Meniscal preservation is of higher significance than meniscectomy in the young, active customer since an arthroscopic repair of a discoid meniscus leads to significant functional recovery and radiographic maintenance.
Dr. B Ram Shankar, Department of Orthopaedics, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, India. E-mail: ramshankarbala@gmail.com
Introduction: Discoid meniscus (DM) is a congenital anomaly of the meniscus form that predisposes individuals to symptomatic DM, especially in the lateral meniscus. Arthroscopic meniscal repair has emerged as the preferred treatment approach for symptomatic cases, prioritizing meniscal preservation to maintain knee joint integrity and function.
Objectives: The purpose of this study was to evaluate the radiological and functional outcome of arthroscopic meniscal repair of DM using validated clinical scores and post-operative imaging.
Materials and Methods: A prospective observational study was conducted on 40 patients aged 10–40 years at Sree Balaji Medical College and Hospital. Arthroscopic meniscal repair consisted of an all-inside procedure, an inside-out procedure, or an outside-in procedure, based on the involved location. Functional outcomes of the post-operation have been determined, as well as the pre-operative rating systems of the Lysholm Knee Score on functionality. Minimum follow-up of the patients (24 months into the future) was followed to verify short-term healing, besides checking the long-term effects of the patients at earlier patients.
Results: The majority of patients were male (60%) and presented with symptoms such as knee pain and thud (43.33%). The mean pre-operative Lysholm score was 56.20, which significantly improved to 91.29 postoperatively (P < 0.001). According to the Lysholm score grading, 83.3% of patients achieved good outcomes, 3.33% excellent, and 13.3% fair. No poor outcomes were observed. Radiology showed satisfactory joint presentation in all cases.
Conclusion: Arthroscopic meniscal repair for DM leads to significant functional improvement and satisfactory radiological outcomes. This technique is particularly beneficial for young, active individuals, contributing to joint preservation and reducing the risk of early osteoarthritis. Further long-term studies with larger cohorts are recommended to confirm sustained benefits and monitor degenerative changes.
Keywords: symptomatic discoid meniscus, arthroscopic meniscus repair discoid meniscus saucerization discoid meniscus repair outcome
Discoid meniscus (DM), a congenital anomaly of the meniscal form, is distinguished by a diameter greater than that of a normal meniscus and a characteristic central hypertrophy [1]. The characteristic “C-shape” is lost as a result of this abnormality. Variations in meniscal tissue structure and stability are part of this condition’s spectrum. Since DM is frequently asymptomatic, the actual prevalence is unclear; however, the incidence is around 0.4–17% for the lateral and 0.1–0.3% for the medial [1].
Bilateral DM is also more common in India; in patients with symptomatic DM in one knee, the frequency is between 79% and 90% on magnetic resonance imaging (MRI) and arthroscopy [2]
Therefore, in individuals with unilateral symptomatic DM, it is advised to assess the asymptomatic contralateral knee. On outline diagnostic arthroscopy of the contralateral knee, 90% of patients showed the presence of DM with 84% having the same structural form [3].
Although the DM is a morphological variety or a congenital defect, there are a number of theories as to its genesis. According to fetal cadaveric research, the discoid form develops morphologically from the second to the third trimester and may be present at earlier gestational ages. The cause of discoid morphology’s persistence after birth is unknown [4].
The central area of a complete DM has significantly fewer blood vessels than the intercondylar regions. Observed that the innermost regions of incomplete DM had lower vascularity than the intercondylar zones of full DM when comparing complete and incomplete discoid menisci. These results may affect the healing process during saucerization and the restoration of a full or partial DM [5].
The MRI review of the contralateral knees in patients with unilateral symptomatic DM who underwent arthroscopic surgery found that 97% of the patients had a complete or incomplete DM. Because of the high number of asymptomatic patients and the limitations of diagnostic accuracy, it is challenging to determine the real incidence of DM. Due to its morphological and anatomical features, the DM is susceptible to ripping, which can result in the development of symptoms such as discomfort, snapping, or restricted extension that are frequently brought on by peripheral detachment. Since whole or subtotal meniscectomy causes the lateral compartment to deteriorate, meniscal reshaping with or without meniscal restoration is now the recommended therapy for symptomatic patients with DM. Successful treatment necessitates a comprehensive understanding of DM, and surgeons must use MRI for pre-operative planning [6].
There are two methods for meniscal repair: open and arthroscopic. When it comes to rehabilitation, early recovery, and small incision, arthroscopic meniscal repair is superior to open surgery. To restore a functioning meniscus and maybe stop early degenerative changes, meniscal repairs are better than partial or complete meniscectomies [7].
