Arthroscopic intra-articular decompression of spinoglenoid cysts combined with labral repair effectively addresses both the source and the consequence of suprascapular nerve compression.
Dr. Sandesh Manohar, Division of Sports Injury, Department of Joint Preservation and Regenerative Medicine, St John’s National Academy of Health Sciences, Bengaluru, Karnataka, India. E-mail: sandeshmanohar@yahoo.com
Introduction: A spinoglenoid cyst is a ganglion cyst that compresses the suprascapular nerve in the spinoglenoid notch. On failure of the conservative treatment, surgical decompression is the treatment of choice. The arthroscopic method helps to decompress the cyst intra-articularly through the labral tear and also allows repair of the labral tear. This study aims to bring out the functional outcome of arthroscopic Spinoglenoid Cyst Decompression with labral repair.
Materials and Methods: This study is a case series of eight symptomatic Spinoglenoid cysts with labral tears which were treated with arthroscopic cyst decompression and labral repair over 5 years from January 2018 to December 2023. The American Shoulder and Elbow Surgeon’s score (ASES), Constant Murley (CM) score, and Visual Analog Score (VAS) were used to assess the patients preoperatively and postoperatively at regular intervals.
Results: All the patients had good to excellent results. There was a significant improvement in the ASES from a mean pre-operative 61.5 to a mean 1-year follow-up of 90.3, while the CM score improved from a mean pre-operative 66.8% to a mean 1-year follow-up of 93.4%. The VAS decreased from a mean pre-operative 6.3 to a mean 1-year follow-up of one.
Conclusion: Spinoglenoid Cyst is usually seen in individuals and athletes who are involved in an overhead activity. Arthroscopic decompression of the cyst and labral repair is a simple and effective treatment and gives excellent functional outcomes.
Keywords: Spinoglenoid cyst, labral repair, suprascapular nerve, superior labrum anteroposterior tear.
There is a strong association between spinoglenoid cysts (SGC) with labral tears [1,2,3]. The tears act as a one-way valve, causing the accumulation of the synovial fluid, leading to the formation of cysts [1,2,3]. SGC can compress the Suprascapular nerve (SSN) in the suprascapular notch or in the spinoglenoid notch according to its size. The former can cause weakness of infraspinatus (IST), while the latter can cause weakness of both supraspinatus (SST) and IST. A few cases of involvement of teres minor (TM) have also been reported [2]. The possible explanation could be the variance in the innervation of the TM muscle by a branch of SSN or a cyst located at the posteroinferior part of the glenoid compressing the posterior branch of the axillary nerve or by a large SGC that expands downwards to compress the nerve to TM.
Arthroscopic sub-labral cyst decompression and labral repair is a simple and effective method of treating SGC with good clinical outcomes [2,4]. It has been found that the recurrence rate of SGC is high when decompression alone is done without labral repair; indicating that there is a strong association of the cyst with intra-articular labral disease [5,6,7]. It is due to the ball-valve mechanism by which fluid from the joint escapes through the labral defect to form a cyst and cannot come back into the joint. Similarly, arthroscopic labral repair without cyst decompression has been associated with poor outcomes; this might be due to the prolonged time required for the resolution of the cyst, resulting in persistent nerve compression and pain [3,8].
This is a case series of eight cases of SGC that presented to our Outpatient over a period of 2 years. All patients were evaluated with a detailed history and clinical examination. Their main complaint was dull aching posterior and deep shoulder pain, which increases with overhead activity. In some patients, there was night pain, and they were not able to lie on the same side. All the patients had weakness of shoulder external rotation due to IST weakness (Fig. 1),

Figure 1: Demonstration of external rotation weakness.
while one patient has weakness of abduction due to an associated SST weakness. One patient also had atrophy of the IST muscle (Fig. 2).

Figure 2: (a) Lateral view and (b) View from behind showing Infraspinatus muscle atrophy.
Standard shoulder radiographs (Anteroposterior, Axillary, and scapular Y views) were normal in all the patients. Magnetic resonance imaging (MRI) was done for all the patients, which confirmed the diagnosis of SGC and labral tear (Fig. 3).
