Fibula fixation in extra-articular distal third tibial fractures is to be considered in selected cases, keeping in mind the future prognosis of tibial fracture healing.
Dr. Sundar Suriyakumar, Department of Orthopaedic surgery, Sri Ramachandra institute of higher education and research, Plot No.1372, F1 Sharon Shelters, I Block, 28th Street, Kambar Colony, 18th Main Road, Anna Nagar West, Chennai-40, India. E-mail: drssundhar@gmail.com
Introduction: Fractures involving the distal third of both bone leg are one of the common long bone fractures with significant concern owing to the amount of soft-tissue damage incurred and poor prognosis with respect to fracture fixation.
Aim: The aim of the study is to evaluate whether fibula fixation is necessary along with internal fixation of extra-articular distal tibia fractures by comparing the clinico-radiological and functional outcome of patients of extra-articular distal third tibia fractures with fibula “fixed” and fibula “not fixed” group.
Materials and Methods: A prospective cohort study with a sample size of 30 patients was conducted in Sri Ramachandra Institute of Higher Education and Research between March 2023 and May 2024. Fibula fixation was done in one group, and the fibula was not fixed in the control group. Research methodology includes radiological evaluation for coronal and sagittal plane malalignment, Radiographic Union Score for Tibial fractures (RUST) scoring, and clinically, rotational malalignment and presence of post-operative infection. All cases were followed up for a minimum duration of 6 months to assess union of tibia fractures in both groups.
Results: Tibial bone union rate was better in the fibula not fixed (control) group compared to the fibula fixed group (P = 0.032), confirmed by the RUST scoring (P = 0.047), which was statistically significant.
Conclusion: There was no significant improvement with additional fibula fixation in the healing of distal tibia fractures, but rather causes greater morbidity in terms of wound infections and delayed healing of the tibia. This clearly demonstrates that fibula fixation in extra-articular distal tibia fractures when the fracture does not affect the syndesmosis or ankle mortise is not necessary, and is associated with a higher risk of tibial non-union.
Keywords: Distal tibia, fibula, fracture, fixation, osteosynthesis.
Fractures involving the distal third tibia are common long bone fractures with an increasing incidence of road traffic accident (RTA) worldwide. It is also one of the most feared fractures because of the increased soft-tissue complications and worse prognosis in terms of fracture fixation. Distal tibia fractures with or without fibula fractures may present as tibial pilon injuries, extra-articular distal one-third tibia fractures, or exclusively ankle injuries [1]. Various options of fibula osteosynthesis have been described for ankle and tibial pilon fractures, but there is no proven literature about when to fix the fibula in extra-articular distal tibia fractures [1].
Distal tibial metaphyseal fractures due to high velocity trauma (axial compressive forces or direct bending as in RTA or fall from height) are commonly seen in adolescent and adult age group especially between 35 and 40 years of age (men>women), whereas the low velocity trauma (rotational forces such as sports-related injuries or simply a twisting ankle injury) occurs in old aged associated with osteoporosis (women>men) [1]. However, overall incidence is more in young adult males compared to any other group. Distal tibial fractures constitute 37.8% of all tibial fractures [1]. Distal tibial metaphyseal (extra-articular) fractures constitute <7% of all tibial fractures, 15% of all fractures of the distal third tibia [2,3,4], <10% of all lower extremity fractures [5].
The aim was to evaluate whether fixation of the fibula is necessary along with internal fixation of extra-articular distal tibia fractures by comparing the clinicoradiological and functional outcome of patients of extra-articular distal third tibia fractures with fibula “fixed” and fibula “not fixed” group.
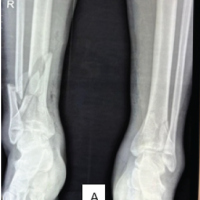
A prospective cohort study was conducted at Sri Ramachandra Institute of Higher Education and Research, Chennai, with 30 patients. Sample size was calculated based on the average census of the above mentioned fracture in a speculated duration reported in a particular healthcare center and it was approved by the Institutional Ethics Committee of Sri Ramachandra University and the thesis guide – between March 2023 and May 2024 for 15 months with minimum follow-up of 6 months to analyze the outcomes of extra-articular distal one tibia fractures with fibula fractures treated with internal fixation of tibia and fibula or internal fixation of the tibia alone. It included patients with age >18 years with extra-articular distal one-third tibia metaphyseal fractures (AO Type 43A) distal to the level of tibial isthmus with concomitant suprasyndesmotic distal fibula fractures (Weber Type C). The study included only patients with closed or open Grade I fractures distal to level of isthmus (Fig. 1).