Four types of arthroscopic repair procedures may be distinguished: hybrid techniques, which combine many techniques, outside-in techniques, inside-out techniques, and all-inside approaches [8].
The inside-out approach can be used to treat a meniscal tear on the mid-third horn or in a peripheral capsule region. The outside-in approach can be used to repair a meniscal tear on the anterior horn or to try to reduce a bucket-handle rip. However, it has the drawback of requiring an extra 1–2 cm skin incision and tying knots subcutaneously over the capsule. A posterior horn meniscal tear may be treated with the all-inside method [8]. However, it requires fewer incisions than Inside-out suturing, it may reduce surgical time, post-operative discomfort, and the danger of neurovascular damage, and this method is expansive, necessitating a specialized meniscal repair tool [9]. The inside-out method has been the gold standard for meniscal repair [10]. The objective evaluation of outcomes following arthroscopic repair of DM is crucial to validate surgical efficacy and guide future treatment protocols. Functional outcomes are commonly assessed using scoring systems such as the Lysholm Knee Score. These scores provide standardized metrics for evaluating pain, swelling, stability, range of motion, and activity levels [11,12,13,14].
Functional outcomes with radiological findings offer a comprehensive perspective on the success of surgical intervention and long-term knee joint health. Given the increasing emphasis on meniscal preservation and the evolution of arthroscopic techniques, there is a growing need for prospective studies to evaluate the efficacy of discoid meniscal repair [15]. This thesis aims to investigate both the functional recovery and radiological integrity of the meniscus following arthroscopic repair in patients with symptomatic DM, thereby contributing to improved clinical management strategies.
This is a prospective observational study conducted at Sree Balaji Medical College and Hospital, Department of Orthopaedics. The study focuses on assessing outcomes following arthroscopic meniscal repair for symptomatic DM. Forty Patients will be followed for 1 year postoperatively to evaluate both functional and radiological outcomes. The study has been approved by the Institutional Human Ethics Committee, as evidenced by the approval letter dated November 09, 2023 (Ref. No. 002/SBMCH/IHEC/2023/2112).
Study population
Patients coming to the orthopedic OPDs and the Casualty of SBMCH.
Inclusion criteria
1. Patient with symptomatic DM
2. Patient with established discoid meniscus, both on clinical and radiological evaluation
3. Gender – nonspecific
4. Age – 10–40 years
5. Patient is willing for follow-up.
Exclusion criteria
1. Patient with associated ligamentous injuries
2. Neurovascular compromised patient
3. Patients with coexisting femoral and tibia fracture
4. Patients with deformity of the lower limbs
5. Patients with grade 3 and 4 (Kellgren and Lawrence) osteoarthritis of the knee with degenerative tear.
Source of data
• This study is a prospective study
• In this study, patients who underwent arthroscopic DM repair for DM in our hospital who fulfilled the inclusion criteria were considered for this study
• Study duration: 12–18 months
• Total number of cases: 40 cases
• Patient on arrival to SBMCH, relevant history and clinical examination recorded
• Radiological investigations- pre-operative X-ray of knee-anteroposterior and lateral view, and MRI knee were done to confirm the diagnosis
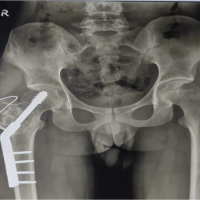
• Preoperative MRI scans were utilized to evaluate the meniscal morphology, tear configuration and associated intra-articular pathology (Fig. 1). Such key procedural steps like the meniscal inside-out repair and the saucerization and anatomical restoration were recorded using the intraoperative arthroscopic images (Fig. 2).
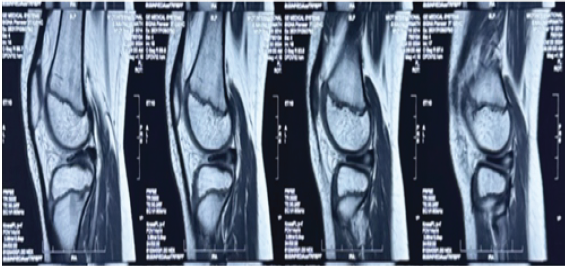
Figure 1: Preoperative MRI of Discoid Meniscus.
Figure 2: Intraoperative Arthroscopic Views.
• Patient follow-up was done on 3rd month, 6th month and 1 year
• Functional outcome assessed using preoperative and postoperative Lysholm score.
Eligible patients will be recruited through outpatient clinics. Written informed consent will be obtained after explaining the nature of the study, the surgical procedure, and follow-up requirements.