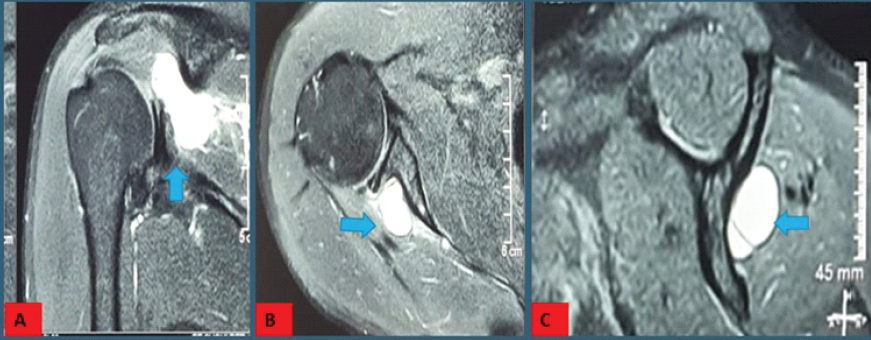
Figure 3: Magnetic resonance imaging of the shoulder (a) coronal (b) axial (c) sagittal views showing spinoglenoid cysts.
Electromyography (EMG) and nerve conduction study (NCS) studies in our patients were inconclusive. All the patients were managed conservatively initially with 3 months of physiotherapy. On failure of the conservative treatment, they underwent arthroscopic sublabral cyst decompression and labral repair. The American Shoulder and Elbow Surgeon’s score (ASES), Constant Murley score (CM), and Visual Analog Score (VAS) were used to assess the patient preoperatively and postoperatively at regular intervals of 3, 6, and 12 months and then yearly.
Arthroscopic technique
All the patients were given general anesthesia and interscalene block, the patient was positioned in the lateral decubitus position with the arm in 30° abduction, 20° of forward flexion, and with 3–4 kg of lateral traction. We prefer a lateral position as it creates a reference point by positioning the glenoid parallel to the floor and helps in easier visualization and better access to the superior and posterior parts of the shoulder joint. Adequate soft-tissue padding under all the pressure points, especially the opposite axilla and knee should be given. Three standard portals were used -posterior, anterior, and trans-tendon. The posterior portal was made in a soft spot between the IST and the TM muscle about 2 cm inferior and 1–2 cm medial to the angle of the acromion. The trans-tendon portal and the anterior portal were made by the outside-in technique using a spinal needle. If needed, additional portals can be made depending on the labral tear pattern. In all the surgeries, the posterior portal was used as a viewing portal, and the anterior portal as a working portal (Fig. 4).
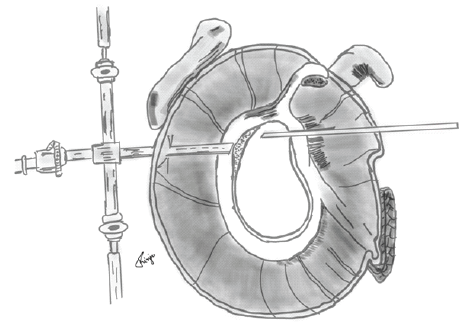
Figure 4: Illustration showing labral tear with 30° arthroscope in posterior viewing portal and probe in the anterior portal.
Suture anchor placement and knot tying were done through the trans-tendon portal. Initially, diagnostic arthroscopy of the joint would be done thoroughly via both portals. Inspection of the labrum was done circumferentially starting anterior to the biceps. Labral tears were usually present as a Type II Superior labrum antero-posterior (SLAP) tear, but in three cases, it was a posterosuperior labral tear extending posteriorly to the biceps anchor, and also the cyst bulge was visible intra-articularly in two cases (Fig. 5) [9].
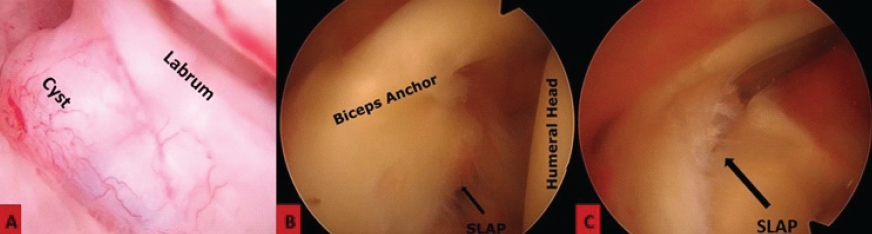
Figure 5: Arthroscopic (a) image of the spinoglenoid cyst (b) image of the Superior labrum anteroposterior tear, (c) image showing probing of the tear.
Viewing through the posterior portal, decompression of the cyst was done sublabrally beneath the tear gently using an arthroscopic probe or tissue rasp introduced through the anterior portal (Fig. 6).
