Early recognition, surgical intervention, and specialized rehabilitation are pivotal in effectively managing bilateral spontaneous quadriceps tendon rupture with concurrent parathyroid adenoma, emphasizing the importance of a comprehensive approach for optimal patient outcomes.
Dr Maqbal Muhasin Nazar I.M., Senior Resident, Department of Orthopaedics, Govt. Medical College, Kozhikode, India.. E-mail: maqbal21@gmail.com
Introduction: Bilateral spontaneous quadriceps tendon rupture (QTR) is extremely rare. This condition involves the simultaneous tear of the fibrous tissue connecting the quadriceps muscle to the patella bone. The importance of prompt diagnosis is emphasized, as early recognition is crucial for initiating appropriate treatment and achieving optimal outcomes.
Case Report: This article presents a case report detailing the management of bilateral QTR alongside concomitant parathyroid adenoma in a 38-year-old male. The patient underwent open repair of both bilateral quadriceps tendons, followed by a well-planned physiotherapy protocol. Furthermore, surgical removal of the parathyroid adenoma was performed. A favourable functional outcome was observed during the 6-month follow-up period.
Conclusion: This case report highlights the critical aspects of managing bilateral spontaneous quadriceps rupture alongside concomitant parathyroid adenoma. Addressing the diagnostic and management challenges associated with this rare condition underscores the importance of early diagnosis, prompt surgical intervention, and tailored rehabilitation programs. This comprehensive approach contributes to the existing literature and emphasizes the significance of multidisciplinary collaboration in achieving favourable patient outcomes.
Keywords: Primary hyperparathyroidism, quadriceps rupture, adenoma, rehabilitation.
Quadriceps muscles are the principal extensors of the knee joint. The quadriceps femoris inserts into the patella through a shared tendon structured in three layers: The rectus femoris lies most superficially, followed by the vastus medialis and vastus lateralis in the intermediate layer, with the vastus intermedius deepest. Quadriceps tendon rupture (QTR) is a rare but debilitating condition characterized by the sudden rupture of the quadriceps tendon. While this injury is commonly attributed to direct trauma, a subset of cases presents spontaneously, without apparent cause.
Spontaneous quadriceps rupture was first described by Steiner and Palmer [1]. These spontaneous ruptures pose a diagnostic challenge and may signify an underlying systemic disorder. Only over 100 cases of spontaneous QTR have been reported worldwide. Spontaneous rupture can occur in degenerative tendons in patients affected by systemic conditions such as diabetes, rheumatoid arthritis, end-stage renal disease, hyperparathyroidism, autoimmune disease, gout, and long-term steroid use [2,3,4].
This case report aims to shed light on the rare but consequential association between spontaneous QTR and primary hyperparathyroidism. By presenting a detailed clinical case, we intend to underscore the importance of considering systemic factors in the evaluation and management of seemingly isolated musculoskeletal injuries. Through this exploration, we hope to enhance awareness among clinicians and researchers regarding the potential implications of primary hyperparathyroidism in the context of tendon pathology, ultimately facilitating early diagnosis and intervention.
A 38-year-old male presented to our outpatient department with complaints of right knee instability following a trivial fall. The patient had a history of left knee instability after a similar incident 5 months prior, which was diagnosed as QTR at another hospital. On examination, bilateral extensor lag was observed, along with a palpable defect in the quadriceps tendon on the left side. Left knee extension was restricted to 50°, whereas right knee extension was limited to 30° from the horizontal plane (Fig. 1).

Figure 1: Extension deficits of both knees.
Moderate hemarthrosis was present in both of his knees. X-ray findings revealed patella baja with calcification in the quadriceps tendon. Magnetic resonance imaging confirmed bilateral QTR near the patellar attachment on both sides (Fig. 2).
