For isolated pisiform fractures with tiny proximal fragments, a contoured hook plate enables stable, fragment-preserving fixation with excellent functional outcomes, providing an effective alternative to fragment excision.
Dr. Ikuo Nakai, Department of Orthopedic Surgery, Nishi Omiya Hospital, Saitama, Japan. E-mail: nykkuo@gmail.com
Introduction: The report describes hook plate fixation for an isolated, displaced pisiform fracture characterized by a small proximal fragment.
Case Report: A 64-year-old woman presented with ulnar-sided wrist pain after a fall. Radiography and computed tomography revealed intra-articular displacement with mild comminution. Open reduction and internal fixation using a 1.2-mm hook plate resulted in a stable anatomical reduction without the need for fragment excision. Postoperatively, the wrist was immobilized in a volar splint in neutral position for 3 weeks, after which progressive mobilization was initiated. At 12-month follow-up, the patient was pain-free with wrist extension of 85° and flexion of 75°. Grip strength was 29.6 kg on the operated side, while 24.3 kg on the contralateral side. Patient-reported outcomes were excellent, indicating satisfactory functional recovery and pain relief. Radiographs confirmed bone union and anatomical alignment, with no evidence of pisotriquetral degenerative changes.
Conclusion: Hook plate fixation may represent a feasible joint-preserving alternative for select comminuted pisiform fractures with small fragments, offering stable fixation and enabling relatively early rehabilitation.
Keywords: Pisiform bone, carpal bones, isolated pisiform fracture, fracture fixation, bone plates.
Isolated fractures of the pisiform are rare, accounting for 0.2–2.0% of all carpal bone fractures [1,2]. These fractures typically result from direct trauma or repetitive microtrauma and, if missed or inadequately t Conservative management with immobilization is generally preferred for nondisplaced fractures [3,4,5]. Surgical intervention is indicated in the presence of comminution, displacement, articular incongruity, or persistent pain following conservative treatment [1]. Previously reported surgical approaches include open reduction and internal fixation (ORIF) using Kirschner wires or cortical screws [6,7,8], as well as pisiform excision in cases of irreparable fractures [9,10]. Internal fixation is technically challenging owing to the pisiform’s small size and potential instability of fracture fragments, and reported outcomes are largely limited to isolated case reports and small case series [1]. Surgical approaches for pisiform injuries typically involve the use of Kirschner wires, screws, or excision; descriptions of mini-plate or hook plate fixation are rare [6,7,8]. We present a case of a displaced, comminuted pisiform fracture with a small proximal fragment that was successfully treated with hook plate fixation, highlighting the technical feasibility and functional outcomes.
A 64-year-old right-handed woman presented with the sudden onset of severe right wrist pain sustained after a fall. Physical examination demonstrated swelling and tenderness along the ulnar aspect of the volar wrist. Plain radiographs and computed tomography (CT) scans revealed a comminuted intra-articular pisiform fracture featuring a small proximal fragment and articular incongruity with a cortical gap and a step-off (Fig. 1 and 2).
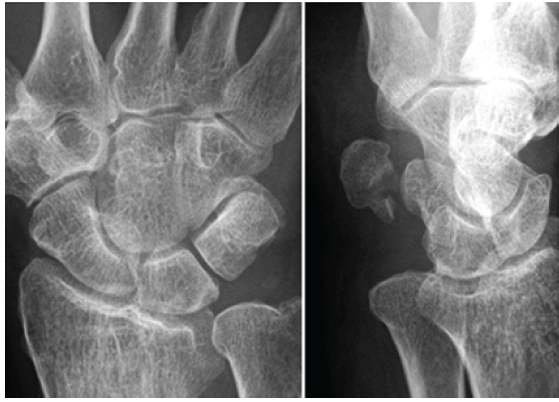
Figure 1: Initial plain radiographs demonstrate an isolated displaced intra-articular pisiform fracture with pisotriquetral joint incongruity.
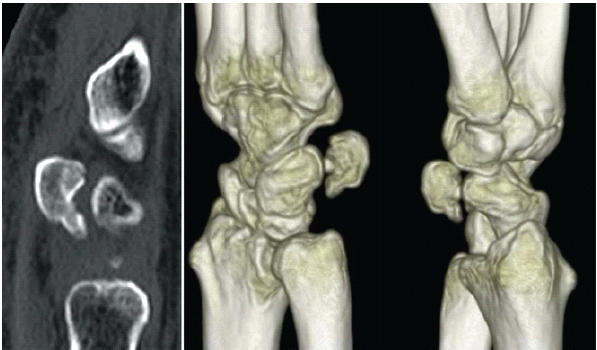
Figure 2: Computed tomography displays a small proximal fragment (3.7 mm) comminution, and pisotriquetral joint incongruity characterized by a cortical gap and a set-off.