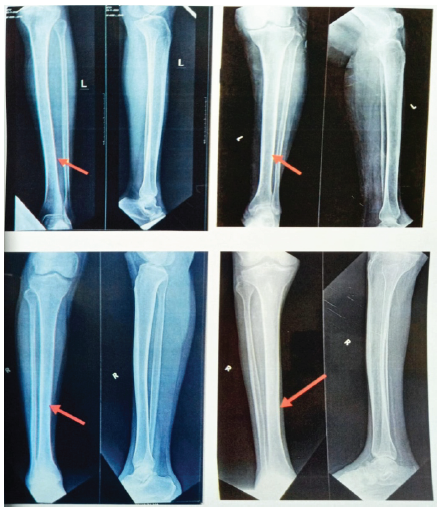 Figure 1: Examples of X-rays showing tibial isthmus (Isthmus is arbitrarily located at middle 1/3rd-distal 1/3rd junction of tibia at the narrowest portion of medullary canal. Isthmus is not located at a fixed point but varies from one individual to other).
Figure 1: Examples of X-rays showing tibial isthmus (Isthmus is arbitrarily located at middle 1/3rd-distal 1/3rd junction of tibia at the narrowest portion of medullary canal. Isthmus is not located at a fixed point but varies from one individual to other).
The study excluded patients with isolated fibula fractures, both bone leg shaft fractures, i.e., tibial shaft fractures with fibula fractures proximal to tibial isthmus (AO type 42), intra-articular tibial pilon fractures (AO Type 43B and 43C), distal fibula fractures with syndesmotic injury (Weber Type A and B), ankle fractures and Gustilo–Anderson open Grade II and Grade III fractures.
We have included 17 patients in Group A, i.e., fibula fixed with either plating (14 patients) or Titanium Elastic Nail System (TENS) nailing (3 patients), and 13 patients in Group B, i.e.,
Fibula not fixed group with 20 male and 10 female patients. Fibula was decided to be fixed in cases wherein distal tibial plating was done, as cyclic compression theory works better only in cases wherein tibial nailing was done without fibula fixation. However, fibula fixation was decided intraoperatively based on the tibial fracture reduction, tibial axis alignment, tibia or fibula fracture comminution and amount of soft tissue cover. The main purpose of the study is to decide whether which pattern of tibia fracture and type of tibia fixation would require additional fibula fixation without compromising on the overall tibial fracture healing both clinically and radiologically. Fibula, if decided to be fixed, was considered for plating (using a precontoured distal fibula plate, one-third tubular plate, or reconstruction plate), which confers better rotational stability and axial alignment than TENS nailing,
which is minimally invasive and is done in cases with severe soft-tissue damage and also to reduce soft tissue and vascular compromise in closed fractures. These factors considered were purely patient- specific and individual surgeon’s preference and expertise. Differences in outcomes between fibula plating and TENS nailing were not separately studied and are beyond the scope of our discussion.
I) Radiological
First, coronal plane malalignment was studied during the immediate and 6th month post-operative period (last follow-up) by measuring Lateral Distal Tibial Angle (LDTA) (Normal LDTA = 89° (86°–92°) and the inference was to rule out varus/valgus >5° change. Then sagittal plane malalignment during the immediate and 6th month post- operative period by measuring Anterior Distal Tibial Angle (ADTA) (Normal ADTA = 80° (78°–82°) and inference was to rule out procurvatum/recurvatum >10° change. Radiographic Union Score for Tibial fractures (RUST) scoring was used to assess fracture healing status and to find any delay in healing (delayed union/non- union) based on callus formation and presence of fracture line
(RUST score = sum of all four cortex scores with a total score of 4–12).
