajat NN, Rasyid HN. Total elbow arthroplasty with tricep turn-down flap in an old unreduced elbow dislocation: A case report. Int J Surg Case Rep 2023;108:108432. [Google Scholar] [PubMed]
- 5. D’Ambrosi R, Formiconi F, Ursino N, Rubino M. Treatment of complete ankylosed elbow with total arthroplasty. BMJ Case Rep 2019;12:e231123. [Google Scholar] [PubMed]
- 6. Bryan RS, Morrey BF. Extensive posterior exposure of the elbow. A triceps-sparing approach. Clin Orthop Relat Res 1982;166:188-92. [Google Scholar] [PubMed]
- 7. Celli A, Paroni C, Bonucci P, Celli L. Total elbow arthroplasty for acute distal humeral fractures with humeral condyle resection or retention: A long-term follow-up study. JSES Int 2021;5:797-803. [Google Scholar] [PubMed]
- 8. Chafik D, Lee TQ, Gupta R. Total elbow arthroplasty: Current indications, factors affecting outcomes, and follow-up results. Am J Orthop (Belle Mead NJ) 2004;33:496-503. [Google Scholar] [PubMed]
- 9. Kholinne E, Arya A, Jeon IH. Complications of modern design total elbow replacement. J Clin Orthop Trauma 2021;19:42-9. [Google Scholar] [PubMed]
- 10. Macken AA, Prkic A, Kodde IF, Lans J, Chen NC, Eygendaal D. Global trends in indications for total elbow arthroplasty: A systematic review of national registries. EFORT Open Rev 2020;5:215-20. [Google Scholar] [PubMed]