Sagittal CT reconstruction confirmed that the fragment measured 3.7 mm in size (DICOM viewer, Horos Project). Pre-operative planning indicated that stable fixation with screws or wires was technically unfeasible due to the small fragment size and poor bone stock. Given the displacement, articular incongruity, and instability, non-operative management was considered unlikely to restore anatomical alignment or bone union. Pisiform excision was considered but deferred as no degenerative changes in the pisotriquetral joint were evident, and joint preservation was preferred. Moreover, ORIF with hook plate fixation was selected, and surgery was performed 8 days post-injury.
Surgical technique
The procedure was performed under axillary block anesthesia with the patient in the supine position, and a pneumatic tourniquet was applied to the arm. A zigzag incision was made over the pisiform to expose the fracture site. The flexor carpi ulnaris (FCU) tendon was retracted radially to expose the fracture site. The site was debrided, and the proximal fragment was carefully mobilized using forceps. The distal impacted fragment was reduced under fluoroscopic guidance to restore joint alignment, and the proximally retracted fragment was repositioned anatomically to complete the reduction. For temporary stabilization, a 0.7-mm Kirschner wire was inserted distally into the proximal fragment. On inspection, the proximal fragment was deemed too small for definitive screw or wire fixation, consistent with the pre-operative assessment. Consequently, hook plate fixation was performed as planned. A 1.2-mm hook plate (APTUS Hand System; Medartis AG, Basel, Switzerland) was applied, with the hook engaging the proximal aspect of the pisiform. Interfragmentary compression was achieved by pulling the plate distally, followed by insertion of a cortical screw into the distal fragment to complete fixation (Fig. 3).

Figure 3: Intraoperative fluoroscopic image after hook plate fixation illustrates reduction and plate compression across the fracture, with the hook engaging the proximal aspect of the pisiform.
This construct provided stable fixation with interfragmentary compression, eliminating the need for direct fixation of the proximal fragment. The wound was closed in layers. Postoperatively, a volar forearm splint was applied with the wrist in a neutral position and maintained for 3 weeks.
Postoperative course and imaging
The post-operative course was uneventful. Active range-of-motion (ROM) exercises were initiated after the splint was removed. At 3 months, plain radiographs confirmed bone union, and the patient had resumed daily and social activities without restriction. At 12 months (Figs. 4 and 5), she reported no wrist pain and had returned to normal activities without limitations.
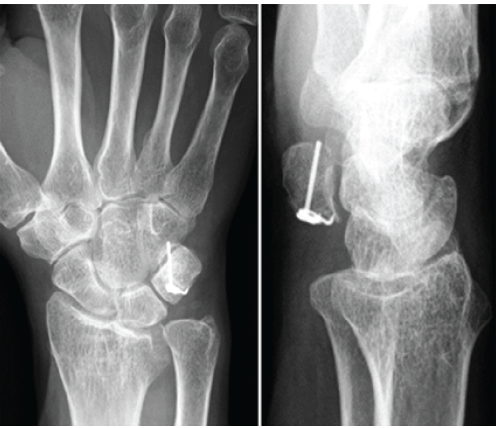
Figure 4: Radiographs at the 12-month follow-up demonstrate bone union with proper anatomical alignment and no pisotriquetral degenerative changes.

Figure 5: Clinical photographs obtained at 12 months demonstrate wrist extension (85°), wrist flexion (75°), and full forearm rotation (pronation and supination).
Radiographs demonstrated complete union and proper alignment. The implant remained well-positioned, with no sign of loosening or migration, and no degenerative changes were observed in the pisotriquetral joint.
Clinical outcomes
At 12 months, examination demonstrated a wrist ROM of 85° in extension and 75° in flexion. Grip strength measured 29.6 kg on the affected right side and 24.3 kg on the contralateral side. No infection, FCU dysfunction, pisotriquetral instability, or ulnar nerve irritation was observed. The patient-reported outcomes were favorable, with a quick disabilities of the arm, shoulder, and hand score of 2.2, hand 20 score of 0.5, and a Modified Mayo Wrist Score of 100 (excellent).