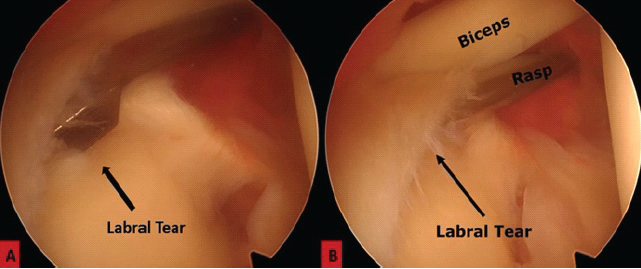
Figure 6: (a and b) Arthroscopic images showing decompression of the labral cyst using an arthroscopic rasp by passing it sublabrally.
An egress of yellowish-tinged gelatinous fluid through the tear indicates a successful decompression. Occasionally, the egressed fluid will be blood-tinged. Care must be taken not to go too deep in the cyst, as the SSN will be present 2 cm medial to the glenoid rim. The footprint of the labral tear should be properly debrided, and the underlying cartilage removed using a soft-tissue shaver to expose the bleeding bone to promote healing. Through the trans tendon portal, the labral tear was repaired using 2 or 3 1.5 mm single-loaded all-suture anchors (Fiberknot-Biotek, Ahmedabad, Gujarat) (Fig. 7). Wounds were closed with no. 2.0 non-absorbable sutures.
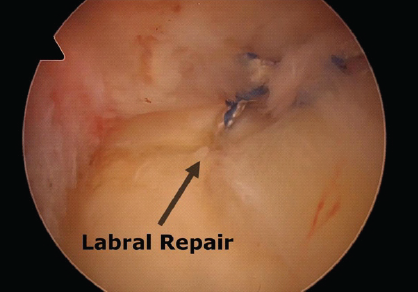
Figure 7: Arthroscopic image showing repaired labral tear using suture anchors.
Standard Rehabilitation protocol was followed for all the patients. All the patients were put on a shoulder immobilizer for the first 3 weeks. Initially, a passive shoulder range of motion was initiated in the 1st post-operative week, followed by active-assisted and active exercises starting from the 3rd post-operative week onwards, except for the use of biceps, which can be initiated after 6 weeks. On achieving a full active range of motion, strengthening exercises were initiated by around 8–10 weeks post-operative, which were continued till 6 months. Overhead lifting of weights and return to sports were allowed after 6 months.
Out of the eight patients, there were seven males and one female. Mean age of the study group was 22 years. Two patients were athletes who were participating in the overhead sports activity, while another was an electrician who frequently carried out the overhead activity. Three patients had a history of fall, while two patients had a history of Road traffic accidents. Out of the eight, six were dominant hands. All the patients had good to excellent results. Out of the eight patients, seven patients had significant pain relief on the 1st post-operative day. At 3 months of follow-up, the patients had no rest pain or night pain, and the power of the muscles improved significantly by 6 months. There was a significant improvement in the ASES from a mean pre-operative 61.5 to a mean 1-year follow-up of 90.3, while the CM score improved from a mean pre-operative 66.8% to a mean 1-year follow-up of 93.4%. The VAS decreased from a mean pre-operative 6.3 to a mean 1-year follow-up of one (Table 1).
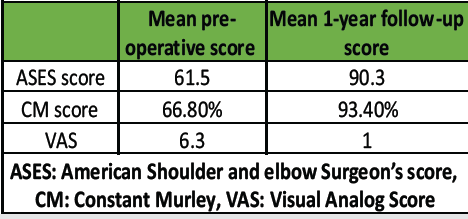
Table 1: Results
In our case series, there was no recurrence of the cysts in any patients. The mean follow-up duration was around 34 months, with a maximum follow-up of 62 months and a minimum follow-up of 14 months.
The SSN arises from the fifth and sixth cervical nerve, which is a part of the upper trunk of the brachial plexus. It is a mixed nerve that innervates the SST and the IST muscles and gives sensory supply to the glenohumeral and the acromioclavicular joint. The nerve traverses deep and parallel to the inferior belly of the omohyoid in the posterior triangle of the neck and then passes beneath the trapezius muscle. The nerve passes through the suprascapular notch to enter the supraspinous fossa, passing beneath the superior transverse scapular ligament. It then passes deep to the SST and around the spinoglenoid notch under the inferior transverse scapular ligament to enter the infraspinous fossa (Fig. 8).