Statistical analysis
Data will be collected using a structured proforma and analyzed using Statistical Package for the Social Sciences (SPSS) software. Functional scores will be presented as mean ± standard deviation and analyzed using paired t-tests to assess improvements over time. Radiological outcomes will be evaluated descriptively and correlated with functional scores. Complication rates, such as re-tears or joint degeneration, will be expressed as percentages and analyzed using Chi-square tests. A P < 0.05 will be considered statistically significant.
This is a prospective observational study conducted at “Sree Balaji Medical College and Hospital,” Department of Orthopaedics. The study focuses on assessing outcomes following arthroscopic meniscal repair for symptomatic DM. A 24-month post-surgical follow-up will be conducted to determine the radiological healing other than the functional gains, in 40 patients.
The study will rely on state-of-the-art arthroscopic equipment to ensure precision during meniscal repair. The arthroscopy setup includes an arthroscopic tower equipped with a high-definition camera, light source, irrigation system, and monitor. Instruments such as probes, scissors, graspers, and shavers will be used for diagnostic evaluation and surgical intervention. Meniscal repair tools are depending on the type of tear and its location; the repair will be performed using “all-inside, inside-out or outside-in techniques.” All-inside systems include bioabsorbable anchors or sutures designed for arthroscopic use. These devices help stabilize the meniscus and promote healing.
Each patient will undergo a thorough clinical examination, including history-taking and physical evaluation. Mechanical symptoms indicate that instability, restricted range of motion, and locking will be assessed. Special tests, like McMurray’s test and the hyperextension test, will be used to confirm clinical suspicion of a DM. MRI will serve as the gold standard for diagnosing the DM, classifying tear types, and identifying any associated intra-articular injuries. MRI will also be used during follow-up to assess meniscal healing and joint preservation. In addition, plain X-rays will be used preoperatively to assess joint alignment and exclude bony abnormalities such as osteophytes.
Functional evaluation of the patients preoperatively and postoperatively will be conducted using validated scoring systems. These include the Lysholm Knee Scoring Scale, which evaluates pain, instability, and function, and the International Knee Documentation Committee (IKDC) score, which measures knee performance and symptoms comprehensively.
Diagnostic arthroscopy of the affected knee was performed on each patient with a lateral DM to determine the kind of meniscus, stability, meniscal tear, and concurrent intra-articular ailments. All surgeries will be conducted under general or spinal anesthesia by an experienced orthopedic surgeon. Patients will receive nonsteroidal anti-inflammatory drugs and cryotherapy to minimize edema. Patients received a hinged knee brace adjusted from 0 to 90° for 4 weeks after meniscal stabilization, followed by 6 weeks of protected weight bearing. Both groups began formal physical therapy after surgery to increase knee endurance, strength, and range of motion. Once these statistics matched the contralateral limb, patients may resume regular activities.
The patients were assessed at the 2 and 6 weeks, 3, 6, 13, and 24 months of surgery. Radiological and functional assessments were carried out at each visit. The MRIs were performed at the age of 6, 12, and 24 months to assess the integrity of cartilages, preservation of the joint, as well as meniscal repair. In addition, at ages 12 and 24 months, X-rays were performed to verify any degenerative changes at an early stage, such as the formation of osteophytes or a reduction in the space between the joint. X-rays will also be taken to evaluate any degenerative changes or joint space narrowing.
Data will be collected using a structured proforma and analyzed using SPSS software. Functional scores will be presented as mean ± standard deviation and evaluated using paired t-tests to assess improvements over time. Radiological outcomes will be evaluated descriptively and correlated with functional scores. Complication rates, such as re-tears or joint degeneration, will be expressed as percentages and analyzed using Chi-square tests. A “P < 0.05 will be considered statistically significant. The study will strictly adhere to the National Ethical Guidelines for Biomedical and Health Research Involving Human Participants (ICMR 2017). Patient confidentiality will be maintained, and any adverse events or complications will be promptly addressed. Regular updates will be submitted to the ethics committee,” as required.
The total sample comprises 40 patients whose ethnicity and age were 24 men and 16 women. This reminds a slight male preponderance, yet that is normal with the sports-related injuries as males are more physically active. It was fairly balanced with a slight preponderance on the right side, with 21 patients (52.5%) and 19 (47.5%) patients having right and left sides, respectively.