Isolated pisiform fractures are rare, representing <2% of carpal fractures, and are frequently missed due to subtle clinical signs and radiographic findings [1,2]. Conservative treatment is generally favored in nondisplaced cases; however, no clear consensus is available on the optimal surgical management of displaced or comminuted fractures [1,5]. In the present case, a comminuted displaced pisiform fracture with a small proximal fragment (3.7 mm) posed significant challenges for standard internal fixation. The fragment’s small size and bone stock reduced the feasibility of screw or wire fixation. Therefore, the hook plate fixation – a method seldom reported for pisiform fractures – was employed to achieve anatomical reduction and stable fixation [6,8]. This construct stabilized the small proximal fragment without direct screw fixation, preserving both fragment integrity and pisotriquetral joint congruity. Screw fixation can be technically demanding and may be infeasible in cases of severe comminution. In contrast, a hook plate offers reliable stabilization and interfragmentary compression by engaging the proximal fragment without requiring direct screw fixation. The design allows for distal traction during fixation, facilitates fragment apposition, and supports relatively early mobilization. In this case, immobilization was limited to 3 weeks, after which active ROM exercises were initiated; this approach may help reduce the risk of joint stiffness, particularly in older patients. Previous reports suggest that pisiform excision can yield favorable outcomes in comminuted fractures; however, these conclusions are based on limited case series and case reports and do not reflect contemporary fixation methods, including hook plates [9,10]. In the present case, when anatomical alignment of the articular surface could be restored and no degenerative change was present, preserving the fragment with fixation was deemed preferable to excision [6,8]. Excision is effective in some contexts but may alter wrist biomechanics by disrupting the FCU insertion and the pisotriquetral articulation [9,10]. Preserving the pisiform may help maintain grip strength and dynamic pisotriquetral joint stability, which is especially important for patients who are active or have physically demanding jobs [6,8]. In contrast, excision carries recognized risks, including ulnar nerve irritation, FCU dysfunction, and pisotriquetral instability [9,10]. Previous reports have discussed surgical fixation using Kirschner wires or cortical screws for larger or non-comminuted fragments [1,6,7]. To our knowledge, reports describing hook plate fixation of isolated pisiform fractures are rare. Our case demonstrates that hook plate fixation can be a practical, joint-preserving option when the proximal fragment is too small for screw or wire fixation and preservation of the fragment is desired. Management should be tailored to the fracture morphology, patient activity level, and anatomical considerations. Hook plate fixation may expand the range of salvageable pisiform fractures and offer an alternative to excision in technically challenging cases [6,8]. This report is limited by its single-case design, 12-month follow-up, and lack of direct comparison with other techniques. Therefore, the findings should be interpreted with caution and may not be generalizable to all patients. Further studies are needed to assess long-term outcomes, determine optimal indications, and evaluate the effectiveness of this approach compared to conservative management and excision.
Hook plate fixation may be a feasible, joint-preserving option for isolated pisiform fractures when the proximal fragment is too small for conventional screw or wire fixation, allowing stable reduction while maintaining pisiform integrity.
Isolated pisiform fractures with very small proximal fragments are difficult to fix using K-wires or screws and are often managed by fragment excision. This case report demonstrates that a contoured hook plate can provide stable fixation while preserving the pisotriquetral joint, enabling early rehabilitation and excellent functional recovery. Surgeons should consider this technique when preservation of the fracture fragment is desirable.
References
- 1. Suh N, Ek ET, Wolfe SW. Carpal fractures. J Hand Surg Am 2014;39:785-91. [Google Scholar] [PubMed]
- 2. Raghupathi AK, Kumar P. Nonscaphoid carpal injuries – incidence and associated injuries. J Orthop 2014;11:91-5. [Google Scholar] [PubMed]
- 3. Kalaria GP, Vora PH, Memon RR. An isolated pisiform fracture: A case report. Int J Res Orthop 2018;4:173-5. [Google Scholar] [PubMed]
- 4. Verma V, Singh A, Kumar S, Singh MP. Isolated fracture of the pisiform: Case report of a rare injury of the wrist. Int J Med Update 2016;11:19-21. [Google Scholar] [PubMed]
- 5. Amer AF, Alrehaili TM, Alrehailiy MM. Isolated non-displaced pisiform fracture: A diagnostic challenge in ulnar-sided wrist trauma managed conservatively. Cureus 2025;17:e87637. [Google Scholar] [PubMed]
- 6. Agathangelidis F, Boutsiadis A, Ditsios K. Open pisiform fracture: Excision or internal fixation? BMJ Case Rep 2013;2013:bcr2012007621. [Google Scholar] [PubMed]
- 7. Super JT, Morris JA, Anakwe RE. Joystick reduction and percutaneous kirschner wire stabilisation for dislocation of the pisiform. J Clin Orthop Trauma 2020;11:694-6. [Google Scholar] [PubMed]
- 8. Letsch MT, De Boer HL, Nguyen DT. Open reduction of the dislocated pisiform bone. J Hand Microsurg 2016;8:183-4. [Google Scholar] [PubMed]
- 9. Peters MJ, Mazor A, Glaris Z, Goetz TJ. Patient satisfaction with pisiform excision for pisotriquetral instability or arthritis: A prospective review. J Wrist Surg 2023;12:331-6. [Google Scholar] [PubMed]
- 10. Van Eijzeren J, Karthaus RP. The effect of pisiform excision on wrist function. J Hand Surg Am 2014;39:1258-63. [Google Scholar] [PubMed]