*Note: Using AP and lateral radiographs, the radiographic evidence of healing on at least three cortices was used to determine fracture union. The absence of radiographic signs of bone union and pain at the fracture site during weight-bearing after the 6th month following surgery were considered as indicator of non-union. Fig. 2 describes the overview of the RUST score [6]. Fig. 3 describes RUST score in three phases of consolidation [7].
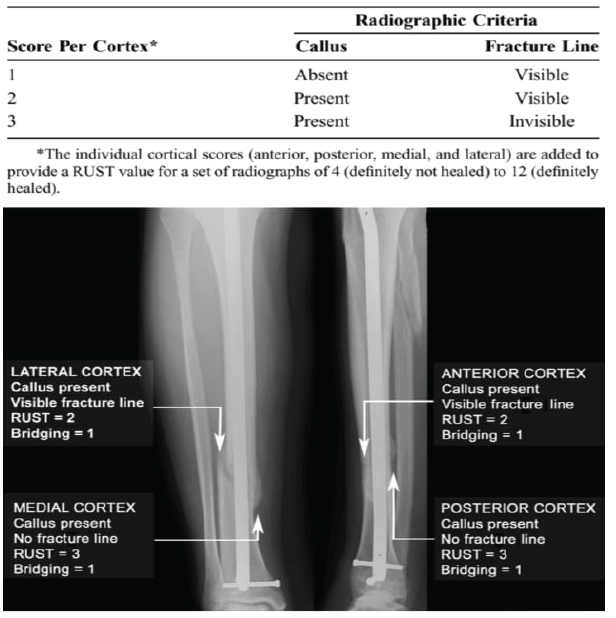 Figure 2: Overview of the radiographic union score for tibial fractures score [6].
Figure 2: Overview of the radiographic union score for tibial fractures score [6].
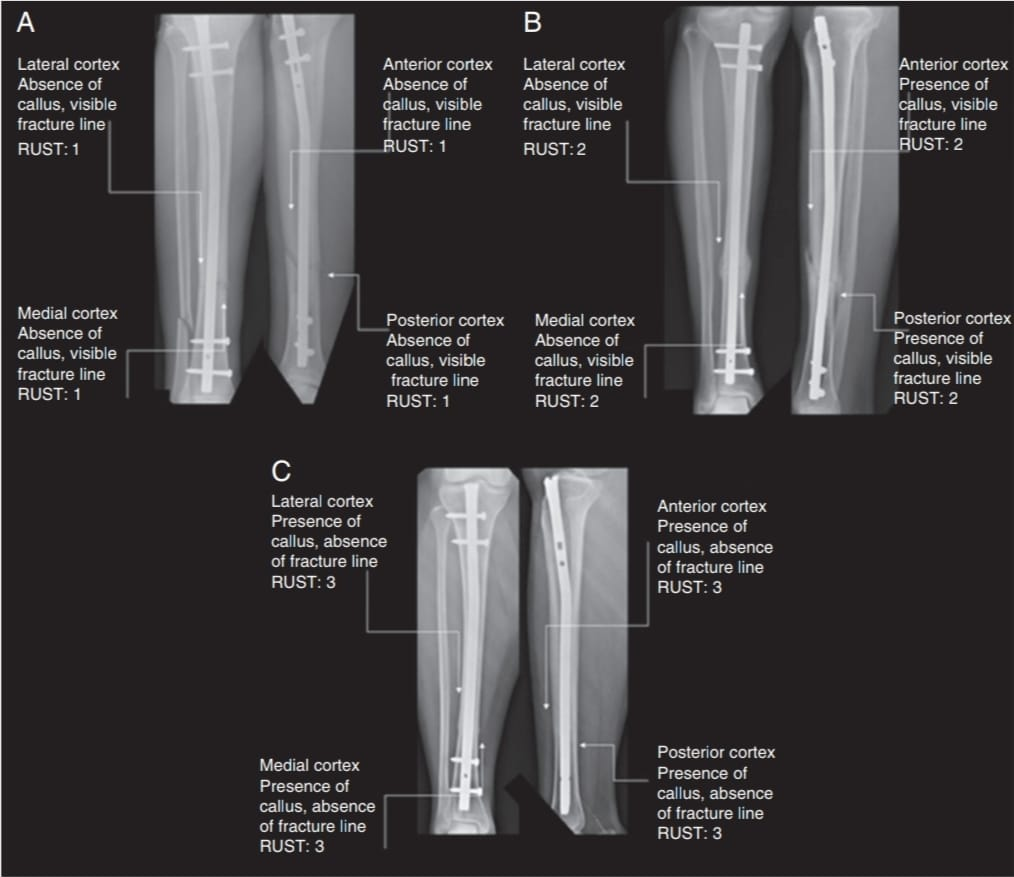 Figure 3: Radiographic union score for tibial fractures score in three phases of consolidation [7] (A=4, B=8, C=12).