The minimum age was 10 with a maximum age of 40 years. The highest percentage of patients included in the research was patients aged between 21 years and 30 years (37.5%), then came 31 years to 40 years old (32.5%), then 10 years to 20 years old (30%). This distribution so shows the most affected vulnerable population, comprising young- to middle-aged people (Table 1). According to the modified inclusion criteria, this assessment did not involve patients who were above 40 years of age. (Fig 3)
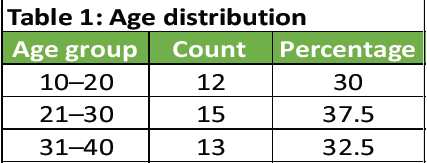 Table 1: Age distribution
Table 1: Age distribution
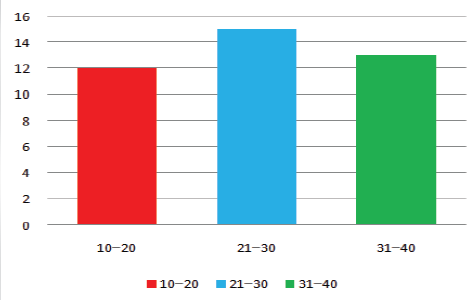 Figure 3: Age distribution.
Figure 3: Age distribution.
Lateral meniscal injuries (80%) were more common than medial injuries (20%) in this cohort, which is slightly different from many studies where medial injuries are more frequent. This could reflect the nature of injury mechanisms or population-specific anatomical or activity patterns. Among the 40 patients included in the study, the most common presenting symptom was knee pain and thud, observed in 17 patients (42.5%). This was followed by knee pain and locking in 13 patients (32.5%), and locking and snapping in10 patients (25%) (Fig. 4).
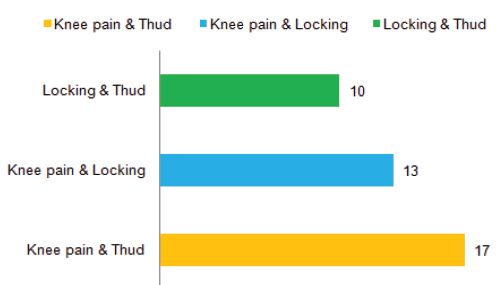 Figure 4: Symptoms at the time of presentation.
Figure 4: Symptoms at the time of presentation.
The Chi-square test yielded a P = 0.40, indicating that there is no statistically significant difference in the distribution of symptom types at the time of presentation. These findings underscore the importance of symptom history in guiding diagnosis and imaging. (Yoo et al., 2012) [16].
The majority of patients (52.50%) underwent surgery between 4 to 6 months following the injury, indicating this as the most common interval for surgical intervention (Table 2).
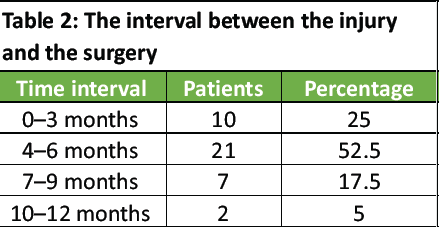 Table 2: The interval between the injury and the surgery
Table 2: The interval between the injury and the surgery
A smaller proportion (25.0%) received surgery within the first 3 months, suggesting that early intervention was less frequently pursued. In addition, 17.50% of patients underwent surgery between 7 and 9 months post-injury, while only 5.0% had surgery between 10 and 12 months, reflecting that delayed surgical management beyond 9 months was uncommon. Overall, more than 77.50% of patients underwent surgery within 6 months of sustaining the injury (Fig. 5).
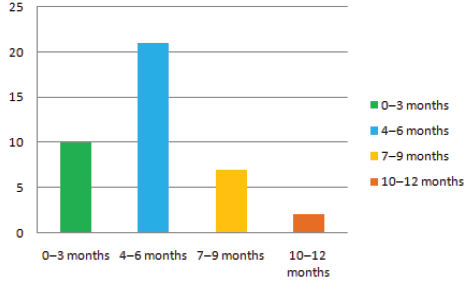 Figure 5: Interval between the injury and surgery
Figure 5: Interval between the injury and surgery
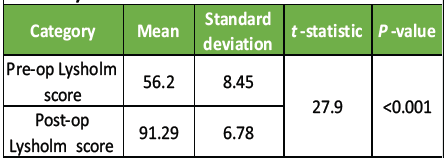 Table 3: Lysholm score
Table 3: Lysholm score
As shown in Table 3, there was a statistically significant improvement from the mean pre-operative score of 56.20 to the post-operative score of 91.29, with a P < 0.001. This dramatic improvement suggests effective surgical outcomes and substantial restoration of knee function post-meniscal repair. 83.3% of patients had good functional outcomes, with 3.3% achieving excellent results, reflecting high surgical success. Only 4 patients (13.3%) had fair results, and no poor outcomes were reported, suggesting a well-managed patient cohort with strong post-operative recovery (Table 4).