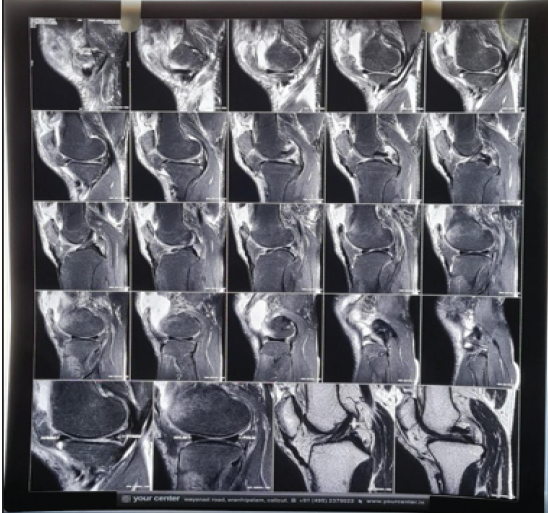
Figure 2: Magnetic resonance imaging films showing a complete tear of the patellar attachment of the quadriceps.
He was investigated for any underlying predisposing causes. (Table 1).
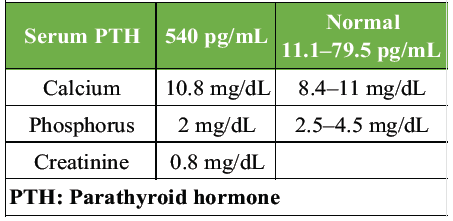
Table 1: Laboratory investigations showed the following values
Thyroid function tests, uric acid, and lipid profile were within normal limits. He was HLA B27 negative, and his body mass index was 27. Contrast-enhanced computed tomography of the abdomen revealed renal calculi measuring 2–4 mm in the right kidney. In addition, ultrasonography of the neck identified a well-defined hypoechoic lesion inferior to the thyroid gland on the left side, exhibiting internal vascularity suggestive of a parathyroid adenoma/hyperplasia.
Subsequently, parathyroid scintigraphy was performed, revealing focal tracer uptake in hypodense foci posterior and inferior to the lower pole of the left lobe of the thyroid gland, measuring 20 × 17 × 25 mm (Fig. 3).
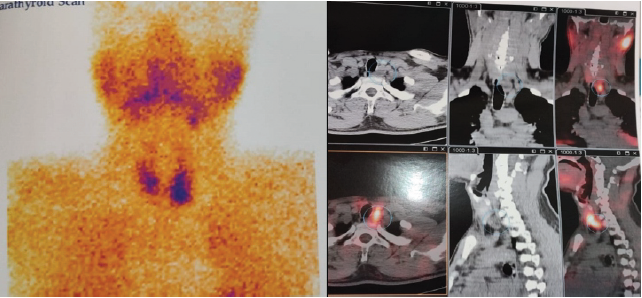
Figure 3: Parathyroid scintigraphy showing a hyperfunctioning parathyroid gland.
These findings were consistent with hyperfunctioning parathyroid adenoma involving the left inferior parathyroid gland, leading to the diagnosis of primary hyperparathyroidism. Both the endocrinologist and the head and neck surgeon consultations were done.
The head and neck surgeon recommended proceeding with parathyroid removal after the completion of quadriceps tendon repair surgery and once the patient’s condition permitted. The patient underwent surgical treatment for quadriceps tendon repair, utilizing a midline longitudinal incision. Both tendons showed a complete tear near the patellar attachment (Fig. 4).
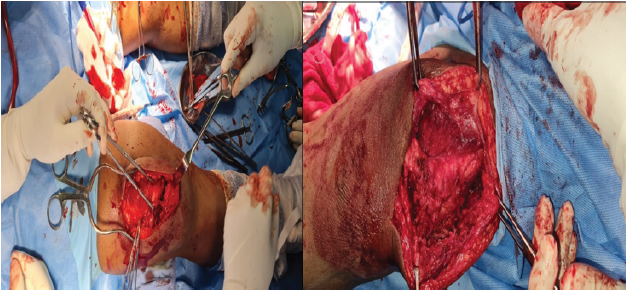
Figure 4: Intraoperative image showing both quadriceps tendon ruptures.
The tendon edges were freshened, and adequate tendon distality was confirmed. Subsequently, both ends of the tendon were sutured using No. 5 Ethibond sutures. To protect the repair, a stainless steel wire was passed through a transverse drill hole in the patella and the osseotendinous junction of the quadriceps tendon (Fig. 5). Following a 2-month recovery period, parathyroid excision was performed, along with hemithyroidectomy.