Figure 3: Radiographic union score for tibial fractures score in three phases of consolidation [7] (A=4, B=8, C=12).
ii) Clinical
It includes rotational malalignment by assessing for post- operative tibial torsion (Tibia varum/valgum) by measuring the thigh-foot angle (Normal: 0–20° External rotation) with > 10° of internal rotation being indicative of tibial torsion and post-operative complications such as infection that might delay fracture/wound healing.
The data were entered into MS Excel (Windows) and further analyzed using SPSS software (version 20; SPSS Inc., Chicago IL, USA). For descriptive analysis, the categorical variables were analyzed using frequency and percentages; the continuous variables were analyzed by calculating mean ± standard deviation. For inferential analysis, the continuous (ordinal) data were analyzed using Independent “t” test/ Mann–Whitney test, and the categorical data were analyzed using Chi-square test and “P < 0.05” will be considered as statistically significant. The mean age of the participants in the fibula fixed group was 45 years, whereas it was 37 years in the fibula not fixed group. The tibial bone union was clinically better in the fibula not fixed group (100%) when compared with the fibula fixed group (70.6% of cases), i.e.,12 out of 17 patients. Thus, the study was found to have statistically significant association between the tibia union and fibula fixation (P = 0.032*) (Fig. 4). RUST score whose mean was 9.47 in fibula fixed and 10.92 among fibula not fixed group showed significant difference between the two groups (P = 0.047*) based on the results of non-parametric Mann–Whitney test (Fig. 5). (Among 29% of fibula fixed cases with tibial non union, (i.e., 5 cases), the fixation implant for tibia used was plate in 4 cases and IM nail in 1 case). The coronal and sagittal plane alignment were maintained within normal range in both groups and occurrence of post-operative infection was similar in both groups and they were statistically insignificant. Tibial torsion was typically absent in all patients, hence was constant. Table 1 shows the summary of the study results of 30 patients.
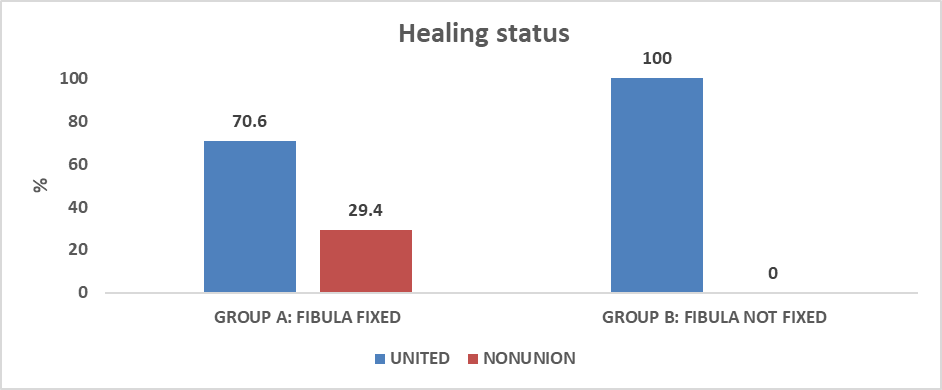 Figure 4: Illustrates union and non-union of fracture among cases and controls.
Figure 4: Illustrates union and non-union of fracture among cases and controls.