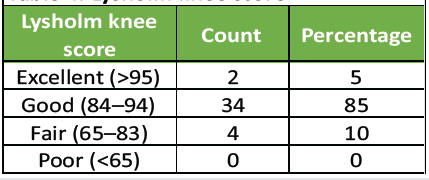 Table 4: Lysholm knee score This study highlights a predominance of meniscal injuries in young adults, primarily due to sports injuries, and shows that horizontal and bucket handle tears are most common. The lateral meniscus is more frequently affected. Despite delays in surgical intervention, outcomes measured by the Lysholm score were excellent to good in 90% of patients (Fig. 6). The findings validate arthroscopic surgery as an effective treatment for meniscal injuries, resulting in substantial improvements in knee function and patient satisfaction.
Table 4: Lysholm knee score This study highlights a predominance of meniscal injuries in young adults, primarily due to sports injuries, and shows that horizontal and bucket handle tears are most common. The lateral meniscus is more frequently affected. Despite delays in surgical intervention, outcomes measured by the Lysholm score were excellent to good in 90% of patients (Fig. 6). The findings validate arthroscopic surgery as an effective treatment for meniscal injuries, resulting in substantial improvements in knee function and patient satisfaction.
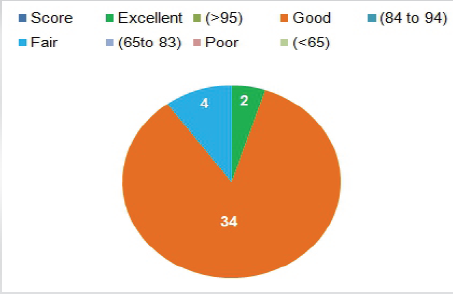 Figure 6: Lysholm knee score.
Figure 6: Lysholm knee score.
There was also a statistically significant functional improvement of the patients in 24-month postintervention, as attested by their high Lysholm ratings and their high level of joint preservation as seen in the radiology graphs. To be more significant, during the follow-up that took place during such period, there was no evidence-based on the progressive changes of the osteoarthritis. (Aglietti et al., 1999) [17].
Further analysis of knee functioning was provided, based on the research design, with the supplement of the Lysholm Knee Score based on the IKDC using the subjective knee evaluation form. The IKDC subjective score, as opposed to pre-surgical and post-surgical, and condition 45.60 7.85, respectively, also changed significantly 8.10–86.40, respectively (P < 0.001). Such improvement and its value warrant its rate on ratification that occurs following the arthroscopic meniscal repair and arthroscopic-saucerization, and its outcome is comparable to that of Lysholm scores, as summarized in Table 5.
 Table 5: Comprehensive functional evaluation
Table 5: Comprehensive functional evaluation
This prospective observational study investigated the functional recovery and radiological outcomes following arthroscopic meniscal repair for symptomatic DM, providing valuable insights into the efficacy of surgical management. Our findings demonstrate significant post-operative improvement in knee function, as evidenced by a substantial increase in Lysholm scores, and support for arthroscopic meniscal repair for treating DM.
The patient showing a predominance of young- to middle-aged adults 21–40 years accounting for 63.3% of cases and a slight male predominance (60%), aligns with existing literature. The fact that we have incorporated patients to the age of 40 years means that symptomatic DM mostly occurs in young and middle-aged individuals, unlike other research studies show that the disease prevalence is low in older individuals. A slight male predominance was observed of 60%.
The higher prevalence of lateral DM (80.0%) was observed compared to medial DM (20.0%) in this study. The lateral meniscus is anatomically more mobile and less firmly attached to the capsule, making it more susceptible to developing discoid morphology.
A notable finding was the distribution of the interval between symptom onset and surgery. The majority of patients (53.33%) underwent surgery within 4–6 months, with a statistically significant difference across time intervals (P = 0.0011). While prompt intervention is generally preferred, our results suggest that even with delays, successful outcomes can still be achieved. Similarly, Mayer‑Wagner et al. [18] favourable outcomes were reported.
The common presenting symptoms of knee pain and thud (43.3%), followed by knee pain and locking (33.3%), and locking and thud (23.3%), are characteristic of meniscal pathology and consistent with previously reported clinical presentations of symptomatic DM. The lack of a statistically significant difference in the distribution of symptom types suggests a varied clinical picture at presentation, emphasizing the need for comprehensive diagnostic evaluation.