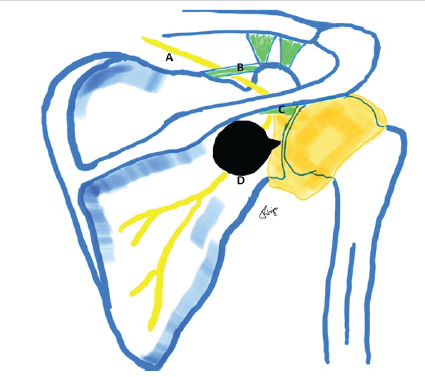
Figure 8: Diagram showing the course of the suprascapular nerve and the potential sites of compression (a) – suprascapular nerve (b) – superior transverse scapular ligament, (c) – Inferior transverse scapular ligament, and (d) – spinoglenoid cyst.
At the spinoglenoid notch, the nerve lies very close to the glenohumeral joint, almost 1.8–2.1 cm from the glenoid rim. The inferior branch of SSN divides into three or four branches to supply the IST in the region of the spinoglenoid notch. SSN entrapment, as a cause of chronic shoulder pain, has been overlooked most of the time. The different causes of entrapment include impingement on the superior and inferior transverse scapular ligament, fracture of the scapula, shoulder dislocation, humeral fractures, tumors, and ganglion cysts.
The patient usually presents to the orthopedic surgeon with a history of shoulder injury in the past, and the usual mechanism is longitudinal traction consistent with that of the SLAP tear. Often, the diagnosis is difficult and delayed due to vague complaints. The main symptom is poorly localized deep posterolateral shoulder pain both in patients with and without atrophy [1]. The reason for this could be due to the compression of the sensory branch of the SSN, which innervates the posterior part of the capsule. The pain gets exaggerated while doing overhead activities and lifting heavy weights, and is relieved by taking rest. Sleep could be disturbed, and patients will be unable to lie on the same side. Usually, there will be no discrete area of tenderness on examination. The patient’s symptoms might mimic a rotator cuff tear, with symptoms of weakness; primarily of external rotation and abduction. There might be associated atrophy of the muscles mainly IST, but rarely also of SST and TM. Other differentials to be considered include cervical disc disease, tendinitis, adhesive capsulitis, and glenohumeral or acromioclavicular arthritis.
Diagnosis is clinched usually with clinical findings, MRI, EMG, and NCS. MRI allows for confirming the presence, location, and size of the cyst. However, it also helps in the detection of associated pathology, such as a labral tear, muscle atrophy, degenerative changes, and rotator cuff tear. The size of the cyst is important as it influences nerve compression and muscle atrophy. It has been reported that cysts >3.1 cm in diameter were associated with signs of muscle denervation [2]. EMG and NCS may show isolated fibrillation potential and denervation of the IST muscle, and in some people of both SST and IST.
SGC has been managed over the years, ranging from conservative treatment to a variety of surgical options. Conservative treatment includes rest, anti-inflammatory drugs, restriction of repetitive overhead shoulder movement, and physiotherapy focusing on strengthening posterior rotator cuff muscles. There could be a spontaneous resolution of the cyst in extremely rare cases [1,4]; however, there can be an expansion of the cyst as well. Expanding cyst can cause denudation of the posterior portion of the glenoid neck. Needle aspiration under ultrasound or computer tomography guidance is a good option; however, there is a risk of incomplete decompression and a high chance of recurrence. Open excision is highly invasive and requires extensive dissection of the deltoid muscle. Other treatment options include arthroscopic decompression of the cyst with or without labral repair, labral repair alone without cyst decompression, or decompression through the subacromial space when the cyst is extending superiorly [8]. Decompression of the cyst can be done directly or indirectly. In our technique, the cyst is decompressed indirectly through the labral tear, after which the labral repair is done with suture anchors.
Arthroscopic decompression can be done either sublabrally or through a subacromial approach. The subacromial approach is used when the SGC is extending superiorly or for suprascapular cysts [10]. However, this technique requires aggressive bursectomy and soft-tissue dissection to identify the raphe between the SST and IST and the structures around the notch. It has the risk of damaging the SSN and the coracoclavicular ligament. Furthermore, sub acromial approach needs additional portals for tackling the associated labral tear.
Arthroscopic intra-articular method helps to address the root cause of the problem and also helps to identify other intra-articular pathologies like rotator cuff tears. Decompression can be done either indirectly through the labral defect or directly through a superior capsular window adjacent to the junction of the capsule and labrum [1,5,7,10]. Decompression through capsular window has the risk of creating a large defect in the superior capsule and the formation of a large hematoma; however, it has the advantage of decompression by directly visualizing the cyst.