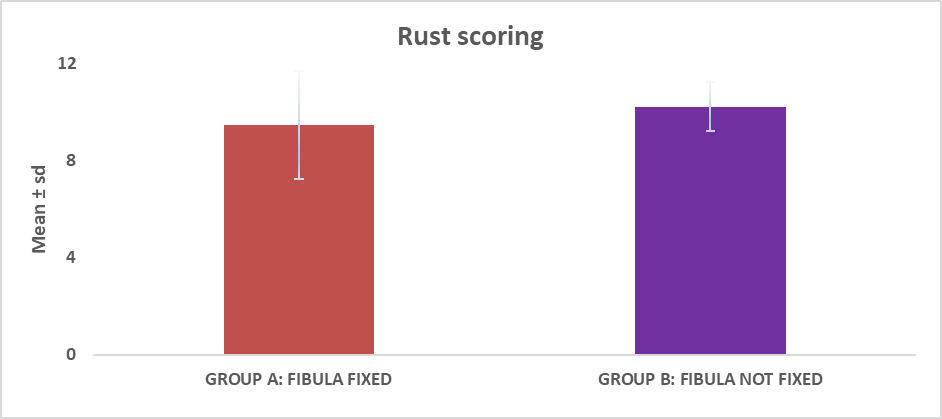 Figure 5: Comparison of radiographic union score for tibial fractures scoring between Group A and Group B.
Figure 5: Comparison of radiographic union score for tibial fractures scoring between Group A and Group B.
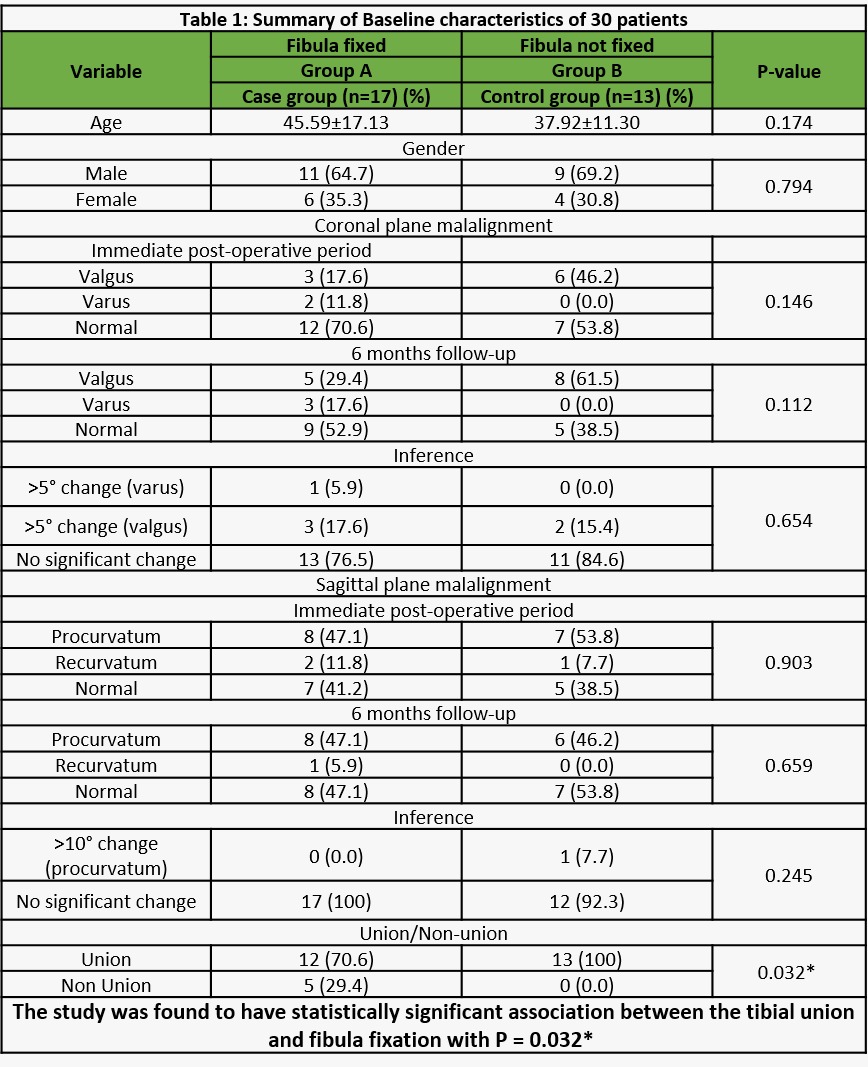
Table 1: Summary of Baseline characteristics of 30 patients
Clinical and biomechanical implications of fibula fixation
It is still a matter of debate if fibular fixation is really necessary for distal third both bone leg fractures. There is disagreement regarding the role of fibula fixation in extra-articular fractures of distal tibial metaphysis, but most agree that those fibula fractures associated with syndesmotic or ankle mortise instability should be stabilized because malreduction of ankle mortise has been attributed to poor functional outcomes. The objectives for any fracture treatment are to restore the anatomical surfaces for articulation, gain adequate length, and ensure proper axial alignment and rotational stability. The fibula bears approximately 1/6th of the load applied to the knee [8], and these forces increase if associated with syndesmotic disruption [9,10,11]. From an anatomical point of view, it has been demonstrated that the fibula shears between 3% and 16% of the leg’s axial loads contributing significantly to lower leg weight-bearing and acts as a tension band (strut) against the medial bending forces on a fractured tibia, thus allowing earlier fracture healing [12]. Fibula along with the trochlear shaped talar dome enhances the biomechanical stability of ankle mortise during walking. It has also been demonstrated that the interosseous membrane serves as a conduit for stress transmission, enabling a load sharing function of fibula. In a holographic study of cadaveric limbs, complete sectioning of interosseous membrane has decreased the transmission of fibular load by 30% [9]. These results imply that in the event of interosseous membrane disruption, the tibia will bear majority of the weight bearing stress.
Anatomical rigid fixation of fibula is beneficial as a supplement to stability, improves the quality of tibial reduction, provides more reliable tibial bone union, and hence fibula fixation was suggested. Tibio-fibular length disparity caused by intact fibula changed tibio-fibular strain patterns, and hence the anatomic fixation of fibula or the intrinsic biomechanics of intact fibula would raise the incidence of non- union. It