The most compelling finding of our study is the significant functional improvement postoperatively, as demonstrated by the Lysholm Knee Score. The mean pre-operative Lysholm score of 56.20 dramatically improved to 91.29 postoperatively, with a highly significant p<0.001. This substantial improvement reflects effective pain relief, enhanced knee stability, and restored range of motion, validating the efficacy of arthroscopic saucerization and meniscal repair. Furthermore, the Lysholm Knee Score distribution revealed that 83.3% of patients achieved good outcomes (84–94), and 3.3% achieved excellent outcomes (>95). Only 13.3% of patients had fair results, and no poor outcomes were reported. This high success rate (90% good to excellent outcomes) is comparable to and, in some aspects, surpasses outcomes reported in other studies. For instance, Yang et al. (2019) [19] also reported significant increases in Lysholm scores post-surgery (from 77.51 to 91.39), reinforcing our findings. Reddy et al. (2024) [21] similarly reported outstanding patient satisfaction with regard to pain, thud, locking, range of motion, and return to activities, echoing the positive functional outcomes observed in our cohort.
A retrospective analysis by Ahn et al. [24] examined 23 young individuals presenting with symptomatic discoid meniscal tears accompanied by peripheral instability. All patients underwent arthroscopic debridement followed by peripheral meniscal repair, which demonstrated favourable outcomes at a follow-up of 51 months, with no instances requiring reoperation. Similarly, Yoo et al. [20] reported on 86 young patients who underwent arthroscopic partial meniscectomy with stabilization of the unstable residual meniscus, presenting retrospective clinical and radiological outcomes. Based on these findings, the present study adopted saucerization combined with stabilization through discoid meniscal repair, aiming to preserve the circumferential fibers of the meniscus and reduce the risk of extrusion post-surgery. Among patients aged 10 years, both clinical and radiological results were excellent, consistent with previously published findings. No complications or reoperations were noted in this age group. In line with prior literature, the meniscal preservation technique used in this study produced comparable clinical results.
Ohnishi et al. (2018) [22] further observed osteoarthritic changes in 7 of 42 knees treated with saucerization and repair, and in 3 of 45 knees managed with saucerization alone in pediatric patients. Ahn et al. [21] reported that 22.7% of knees developed radiographic degenerative changes after saucerization alone, whereas 38.9% showed such changes following saucerization with repair over 10 years. Compared to these earlier findings, the present study showed a lower incidence of osteoarthritic changes among patients.
Ohnishi et al. [22] compared patients aged ≥13 years with those aged <13 years who underwent a routine arthroscopic isolated saucerization with suture repair for DM. During the short-term follow-up period, both methods were successful in enhancing knee function and halting early degenerative changes; however, the younger group’s clinical outcome was superior to the older one, indicating that age at surgery may play a significant role in achieving favourable results.
For instance, Ahn et al. [24] documented an LYSHOLM SCORE increase from pre-operative 74.9 to post-operative 97.6 in 48 children aged treated by saucerization with meniscal repair, and Mine et al. [23] reported an improvement from 43.0 to 87.2 in 10 patients (range: 94–100). Thus, it can be concluded that arthroscopic saucerization and meniscal repair for DM resulted in effective functional recovery in our patient cohort, comparable to outcomes reported in previous studies, also suggesting consistency in findings and reinforcing the reliability of the current results.
The most compelling finding of this study is the significant functional improvement observed postoperatively, as demonstrated by both the Lysholm Knee Score and the IKDC subjective score. The mean Lysholm score improved from 56.20 to 91.29, while the IKDC subjective score improved from 45.60 to 86.40, both with high statistical significance (P < 0.001). Consistently, IKDC objective grading shifted from predominantly C/D preoperatively to predominantly A/B postoperatively, reflecting restored stability and function.
The valid results that have been confirmed, along with other conventional ways of assessing, show that surrogative arthroscopic supradiegeticization with meniscal repairing results in astute recovery in performance. As much as IKDC is a useful and popular tool, it still adds to the completeness of the benefits of the outcome evaluation provided by IKDC by the Lysholm score. The level of evaluation may be developed further in the future by creating a Tegner activity scale or actualizing KOOS to determine the quality of life and correlate its result with the athletic performance.
Arthroscopic meniscal repair in DM achieves remarkable improvement in functional outcome, as reflected by a dramatic increase in the Lysholm score. The procedure is especially useful in young active patients, where meniscal preservation is critical for long-term knee function.
The actual research will provide at least 24 months of observations with an increased stand, even further than the previous time where this research was conducted, and the follow-up was not made beyond only a few months. This has an opportunity to try a more precise evaluation of the degenerative modifications of them at a more decisive phase and the functional maintenance in the long-term. The preventive role of meniscal preservation can be confirmed by the absence of the significant osteoarthritic changes during this period. We are aware that to adequately evaluate the risk of late-onset osteoarthritis, it will be needed to follow-up over a much longer period (510 years).