Indirect sub-labral decompression can be done using a rosette knife or bluntly using a shaver or a probe [6]. In our technique, we have decompressed the cyst using an arthroscopic tissue rasp. The SSN lies very close to the glenoid rim, almost within 2 cm, hence there is a risk of injuring the nerve through the indirect technique. It can also lead to incomplete decompression of the cyst, and there is a risk of converting the tear into a large and unstable one. However, sublabral approach has the advantage of decompressing the cyst without damaging the surrounding tissue (Table 2).
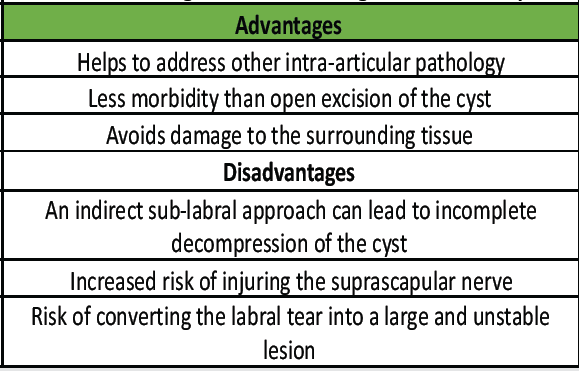
Table 2: Advantages and disadvantages of our technique
The diagnosis of a spinoglenoid cyst is usually difficult and delayed due to its vague complaints. It is usually seen in individuals and sports persons involved in the overhead activity. If left untreated, it can result in persistent shoulder pain progressing to muscle weakness and atrophy. Arthroscopic intra-articular decompression of the spinoglenoid cyst and labral repair gives patients excellent results in the form of pain relief and regaining of the full range of movement and power. It allows athletes to return to their sport within 6 months.
Early recognition of spinoglenoid cysts associated with labral tears is essential in patients presenting with unexplained posterior shoulder pain and weakness. Arthroscopic cyst decompression combined with labral repair provides a minimally invasive, safe, and effective solution that relieves nerve compression, prevents recurrence, and yields excellent functional recovery.
References
- 1. Moore TP, Fritts HM, Quick DC, Buss DD. Suprascapular nerve entrapment caused by supraglenoid cyst compression. J Shoulder Elbow Surg 1997;6:455-62. [Google Scholar] [PubMed]
- 2. Tung GA, Entzian D, Stern JB, Green A. MR imaging and MR arthrography of paraglenoid labral cysts. AJR Am J Roentgenol 2000;174:1707-15. [Google Scholar] [PubMed]
- 3. Youm T, Matthews PV, El Attrache NS. Treatment of patients with spinoglenoid cysts associated with superior labral tears without cyst aspiration, debridement, or excision. Arthroscopy 2006;22:548-52. [Google Scholar] [PubMed]
- 4. Piatt BE, Hawkins RJ, Fritz RC, Ho CP, Wolf E, Schickendantz M. Clinical evaluation and treatment of spinoglenoid notch ganglion cysts. J Shoulder Elbow Surg 2002;11:600-4. [Google Scholar] [PubMed]
- 5. Hashiguchi H, Iwashita S, Ohkubo A, Takai S. SLAP repair with arthroscopic decompression of spinoglenoid cyst. SICOT J 2016;22:1. [Google Scholar] [PubMed]
- 6. Iannotti JP, Ramsey ML. Arthroscopic decompression of a ganglion cyst causing suprascapular nerve compression. Arthroscopy 1996;12:739-45. [Google Scholar] [PubMed]
- 7. Bhatia S, Chalmers PN, Yanke AB, Romeo AA, Verma NN. Arthroscopic suprascapular nerve decompression: Transarticular and subacromial approach. Arthrosc Tech 2012;1:e187-92. [Google Scholar] [PubMed]
- 8. Schroder CP, Skare O, Stiris M, Gjengedal E, Uppheim G, Brox JI. Treatment of labral tears with associated spinoglenoid cysts without cyst decompression. J Bone Joint Surg Am 2008;90:523-30. [Google Scholar] [PubMed]
- 9. Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy 1990;6:274-9. [Google Scholar] [PubMed]
- 10. Ghodadra N, Nho SJ, Verma NN, Reiff S, Piasecki DP, Provencher MT, et al. Arthroscopic decompression of the suprascapular nerve at the spinoglenoid notch and suprascapular notch through the subacromial space. Arthroscopy 2009;25:439-45. [Google Scholar] [PubMed]