was also elucidated that the effects of fibular sparing on distal tibial fracture resulted in rapid union of the fracture because it promotes cyclic compression at tibial fracture site [13]. A mechanical testing conducted with fractured human legs found that fibula osteotomy increased motion at the tibial defect when less rigid fixation was used to fix tibia (with intramedullary [IM] nail), and stabilization of fibula improved stability. When the tibia fracture was treated with a bridging plate and the fibula was left untreated, there was a greater tendency for non-union of fibular fracture at the same level as tibial fracture hence fibular osteosynthesis promotes stability and enhances fracture recovery. Tibial healing was unaffected when the fibula fracture occurred at a different level. The current study thus demonstrated that fibula fixation does not significantly affect the healing of tibia fracture if both fractures are not at the same level or if the tibial fixation device is a nail [14].
Previously well proven indicators of fibular fixation include fractures close to the tibial plafond, fractures of tibia and fibula
at the same level and significant fibular comminution [15]. It is also important to maintain distal tibial alignment if planned for tibial IM nailing as malalignment is very common due to narrow IM nail diameter and wider distal tibial metaphyseal medullary canal. Placing a fibular plate before tibia nailing can help in preserving alignment and length for distal tibia fractures with concomitant fibula fractures. This is especially helpful for very distal tibial and simple fibular fracture patterns. It is important to reduce the fibula carefully because improper fibula reduction will impede precise tibial reduction. After fibular plating is done, it will keep the tibia out to length laterally, but it usually will not prevent the varus collapse, hence care should be made to ensure the tibia is not malaligned in varus [1].
Disadvantages of adjunctive fibular fixation in distal tibial fractures. There is no added advantage of fibula fixation in distal tibial fractures without syndesmotic injury or extra-articular tibial pilon fractures with incorrect/open reduction and fixation of fibula increasing chances of late tibial malunion, fibular non-union and soft-tissue complications, hence not recommended [16] latter especially with high-energy injuries. Hence, managing these fractures require a minimally invasive approach.