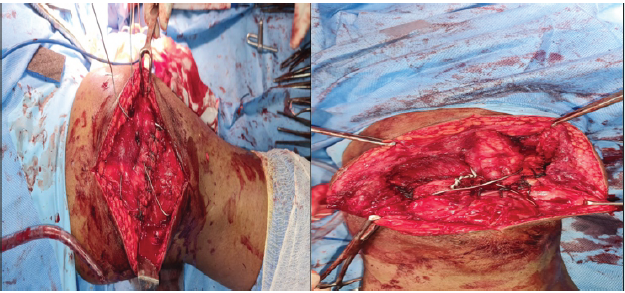
Figure 5: Intraoperative image after repair using Ethibond and strengthening with stainless steel wire.
In the post-operative period, the patient underwent a series of investigations to assess his progress. After 3 months, the serum levels of parathyroid hormone (PTH) were 13.4 pg/mL, serum calcium = 11.1 mg/dL, and serum phosphorus = 2 mg/dL. Post-operative X-ray revealed the patella with a normal Insall Salvati ratio and stainless steel wire in situ.
After a recovery period, the patient commenced a range of motion (ROM) exercises 6 weeks postoperatively. At the 6-month follow-up appointment, the patient exhibited full ROM without any extensor lag, indicating a successful surgical outcome (Fig. 6). There were no features of disease recurrence.

Figure 6: Full knee extension of both knees after 6 months of follow-up.
QTR is a serious and disabling injury that can occur as a result of a direct or, more commonly, an indirect mechanism. Bilateral QTRs can occur spontaneously or following minimal trauma. Most injuries occur during an eccentric contraction of the quadriceps against the body weight, when a significantly higher force is generated [5]. Spontaneous QTR in the background of primary hyperparathyroidism has been rarely reported; however, QTR occurring in patients with chronic renal failure, gout, SLE, obesity, and long-term steroid therapy is not rare. Diagnostic delay is quite common, especially in bilateral ruptures, as they can be mistaken for stroke, rheumatoid arthritis, disc prolapse, neuropathy, or even a psychiatric disorder [6]. Spontaneous QTR can be a clue to primary hyperparathyroidism, as in this case.
Primary hyperparathyroidism, characterized by excessive secretion of PTH from one or more parathyroid glands, is a known cause of musculoskeletal manifestations, including bone resorption and tendon calcification. Despite its association with bone pathology, the link between primary hyperparathyroidism and spontaneous QTR remains under-recognized and inadequately understood.
The effects of PTH on bone can be either catabolic or anabolic. The prevalence of one action will determine the net effect of PTH on bone mass and its microarchitecture. In co-culture experiments [7], osteoblasts are continuously exposed to PTH and sustain osteoclastogenesis, mimicking the effect of continuous exposure to high levels of PTH, as occurs in primary hyperparathyroidism patients. Under these conditions, PTH will lead to an increased osteoblast expression of the receptor activator of nuclear factor kappa-B ligand (RANKL). RANKL will bind to its receptor (RANK), which is expressed in osteoclast precursors, thereby stimulating osteoclastogenesis and osteoclast activity. In parallel, PTH induces a decrease in osteoprotegerin (OPG), a decoy receptor for RANKL, which prevents RANKL interaction with RANK. An increased RANKL/OPG ratio is thought to be the main mechanism by which a high level of PTH that elicits bone resorption is maintained [8].
In primary hyperparathyroidism, osteoblasts and osteoclasts are increased, but the resorption depth is overtaken, and the bone formation period is long. These ultrastructural events account for the increase in markers of bone turnover and changes in bone mineral density (BMD) [9]. Eventually, high levels of PTH lead to patellar subperiosteal bone resorption, thereby reducing the firmness of the quadriceps tendon, which attaches to the upper pole of the patella; these factors lead to complete disruption of the quadriceps tendon [10,11]. Another important factor of QTR occurrence is the sustained high level of PTH caused by a long-term and chronic injury to the quadriceps tendon due to toxins. These toxins cause negative feedback on tendon organization, leading to a reduction in protein–polysaccharide aggregate, enzyme secretion, maturity of actuated collagen fiber, and immaturity of quadriceps collagen [12,13]. These pathologic changes lead to significant tendon abnormalities, so that tendon mechanical stresses may be further damaged and exceed their tensile strength to the point of rupture. Therefore, a small trauma can lead to complete disruption of the quadriceps tendon, as in our case.