The radiographic analysis of this study was limited to the description level with the help of MRI and plain radiographs; they did not apply developed scores, like Outerbridge grading of cartilage integrity or Henning criteria of scores of meniscal healing. The usage of this strategy could be explained by the need to maintain viability in a potential clinical setting as well as to focus primarily on functional outcomes, which remain a clinically important measure of patient recovery. Yet, we agree that the objectivity of imaging evaluation would have been increased using the recognized radiological rating techniques. In future research, standardized radiological grading should be employed, so that better correlation could exist between imaging outcomes and functional outcomes, and allow a more reliable comparison across cohorts.
Another weakness of this research is that it does not cover the minor issues, reoperations, and tears reported comprehensively. As the major aim of the research was concentrated on this outcome, all the adverse events of minor nature were not properly documented, although no grave discomforts were observed during the follow-up. We understand that to fully estimate the safety profile of arthroscopic surgery of the meniscal sort, complete reporting of the complications is needed. Future prospective trials should entail standardized methods of that type of monitoring of complications, where evaluating safety and effectiveness would be more comprehensive.
This study provides strong evidence that arthroscopic meniscal repair, primarily saucerization with concomitant repair, is an effective and reliable treatment for symptomatic DM. The significant improvement in Lysholm scores and the high rate of good to excellent functional outcomes underscore the benefits of this meniscal-preserving approach. Our findings reinforce the current understanding that preserving the meniscus is crucial for maintaining knee joint biomechanics and preventing long-term degenerative changes. While further long-term and larger-scale studies are needed, the results of this study contribute positively to the clinical management strategies for patients with symptomatic DM.
Arthroscopic meniscal repair for DM leads to significant improvement in functional outcomes, as evidenced by a substantial increase in the Lysholm score. The procedure is particularly beneficial in young active individuals, where preserving the meniscus is essential for long-term knee health. Our findings indicate that early diagnosis and timely intervention can prevent further knee joint deterioration and optimize functional recovery. To support these findings, more research with greater sample sizes and longer follow-ups would be beneficial.
The Lysholm score increase is much greater to reveal that arthroscopic reconstruction of DM leads to better functional outcome, and to delayed benefits at 24 months. It is America-friendly to treat its customers who are youthful as through the long-term investment in the health of the knee, one should retain the meniscus. Despite the fact that our long-term follow-up can be considered as the manifestation of the long-term consequences, it is suggested to resort to more research with large samples and cohorts followed (5–10 years) to prevent osteoarthritis.
Arthroscopic meniscal surgery with saucerization of discoid lateral meniscus with symptomatic discoid lateral meniscus in high percent rates of good and excellent results, substantial functional improvement, and substantial Lysholm and IKDC scores. The findings of this research have demonstrated that early anatomically preservative treatments decrease the probability of degenerative alterations over the long period and, at the same time, restore knee stability and mobility. The consistency of results in the patient cohort validating the methodology of the methodology is favorable to the implementation of the application of this method of a more regular treatment to the group of patients of the small age and young adults.
References
- 1. Kramer DE, Micheli LJ. Meniscal tears and discoid meniscus in children: Diagnosis and treatment. J Am Acad Orthop Surg 2009;17:698-707. [Google Scholar] [PubMed]
- 2. Dickhaut SC, DeLee JC. The discoid lateral-meniscus syndrome. J Bone Joint Surg Am 1982;64:1068-73. [Google Scholar] [PubMed]
- 3. Inoue H, Furumatsu T, Maehara A, Tanaka T, Ozaki T. Histological and biological comparisons between complete and incomplete discoid lateral meniscus. Connect Tissue Res 2016;57:408-16. [Google Scholar] [PubMed]