In recent literature, a multi-centric case series showed a negative impact of fibula plating on tibial fractures treated with an IM nailing, citing an 8-fold increased risk of delayed union. In cadaveric studies, there was no increase in stability with fibular fixation using traditional bi-planar locking screw fixation after using multidirectional locking screws for IM nailing of distal tibia fractures. Ultimately concluding that fibular fixation is not necessary when tibia is fixed with multidirectional locking screws [17]. Fibula and tibia fractures should be considered as a single biomechanical and pathological factor, and the value of double surgical osteosynthesis was confirmed as an added advantage to increase stability and to facilitate tibial reduction, i.e., the tibial axes were statistically better corrected when fibula was fixed [18].
Thus in my study, the tibial fracture union was better in the fibula not fixed group (100%) when compared with fibula fixed group (70.6%) which is according to Teitz et al. [13] wherein he proved that distal tibia union will be better if distal fibula is not fixed as an intact or fixed fibula will inhibit the cyclical loading at tibial fracture site thus leading to delayed union or non-union. Distal tibial metaphyseal fracture with an intact fibula might also require a partial fibulectomy or fibular osteotomy to accentuate tibial fracture healing in tibia fracture non-union management as per DeLee et al. [19]. Furthermore, fibula fracture reduction and fixation might cause additional soft tissue damage further delaying distal tibial fracture healing as shown by Varsalona and Lui [16] as it is a well-known fact that there is poor blood supply at the middle third-distal third junction of tibia (“water-shed zone in tibia”). Fibula plating has thus been proven to increase initial rotational stability by decreasing the axial rotation in cases wherein concurrent IM nailing of tibia is done thus reducing risk of valgus malunion as per the cadaveric studies by Kumar et al. [20] and it is very much proven clinically in our study but it is not statistically significant. The tibial alignment is also better corrected in both coronal and sagittal plane if both tibia and fibula are fixed as explained by Bonnevialle et al. [15]. Vallier et al. [18] concise in their study all of the above proven concepts that fibula fixation if not done leads to significant rates of malunion as fibula fixation aids tibial fracture reduction at the time of surgery but at the same time has chances of tibial non-union also. Hence, this shows that risk–benefit factors should be assessed by comparing and contrasting whether fibula fixation is really needed or not which is patient specific and moreover surgeon’s preference.
Some of the limitations of the study include small sample size, absence of randomization, different surgeons involved in operation, malrotation was only assessed clinically without computed tomography scan, mechanism of injury, order of fracture fixation, anatomical location of fibula fractures (whether at same level/proximal/distal to tibial fracture), type of extra-articular distal tibial fractures (43A1/A2/A3) and intraoperative assessment of tibio-fibular stability were not considered, medical comorbidities such as diabetes, CAD and alcoholism/smoking were neither considered nor any BMD measurements performed which might influence healing standards.
We did not observe any significant improvement using fibular fixation in the treatment outcomes of distal tibia fractures. The addition of fibula fixation does not affect whether or not alignment is maintained during the short-term (6-month) follow-up period or the immediate post-operative period. Therefore, my research has clearly demonstrated that fibular fixation in extra -articular distal tibia fractures when the fracture does not affect the syndesmosis or the ankle mortise is not necessary, and that it is associated with a higher risk of tibia non- union. The additional trauma of fibular internal fixation may rather cause greater morbidity in terms of wound infections and delayed healing of tibia. Despite the different modes of biomechanics and healing potential and post-operative rehab protocol with tibia plating and tibia IM nailing, adhering to the general principles as discussed above, fibula fixation is mandated only if tibial fracture reduction is not satisfactory or there is difficulty in attaining adequate alignment with adequate soft tissue cover.
Over-zealous approach in fixing fibula is to be avoided and to be considered only in cases herein there is an absolute indication to maintain tibial length, alignment and stability promoting favorable tibial fracture healing. (According to the existing concepts and the above results, the absolute indications for fibula fixation are distal fibula fracture with associated syndesmotic injury with adequate soft tissue cover and in cases wherein there is difficulty in maintaining tibial axis alignment intraoperatively post tibial fracture fixation).