Managing spontaneous quadriceps rupture in a patient with hyperparathyroidism requires a multidisciplinary approach. Surgery is necessary to repair the rupture, along with removal of the adenoma, followed by careful post-operative monitoring of metabolic parameters such as serum PTH, calcium, and phosphorus levels.
Rehabilitation plays a crucial role in restoring quadriceps strength and function, with tailored exercise protocols implemented to facilitate recovery. Long-term follow-up is essential to monitor for recurrence or complications related to both the quadriceps rupture and hyperparathyroidism. Overall, successful management relies on coordinated care involving orthopedic surgeons, endocrinologists, and rehabilitation specialists to optimize outcomes and improve the patient’s quality of life.
The occurrence of spontaneous quadriceps rupture in patients with hyperparathyroidism underscores the importance of vigilance in both diagnosis and management. Clinicians should maintain a high index of suspicion for this complication, especially in patients with known hyperparathyroidism presenting with knee pain or sudden loss of function. Early recognition, prompt surgical intervention, and meticulous post-operative care are paramount for successful outcomes.
References
- 1. Steiner CA, Palmer LH. Simultaneous bilateral rupture of the quadriceps tendon. Am J Surg 1949;78:752-5. [Google Scholar] [PubMed]
- 2. Mousa A, Jones S, Toft A, Perros P. Spontaneous rupture of Achilles tendon: Missed presentation of Cushing’s syndrome. BMJ 1999;319:560-1. [Google Scholar] [PubMed]
- 3. De Ávila Fernandes E, Sandim GB, Mitraud SA, Kubota ES, Ferrari AJ, Fernandes AR. Sonographic description and classification of tendinous involvement in relation to tophi in chronic tophaceous gout. Insights Imaging 2010;1:143-8. [Google Scholar] [PubMed]
- 4. Alves EM, Macieira JC, Borba E, Chiuchetta FA, Santiago MB. Spontaneous tendon rupture in systemic lupus erythematosus: Association with Jaccoud’s arthropathy. Lupus 2010;19:247-54. [Google Scholar] [PubMed]
- 5. Ilan DI, Tejwani N, Keschner M, Leibman M. Quadriceps tendon rupture. J Am Acad Orthop Surg 2003;11:192-200. [Google Scholar] [PubMed]
- 6. Arumilli B, Adeyemo F, Samarji R. Bilateral simultaneous complete quadriceps rupture following chronic symptomatic tendinopathy: A case report. J Med Case Rep 2009;3:9031. [Google Scholar] [PubMed]
- 7. Huang JC, Sakata T, Pfleger LL, Bencsik M, Halloran BP, Bikle DD, et al. PTH differentially regulates expression of RANKL and OPG. J Bone Miner Res 2004;19:235-44. [Google Scholar] [PubMed]
- 8. Nakchbandi IA, Lang R, Kinder B, Insogna KL. The role of the receptor activator of nuclear factor-kappaB ligand/osteoprotegerin cytokine system in primary hyperparathyroidism. J Clin Endocrinol Metab 2008;93:967-73. [Google Scholar] [PubMed]
- 9. Schnoke M, Midura SB, Midura RJ. Parathyroid hormone suppresses osteoblast apoptosis by augmenting DNA repair. Bone 2009;45:590-602. [Google Scholar] [PubMed]
- 10. Bhole R, Flynn JC, Marbury TC. Quadriceps tendon ruptures in uremia. Clin Orthop Relat Res 1985;195:200-6. [Google Scholar] [PubMed]
- 11. Ohishi M, Schipani E. PTH and stem cells. J Endocrinol Invest 2011;34:552-6. [Google Scholar] [PubMed]
- 12. Jones N, Kjellstrand CM. Spontaneous tendon ruptures in patients on chronic dialysis. Am J Kidney Dis 1996;28:861-6. [Google Scholar] [PubMed]
- 13. Basic-Jukic N, Juric I, Racki S, Kes P. Spontaneous tendon ruptures in patients with end-stage renal disease. Kidney Blood Press Res 2009;32:32-6. [Google Scholar] [PubMed]