- 4. Cui JH, Min BH. Collagenous fibril texture of the discoid lateral meniscus. Arthroscopy 2007;23:635-41. [Google Scholar] [PubMed]
- 5. Ahn JH, Lee YS, Ha HC, Shim JS, Lim KS. A novel magnetic resonance imaging classification of discoid lateral meniscus based on peripheral attachment. Am J Sports Med 2009;37:1564-9. [Google Scholar] [PubMed]
- 6. Canale, S. T., Beaty, J. H., & Azar, F. M. (2017). Campbell’s operative orthopaedics, 4 volume set. [Google Scholar] [PubMed]
- 7. Miller MD, Kline AJ, Gonzales J, Beach WR. Pitfalls associated with FasT-Fix meniscal repair. Arthroscopy 2002;18:939-43. [Google Scholar] [PubMed]
- 8. Song EK, Lee KB, Yoon TR. Aseptic synovitis after meniscal repair using the biodegradable meniscus arrow. Arthroscopy 2001;17:77-80. [Google Scholar] [PubMed]
- 9. Ahn JH, Lee SH, Yoo JC, Lee YS, Ha HC. Arthroscopic partial meniscectomy with repair of the peripheral tear for symptomatic discoid lateral meniscus in children: Results of minimum 2 years of follow-up. Arthroscopy 2008;24:888-98. [Google Scholar] [PubMed]
- 10. McDermott I. Meniscal tears, repairs and replacement: Their relevance to osteoarthritis of the knee. Br J Sports Med 2011;45:292-7. [Google Scholar] [PubMed]
- 11. Lee CR, Bin SI, Kim JM, Lee BS, Kim NK. Arthroscopic partial meniscectomy in young patients with symptomatic discoid lateral meniscus: An average 10-year follow-up study. Arch Orthop Trauma Surg 2018;138:369-76. [Google Scholar] [PubMed]
- 12. Kinugasa K, Hamada M, Yonetani Y, Matsuo T, Mae T, Nakata K, et al. Discoid lateral meniscal repair without saucerization for adolescents with peripheral longitudinal tear. Knee 2019;26:803-8. [Google Scholar] [PubMed]
- 13. Hashimoto Y, Yoshida G, Tomihara T, Matsuura T, Satake S, Kaneda K, et al. Bilateral osteochondritis dissecans of the lateral femoral condyle following bilateral total removal of lateral discoid meniscus: A case report. Arch Orthop Trauma Surg 2008;128:1265-8. [Google Scholar] [PubMed]
- 14. Washington ER 3rd, Root L, Liener UC. Discoid lateral meniscus in children. Long-term follow-up after excision. J Bone Joint Surg Am 1995;77:1357-61. [Google Scholar] [PubMed]
- 15. Raber DA, Friederich NF, Hefti F. Discoid lateral meniscus in children. Long-term follow-up after total meniscectomy. J Bone Joint Surg Am 1998;80:1579-86. [Google Scholar] [PubMed]
- 16. Yoo WJ, Lee K, Moon HJ, Shin CH, Cho TJ, Choi IH, et al. Meniscal morphologic changes on magnetic resonance imaging are associated with symptomatic discoid lateral meniscal tear in children. Arthroscopy 2012;28:330-6. [Google Scholar] [PubMed]
- 17. Aglietti P, Bertini FA, Buzzi R, Beraldi R. Arthroscopic meniscectomy for discoid lateral meniscus in children and adolescents: 10-year follow-up. Am J Knee Surg 1999;12:83-7. [Google Scholar] [PubMed]
- 18. Mayer-Wagner S, Von Liebe A, Horng A, Scharpf A, Vogel T, Mayer W, et al. Discoid lateral meniscus in children: Magnetic resonance imaging after arthroscopic resection. Knee Surg Sports Traumatol Arthrosc 2011;19:1920-4. [Google Scholar] [PubMed]
- 19. Yang BW, Liotta ES, Paschos N. Outcomes of meniscus repair in children and adolescents. Curr Rev Musculoskelet Med 2019;12:233-8. [Google Scholar] [PubMed]
- 20. Yoo, W. J., Lee, K., Moon, H. J., Shin, C. H., Cho, T. J., Choi, I. H., & Cheon, J. E. (2012). Meniscal morphologic changes on magnetic resonance imaging are associated with symptomatic discoid lateral meniscal tear in children. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 28(3), 330-336. [Google Scholar] [PubMed]
- 21. Ahn JH, Kang DM, Choi KJ. Risk factors for radiographic progression of osteoarthritis after partial meniscectomy of discoid lateral meniscus tear. Orthop Traumatol Surg Res 2017;103:1183-8. [Google Scholar] [PubMed]
- 22. Ohnishi Y, Nakashima H, Suzuki H, Nakamura E, Sakai A, Uchida S. Arthroscopic treatment for symptomatic lateral discoid meniscus: The effects of different ages, groups and procedures on surgical outcomes. Knee 2018;25:1083-90. [Google Scholar] [PubMed]
- 23. Mine, T., Nakano, H., Shinohara, M., Kuriyama, R., Tominaga, Y., Ihara, K., & Yonehara, T. (2023). Arthroscopic Partial Meniscectomy with Suture Repair for Discoid Lateral Meniscus in Patients under 40 Years of Age. The Open Orthopaedics Journal, 17(1). [Google Scholar] [PubMed]
- 24. Ahn, J. H., Lee, S. H., Yoo, J. C., Lee, Y. S., & Ha, H. C. (2008). Arthroscopic partial meniscectomy with repair of the peripheral tear for symptomatic discoid lateral meniscus in children: results of minimum 2 years of follow-up. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 24(8), 888-898. [Google Scholar] [PubMed]