References
- 1. Bucholz R. Rockwood and Green’s Fractures in Adults. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. [Google Scholar] [PubMed]
- 2. Bourne RB, Rorabeck CH, Macnab J. Intra-articular fractures of the distal tibia: The pilon fracture. J Trauma 1983;23:591-6. [Google Scholar] [PubMed]
- 3. Ovadia DN, Beals RK. Fractures of the tibial plafond. J Bone Joint Surg Am 1986;68:543-51. [Google Scholar] [PubMed]
- 4. Tyllianakis M, Megas P, Giannikas D, Lambiris E. Interlocking intramedullary nailing in distal tibial fractures. Orthopedics 2000;23:805-8. [Google Scholar] [PubMed]
- 5. Marsh JL, Saltzman CL. Ankle fractures. In: Bucholz RW, Heckman JD, editors. Rockwood and Green’s Fractures in Adults. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. p. 2001-90. [Google Scholar] [PubMed]
- 6. Kooistra BW, Dijkman BG, Busse JW, Sprague S, Schemitsch EH, Bhandari M. The radiographic union scale in tibial fractures: Reliability and validity. J Orthop Trauma 2010;24 Suppl 1:S81-6. [Google Scholar] [PubMed]
- 7. Azevedo Filho FA, Cotias RB, Azi ML, de Almeida Teixeira AA. Reliability of the radiographic union scale in tibial fractures (RUST). Rev Bras Ortop 2016;52:35-9. [Google Scholar] [PubMed]
- 8. Lambert KL. The weight-bearing function of the fibula. A strain gauge study. J Bone Joint Surg Am 1971;53:507-13. [Google Scholar] [PubMed]
- 9. Vukicević S, Stern-Padovan R, Vukicević D, Keros P. Holographic investigations of the human tibiofibular interosseous membrane. Clin Orthop Relat Res 1980;151:210-4. [Google Scholar] [PubMed]
- 10. Skraba JS, Greenwald AS. The role of the interosseous membrane on tibiofibular weight-bearing. Foot Ankle 1984;4:301-4. [Google Scholar] [PubMed]
- 11. Strauss EJ, Alfonso D, Kummer FJ, Egol KA, Tejwani NC. The effect of concurrent fibular fracture on the fixation of distal tibia fractures: A laboratory comparison of intramedullary nails with locked plates. J Orthop Trauma 2007;21:172-7. [Google Scholar] [PubMed]
- 12. Pogliacomi F, Schiavi P, Calderazzi F, Ceccarelli F, Vaienti E. When is indicated fibular fixation in extra – articular fractures of the distal tibia? Acta Biomed 2019;89:558-63. [Google Scholar] [PubMed]
- 13. Teitz CC, Carter DR, Frankel VH. Problems associated with tibial fractures with intact fibulae. J Bone Joint Surg Am 1980;62:770-6. [Google Scholar] [PubMed]
- 14. Weber TG, Harrington RM, Henley MB, Tencer AF. The role of fibular fixation in combined fractures of the tibia and fibula: A biomechanical investigation. J Orthop Trauma 1997;11:206-11. [Google Scholar] [PubMed]
- 15. Bonnevialle P, Lafosse JM, Pidhorz L, Poichotte A, Asencio G, Dujardin F, et al. Distal leg fractures: How critical is the fibular fractures and its fixation? Orthop Traumatol Surg Res 2010;96:667-73. [Google Scholar] [PubMed]
- 16. Varsalona R, Liu GT. Distal tibial metaphyseal fractures: The role of fibular fixation. Strat Traum Limb Recon 2006;1:42-50. [Google Scholar] [PubMed]
- 17. Attal R, Maestri V, Doshi HK, Onder U, Smekal V, Blauth M, et al. The influence of distal locking on the need for fibular plating in intramedullary nailing of distal metaphyseal tibiofibular fractures. Bone Joint J 2014;96-B:385-9. [Google Scholar] [PubMed]
- 18. Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma 2011;25:736-41. [Google Scholar] [PubMed]
- 19. DeLee JC, Heckman JD, Lewis AG. Partial fibulectomy for ununited fractures of the tibia. J Bone Joint Surg Am 1981;63:1390-5. [Google Scholar] [PubMed]
- 20. Kumar A, Charlebois SJ, Lyle Cain E, Smith RA, Daniels AU, Crates JM. Effect of fibular plate fixation on rotational stability of simulated distal tibial fractures treated with intramedullary nailing. J Bone Joint Surg Am 2003;85:604-8. [Google Scholar] [PubMed]